Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (23): 3654-3661.doi: 10.3969/j.issn.2095-4344.2730
Previous Articles Next Articles
Reasonable choice of occipitocervical angle and posterior occipitocervical angle in basilar invagination patients during occipitocervical fusion
Yang Sheng, Tang Chao, Liao Yehui, Tang Qiang, Ma Fei, He Hongchun, Zhong Dejun
- Department of Spine Surgery, the Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Received:2019-12-02Revised:2019-12-05Accepted:2020-01-17Online:2020-08-18Published:2020-04-25 -
Contact:Zhong Dejun, MD, Chief physician, Department of Spine Surgery, the Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Yang Sheng, Master candidate, Physician, Department of Spine Surgery, the Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
Supported by:The Project of Sichuan Provincial Health and Family Planning Commission, No. 16PJ551
CLC Number:
Cite this article
Yang Sheng, Tang Chao, Liao Yehui, Tang Qiang, Ma Fei, He Hongchun, Zhong Dejun. Reasonable choice of occipitocervical angle and posterior occipitocervical angle in basilar invagination patients during occipitocervical fusion [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(23): 3654-3661.
share this article
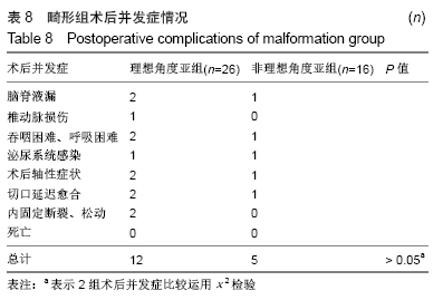
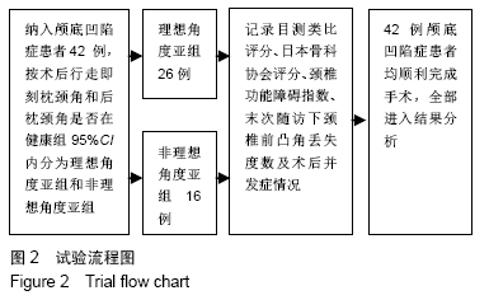
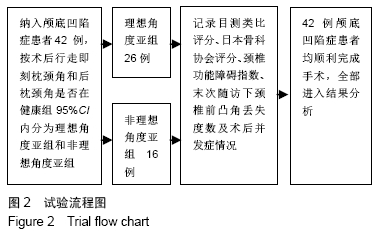
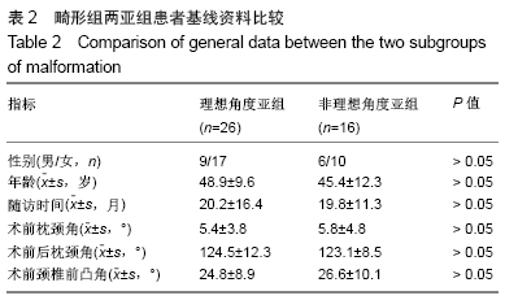
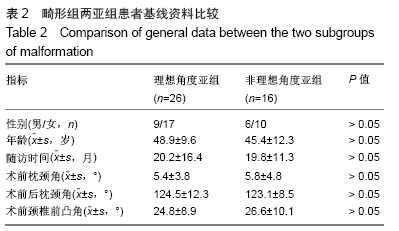
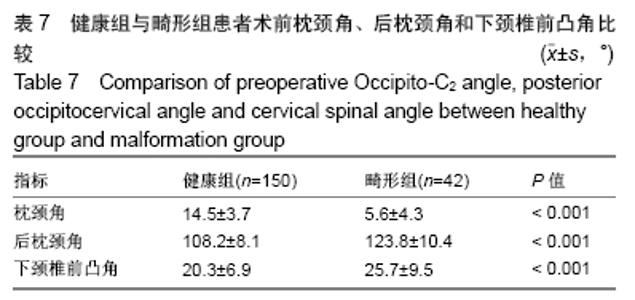
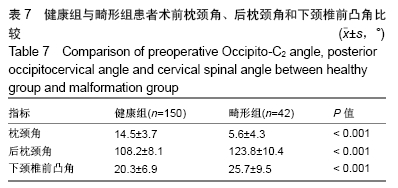
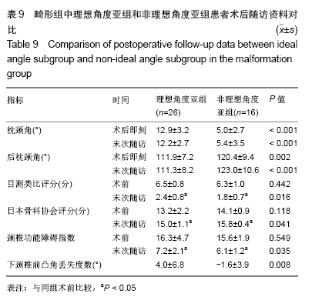
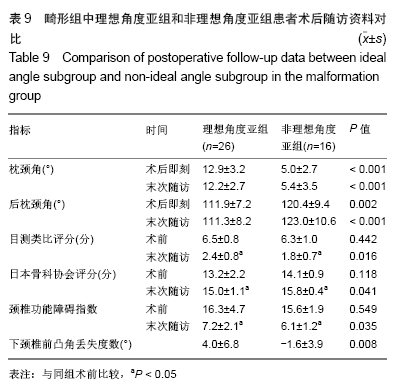
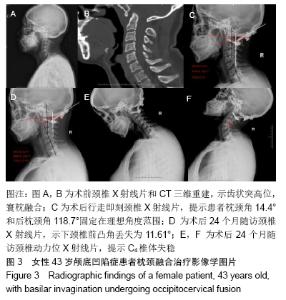
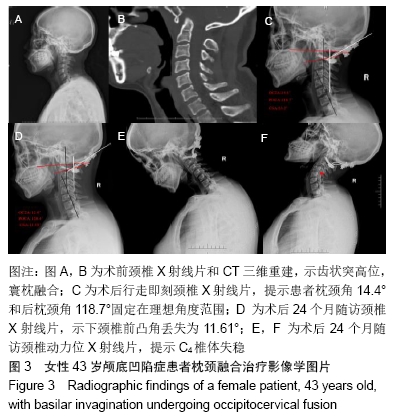
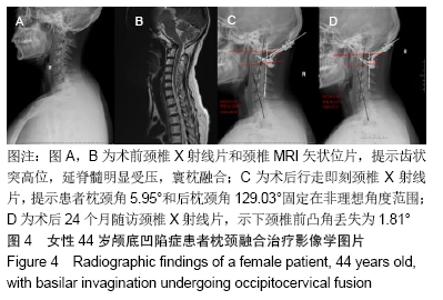
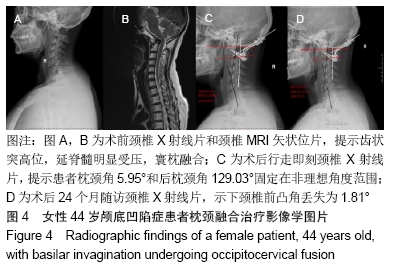
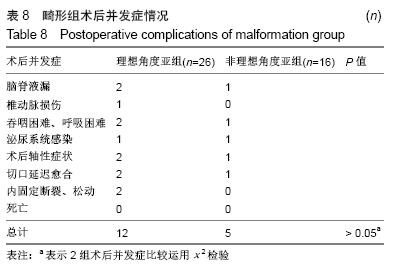
2.7 畸形组术后并发症及术后行走即刻枕颈角和后枕颈角选择固定情况 畸形组42例患者中,26例(理想角度亚组)术后行走即刻枕颈角和后枕颈角固定在理想角度范围(健康组的95%CI内);16例(非理想角度亚组)枕颈角和后枕颈角固定选择不在健康组95%CI,其中14例(87.5%,14/16)枕颈角低于7.2°(健康组95%CI的下限值),2例(12.5%,2/16)后枕颈角高于124.0°(健康组95%CI的上限值)。 理想角度组术后并发症情况:脑脊液漏2例,椎动脉损伤1例,吞咽困难、呼吸困难2例,泌尿系统感染1例,术后轴性症状2例,切口延迟愈合2例,内固定松动及断裂2例。 非理想角度亚组术后并发症情况:脑脊液漏1例,吞咽困难1例,泌尿系统感染1例,术后轴性症状1例,切口延迟愈合1例。 椎动脉损伤为非优势侧椎动脉损伤,行椎动脉修补术。吞咽困难、呼吸困难共3例,其中2例为一过性,对症支持治疗后好转;理想角度亚组1例患者考虑术中枕颈区角度选择不合理,行再手术治疗,术中调整枕颈角及后枕颈角角度。理想角度组有2例内固定松动及断裂,均行再手术治疗,调整枕颈角及后枕颈角角度。其余并发症经对症治疗全部痊愈,对患者术后临床疗效结果评价未产生影响,见表8。 "
| [1] GOEL A , BHATJIWALE M , DESAI K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88(6):962-968. [2] 唐军伟. 颅底凹陷症分型及对手术式选择的意义[D].乌鲁木齐:新疆医科大学,2010. [3] ATUL G. Atlanto-axial joint distraction in the treatment of select cases of basilar invagination, syringomyelia and fixed atlanto-axial dislocation. Nepal J Neurosci. 2005; 2:1-6. [4] KLIMO P JR, RAO G, BROCKMEYER D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007;18(3) :463-478. [5] SAWIN PD , MENEZES AH. Basilar invagination in osteogenesis imperfecta and related osteochondrodysplasias: medical and surgical management. J Neurosurg. 1997;86(6):950-960. [6] GOEL A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281-286. [7] WANG C , YAN M , ZHOU HT , et al. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine. 2006;31(11):E306-E313. [8] DING X , ABUMI K , ITO M , et al. A retrospective study of congenital osseous anomalies at the craniocervical junction treated by occipitocervical plate-rod systems. Eur Spine J. 2012;21(8):1580-1589. [9] PAN J , HUANG D , HAO D , et al. Occipitocervical fusion: Fix to C2 or C3? Clin Neurol Neurosurg. 2014;127:134-139. [10] MATSUNAGA S, ONISHI T, SAKOU T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine. 2001;26(2):161-165. [11] LOGROSCINO CA, GENITIEMPO M, CASULA S. Relevance of the cranioaxial angle in the occipitocervical stabilization using an original construct: a retrospective study on 50 patients. Eur Spine J. 2009;18 Suppl 1(1):7-12. [12] TAIGO I, TAKEO F, KOSHIRO K, et al. Postoperative increase in occiput–c2 angle negatively impacts subaxial lordosis after occipito–upper cervical posterior fusion surgery. Asian Spine J. 2016;10(4):744-747. [13] YOSHIDA M, NEO M, FUJIBAYASHI S, et al. Upper-airway obstruction after short posterior occipitocervical fusion in a flexed position. Spine. 2007; 32(8): E267-270. [14] MASANORI I , MASASHI N ,MITSURU T,et al. The O-C2 angle established at occipito- cervical fusion dictates the patient’s destiny in terms of postoperative dyspnea and/or dysphagia. Eur Spine J. 2014;23:328-336. [15] SHESHADRI V , MOGA R , MANNINEN P , et al. Airway adverse events following posterior occipito-cervical spinal fusion. J Clin Neurosci. 2017; 39:124-129. [16] NAGASHIMA S,NAGAE M,ARAI Y, et al. A new method of measuring the occipitocervical angle that could be applied as an intraoperative indicator during occipitocervical fusion. Clin Spine Surg. 2016;30(7):981-987. [17] GROB D, FRAUENFELDER H, MANNION AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007;16(5): 669-678. [18] GUO Q , NI B , YANG J , et al. Relation between alignments of upper and subaxial cervical spine: a radiological study. Arch Orthopa Trauma Surg. 2011; 131(6):857-862. [19] PASSIAS PG , WANG S , KOZANEK M , et al. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech. 2013;26(1):15-21. [20] RIEL RU , LEE MC , KIRKPATRICK JS . Measurement of a posterior occipitocervical fusion angle. J Spinal Disord Tech. 2010; 23(1):27-29. [21] MAULUCCI CM, GHOBRIAL GM, SHARAN AD,et al. Correlation of posterior occipitocervical angle and surgical outcomes for occipitocervical fusion. Evid Based Spine Care J. 2014; 5(2):163-165. [22] 李广州,刘浩,丁琛,等. 后路枕颈融合术中联合应用后枕颈角和枕颈角调整枕颈固定角度的临床研究[J]. 中国修复重建外科杂志, 2019, 33(1):42-47. [23] GORE D. Roentgenographic findings of the cervical spine in asymptomatic patients. Spine. 1986;11(6):521-524. [24] FOERSTER O. Die leitungsbahnen des schmerzgefuhls und die chirurgische behandlung der schmerzustande. Berlin: Urban and Schwarzenberg,1927:266-267. [25] SHEREKAR SK, YADAV YR, BASOOR AS, et al. Clinical implications of alignment of upper and lower cervical spine. Neurol India. 2006;54(3): 264-267. [26] 唐超,李广州,廖烨晖,等.150例健康成人枕颈角和后枕颈角影像参数测量及其临床意义[J].中国脊柱脊髓杂志,2018,28(3):239-244. [27] 张鹏. 枕颈融合术后下颈椎曲度异常的生物力学和临床研究[D].上海:中国人民解放军海军军医大学,2018. [28] KUNAKORNSAWAT S, PLUEMVITAYAPORN T, PRUTTIKUL P, et al. A new method for measurement of occipitocervical angle by occiput-C3 angle. Eur J Orthop Surg Traumatol. 2017;27(8): 1051-1056. [29] WU X , QI Y , TAN M , et al. Incidence and risk factors for adjacent segment degeneration following occipitoaxial fusion for atlantoaxial instability in non-rheumatoid arthritis. Arch Orthop Trauma Surg. 2018; 138(7):921-927. [30] GOEL A. Instability and basilar invigilation. J Craniovertebr Junction Spine. 2012;3(1): 1-2. [31] MENEZES AH. Craniovertebral junction database analysis: incidence classification, presentation, and treatment algorithms. Childs Nerv Syst. 2008;24(10): 1101-1108. [32] OGIHARA N, TAKAHASHI J, HIRABAYASHI H, et al. Surgical treatment of Klippel-Feil syndrome with basilar invigilation. Eur Spine J. 2013;22 Suppl (3): 1-8. [33] SALUNKE P, SHARMA M, SODHI HB, et al. Congenital atlantoaxial dislocation: a dynamic process and role of facets in irreducibility: Clinical article. J Neurosurg Spine. 2011; 15(6): 678-685. [34] TANG C, LI GZ, LIAO YH, et al. Importance of the occipitoaxial angle and posterior occipitocervical angle in occipitocervical fusion. Orthop Surg. 2019;11(6):1054-1063. [35] GLASSMAN SD, BERVEN S, BRIDWELL K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005; 30(6):682-688. [36] BERJANO P, BASSANI R, CASERO G, et al. Failures and revisions in surgery for sagittal imbalance: analysis of factors influencing failure. Eur Spine J. 2013;22 Suppl 6:S853-858. [37] 孟阳,刘浩,戎鑫,等.颅底凹陷症合并寰枢椎脱位患者枕颈角与下颈椎曲度的关系[J].中国脊柱脊髓杂志,2017,27(1):25-30. |
| [1] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [2] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [3] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [4] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [5] | Gao Yan, Zhao Licong, Zhao Hongzeng, Zhu Yuanyuan, Li Jie, Sang Deen. Alteration of low frequency fluctuation amplitude at brain-resting state in patients with chronic discogenic low back pain [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1160-1165. |
| [6] | Wu Gang, Chen Jianwen, Wang Shilong, Duan Xiaoran, Liu Haijun, Dong Jianfeng. Simple HyProCure subtalar stabilization in treatment of adolescent flexible flatfoot combined with painful accessory navicular bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 901-905. |
| [7] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [8] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [9] | Zhang Nianjun, Chen Ru. Analgesic effect of cocktail therapy combined with femoral nerve block on total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 866-872. |
| [10] | Li Quanxi, Shen Yu, Wan Wei, Sun Shanzhi. Changes of abdominal wall mechanics and pain after tension-free inguinal hernia repair with polypropylene mesh [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 548-552. |
| [11] | Wang Xiaofei, Teng Xueren, Cong Linyan, Zhou Xu, Ma Zhenhua. Herbert screw internal fixation for treating adult osteochondritis dissecans of the knees [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 397-402. |
| [12] | Yang Wei, Chen Zehua, Yi Zhiyong, Huang Xudong, Han Qingmin, Zhang Ronghua. Effectiveness of intra-articular injection of hyaluronic acid versus placebo in the treatment of early and mid-stage knee osteoarthritis: a Meta-analysis based on randomized, double-blind, controlled, clinical trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3760-3766. |
| [13] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| [14] | Jiang Hai, Yu Yu, Liu Zhicheng, Zhang Qiliang. Treatment of plantar fasciitis with extracorporeal shock wave and corticosteroid injection: comparison of plantar pressure and gait [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3286-3291. |
| [15] | Deng Zhibo, Li Zhi, Wu Yahong, Mu Yuan, Mu Yuexi, Yin Liangjun. Local infiltration anesthesia versus femoral nerve block for pain control and safety after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3401-3408. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||