Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (30): 4782-4788.doi: 10.3969/j.issn.2095-4344.2823
Previous Articles Next Articles
Analysis and prediction of related factors of single-level cervical total disc replacement
He Li1, Xu Shuai2, Xu Song1, Zhao Xiaoyu1, Pang Shilong1, Miao Jun3, Liu Haiying2, Liang Yan2
- 1Tianjin Ninghe Hospital, Tianjin 301500, China; 2Department of Spine Surgery, Peking University People’s Hospital, Beijing 100044, China; 3Department of Spine Surgery, Tianjin Hospital, Tianjin 300210, China
-
Received:2020-01-09Revised:2020-01-14Accepted:2020-03-11Online:2020-10-28Published:2020-09-18 -
Contact:Liu Haiying, Chief physician, Professor, Doctoral supervisor, Department of Spine Surgery, Peking University People’s Hospital, Beijing 100044, China Liang Yan, Attending physician, MD, Department of Spine Surgery, Peking University People’s Hospital, Beijing 100044, China -
About author:He Li, Master, Associate chief physician, Tianjin Ninghe Hospital, Tianjin 301500, China -
Supported by:the National Natural Science Foundation of China, No. 81472140; the Research and Development Fund of Peking University People’s Hospital, No. RDD2016-02
CLC Number:
Cite this article
He Li, Xu Shuai, Xu Song, Zhao Xiaoyu, Pang Shilong, Miao Jun, Liu Haiying, Liang Yan. Analysis and prediction of related factors of single-level cervical total disc replacement[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(30): 4782-4788.
share this article

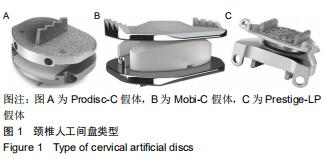
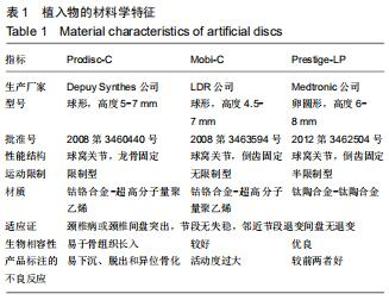
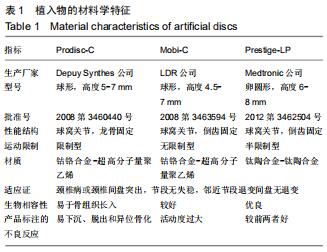
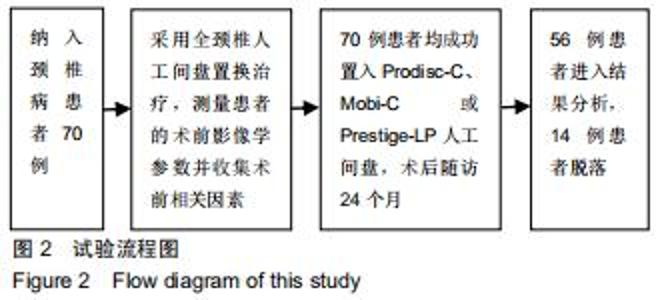
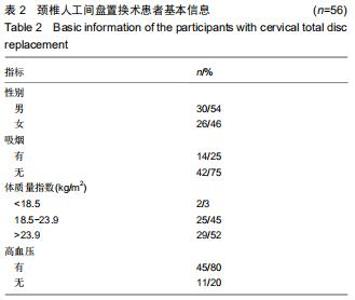
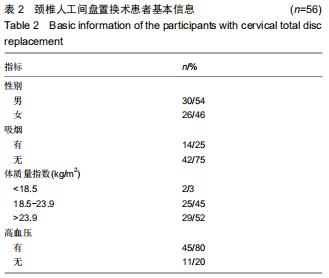
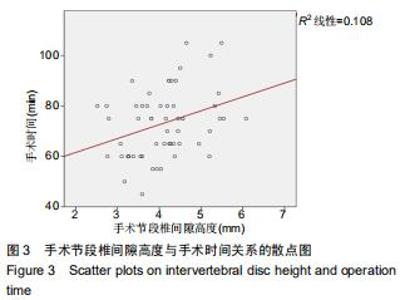
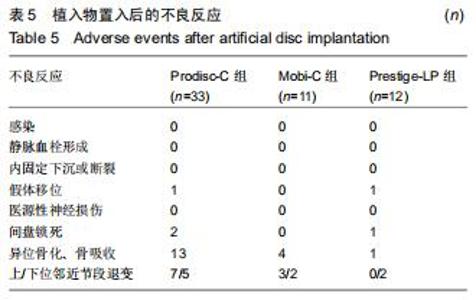
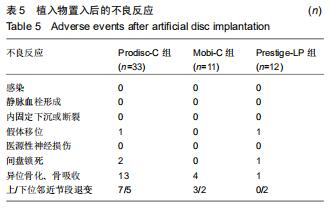
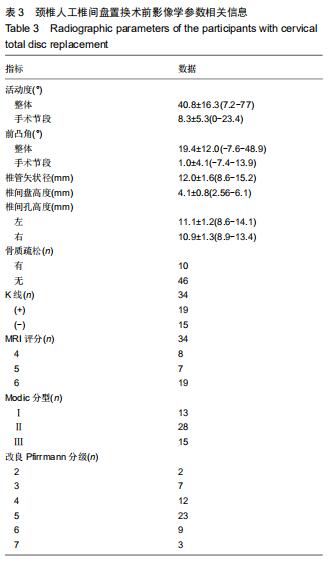
2.5 次要结果 手术节段最常见的为C5/6(40例),其余依次为C4/5,C6/7和C3/4;颈椎病最常见的为混合型(28例)和神经根型颈椎病(18例);颈椎人工间盘Prodisc-C假体33例,Mobi-C假体12例和Prestige-LP假体11例;术前38例行保守治疗。术前活动度、颈椎前凸角等影像学参数具体信息见表3。其中骨质疏松患者10例;根据颈椎MRI测得K线(+)者为56%,MRI评分分别为4分(23%)、5分(21%)和6分(56%);终板Modic分型最常见为Ⅱ型(28例);改良Pfirrmann分级中最常见的为5级(41%)和4级(21%)。而术前56例患者平均ODI为48.2±9.8,日本骨科学会评分为(11.1±3.0)分,目测类比评分为(5.8±2.6)分。 "
|
[1] NUNLEY PD, CORIC D, FRANK KA, et al. Cervical disc arthroplasty: current evidence and real-world application. Neurosurgery. 2018;83(6):1087-1106.
[2] YANG Y, SHI B, DUAN Y, et al. Anatomic morphology and clinical significance of intraforaminal ligaments of the cervical spine. Clin Anat. 2019;32(5):654-660.
[3] 袁野,郭晓丹,姜里强,等.颈胸段脊柱手术前方入路的应用解剖[J].解剖学杂志,2017,40(4):453-455.
[4] RYU JI, HAN MH, KIM JM, et al. Cervical epidural hematoma that induced sudden paraparesis after cervical spine massage: case report and literature review. World Neurosurg. 2018;112:217-220.
[5] RADCLIFF K, ONG KL, LOVALD S, et al. Cervical Spine Surgery Complications and Risks in the Elderly. Spine (Phila Pa 1976). 2017;42(6):E347-E354.
[6] SMITH JS, FU KM, POLLY DJ, et al. Complication rates of three common spine procedures and rates of thromboembolism following spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976). 2010;35(24):2140-2149.
[7] CARLSON BC, ROBINSON WA, WANDERMAN NR, et al. A Review and Clinical Perspective of the Impact of Osteoporosis on the Spine. Geriatr Orthop Surg Rehabil.2019;10:1467854505.
[8] WILLNER D, SPENNATI V, STOHL S, et al. Spine surgery and blood loss: systematic review of clinical evidence. Anesth Analg. 2016;123(5):1307-1315.
[9] LAPAGE KG, WOUTERS PF. The patient with hypertension undergoing surgery. Curr Opin Anaesthesiol. 2016;29(3):397-402.
[10] DELESKOG L, LAURSEN NO, NIELSEN BR, et al. Vertebral fracture assessment by DXA is inferior to X-ray in clinical severe osteoporosis. Osteoporos Int. 2016;27(7):2317-2326.
[11] HAREL R, STYLIANOU P, KNOLLER N. Cervical spine surgery: approach-related complications. World Neurosurg. 2016;94:1-5.
[12] SMORGICK Y, BAKER KC, BACHISON CC, et al. Hidden blood loss during posterior spine fusion surgery. Spine J. 2013;13(8): 877-881.
[13] WU YS, ZHANG H, ZHENG WH, et al. Hidden blood loss and the influential factors after percutaneous kyphoplasty surgery. Eur Spine J. 2017;26(7):1878-1883.
[14] UHRENHOLT L, CHARLES AV, GREGERSEN M, et al. Histological osteoarthritic changes in the human cervical spine facet joints related to age and sex. Spine (Phila Pa 1976). 2018; 43(12):E689-E696.
[15] ZHENG B, HAO D, GUO H, et al. ACDF vs TDR for patients with cervical spondylosis - an 8 year follow up study. BMC Surg. 2017; 17(1):113. [16] MUZEVIC D, SPLAVSKI B, BOOP FA, et al. Anterior cervical discectomy with instrumented allograft fusion: lordosis restoration and comparison of functional outcomes among patients of different age groups. World Neurosurg. 2018;109:e233-e243.
[17] LIM S, CARABINI LM, KIM RB, et al. Evaluation of American Society of Anesthesiologists classification as 30-day morbidity predictor after single-level elective anterior cervical discectomy and fusion. Spine J. 2017;17(3):313-320.
[18] GOODNOUGH LT, RUDNICK S, PRICE TH, et al. Increased preoperative collection of autologous blood with recombinant human erythropoietin therapy. N Engl J Med.1989;321(17): 1163-1168.
[19] PAUYO T, VERMA N, MARWAN Y, et al. Canadian Consensus for the Prevention of Blood Loss in Spine Surgery. Spine (Phila Pa 1976).2017;42(1):E50-E55.
[20] PATEL N, BAGAN B, VADERA S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007; 6(4):291-297.
[21] NARAIN AS, HIJJI FY, HAWS BE, et al. Impact of body mass index on surgical outcomes, narcotics consumption, and hospital costs following anterior cervical discectomy and fusion. J Neurosurg Spine. 2018;28(2):160-166.
[22] TUREL MK, KEROLUS MG, ADOGWA O, et al. Cervical arthroplasty: what does the labeling say? Neurosurg Focus. 2017;42(2):E2.
[23] BUCKLAND AJ, BAKER JF, ROACH RP, et al. Cervical disc replacement - emerging equivalency to anterior cervical discectomy and fusion. Int Orthop. 2016;40(6):1329-1334.
[24] LANDI A, GREGORI F, MAROTTA N, et al. Efficacy, security, and manageability of gelified hemostatic matrix in bleeding control during thoracic and lumbar spine surgery: floseal versus surgiflo. J Neurol Surg A Cent Eur Neurosurg. 2016;77(2):139-143.
[25] BURGER W, CHEMNITIUS JM, KNEISSL GD, et al. Low-dose aspirin for secondary cardiovascular prevention - cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation - review and meta-analysis. J Intern Med. 2005; 257(5):399-414.
[26] EPSTEIN NE. When to stop anticoagulation, anti-platelet aggregates, and non-steroidal anti-inflammatories (NSAIDs) prior to spine surgery. Surg Neurol Int. 2019;10:45.
[27] THAKUR S, RIYAZ B, PATIL A, et al. Novel drug delivery systems for NSAIDs in management of rheumatoid arthritis: An overview. Biomed Pharmacother. 2018;106:1011-1023.
[28] CHOI SH, CHO JH, HWANG CJ, et al. Preoperative Radiographic parameters to predict a higher pseudarthrosis rate after anterior cervical discectomy and fusion. Spine (Phila Pa 1976).2017; 42(23):1772-1778.
[29] PENZKOFER R, HOFBERGER S, SPIEGL U, et al. Biomechanical comparison of the end plate design of three vertebral body replacement systems. Arch Orthop Trauma Surg,2011;131(9):1253-1259.
[30] RONG X, LOU J, LI H, et al. How to choose when implants of adjacent height both fit the disc space properly in single-level cervical artificial disc replacement. Medicine (Baltimore).2017; 96(29):e6954.
[31] WANG H, SUN W, FU D, et al. Update on biomaterials for prevention of epidural adhesion after lumbar laminectomy. J Orthop Translat. 2018;13:41-49.
[32] 金永明,郑嘉寅,张骏,等.脊柱转移性肿瘤后路360度减压内固定手术时间和出血量的影响因素分析[J].浙江医学,2014,36(6):489-493.
[33] 钱邦平,邱勇,乔军,等.全椎弓根螺钉矫正青少年特发性脊柱侧凸术中出血量及手术时间的影响因素分析[J].解剖与临床,2011,16(2): 124-126. [34] 刘丰,尹庆水,吴锐辉,等.颈椎前路减压与椎内静脉丛相关的应用解剖学研究[J].中国临床解剖学杂志,2008,26(3):262-264. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [5] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [6] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [7] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [8] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [9] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [10] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [11] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [12] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [13] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [14] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [15] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||