Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (3): 749-759.doi: 10.12307/2025.867
Previous Articles Next Articles
Risk prediction models of recurrence after percutaneous endoscopic lumbar discectomy: a systematic review and meta-analysis
Yu Weijie1, 2, Cao Dongdong1, 2, Guo Tianci1, 2, Niu Puyu1, 2, Yang Jialin1, 2, Wang Simin1, 2, Liu Aifeng1, 2
- 1First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; 2National Clinical Research Center of Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China
-
Received:2024-10-15Accepted:2024-12-18Online:2026-01-28Published:2025-07-09 -
Contact:Liu Aifeng, Chief physician, Doctoral supervisor, First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; National Clinical Research Center of Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China -
About author:Yu Weijie, Doctoral candidate, First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; National Clinical Research Center of Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China -
Supported by:Tianjin Health and Family Planning Industry High-level Talents Selection and Training Project (Jinmen Medical Talents), No. TJSJMYXYC-D2-028 (to LAF); Tianjin Science and Technology Plan Project, No. 23KPXMRC00170 (to LAF)
CLC Number:
Cite this article
Yu Weijie, Cao Dongdong, Guo Tianci, Niu Puyu, Yang Jialin, Wang Simin, Liu Aifeng. Risk prediction models of recurrence after percutaneous endoscopic lumbar discectomy: a systematic review and meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 749-759.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
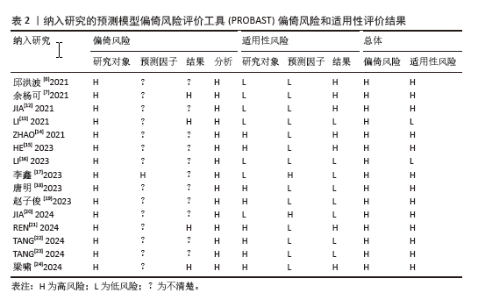
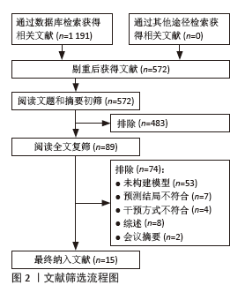
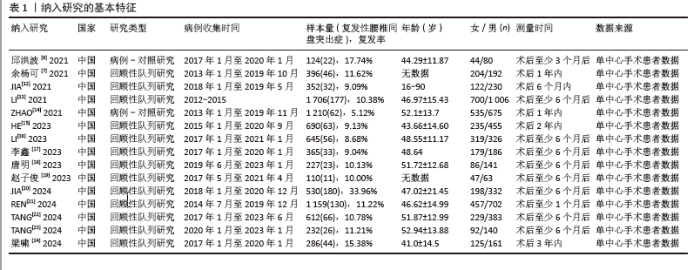
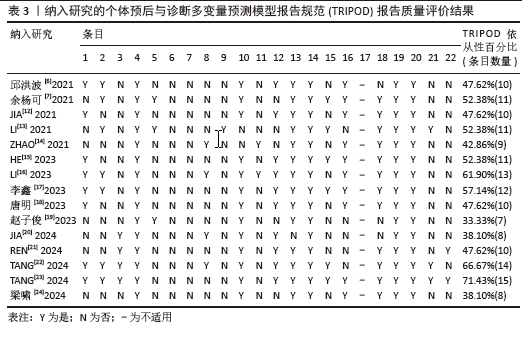
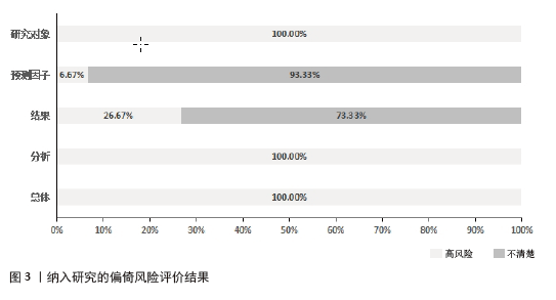
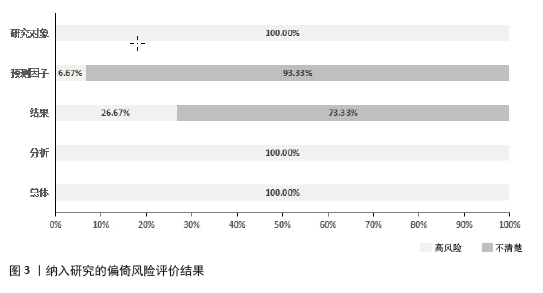
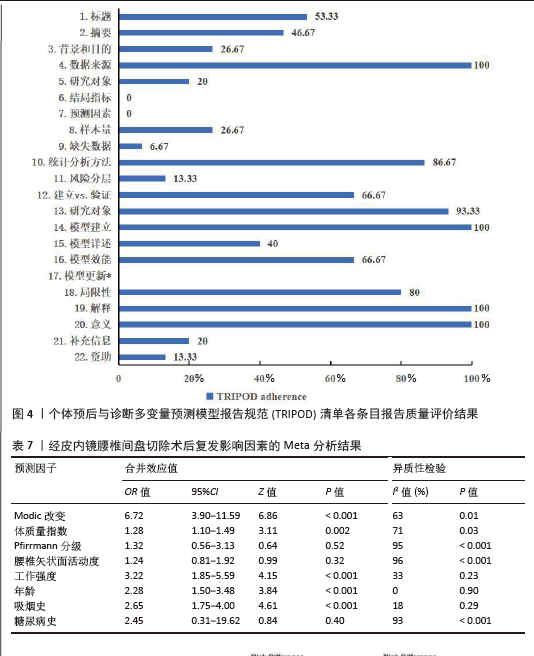
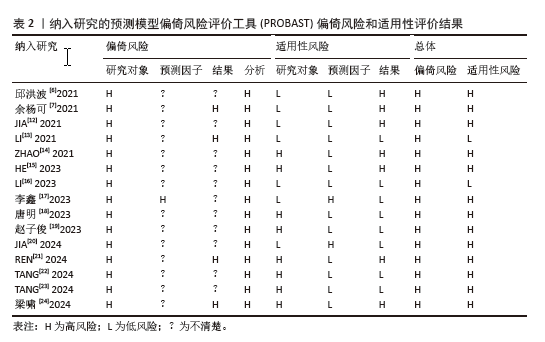
2.3 纳入研究的偏倚风险、适用性和报告质量评价结果 2.3.1 偏倚风险评价结果 纳入研究总体均为高偏倚风险:①研究对象领域:15项研究均为高偏倚风险[6,7,12-24],主要与研究类型均来自于回顾性队列研究或病例-对照研究有关;②预测因子领域:1项研究为高偏倚风险[17],主要与模型所包含的年龄和手术节段预测因子可能无效有关;其余14项研究为偏倚风险不清楚[6-7,12-16,18-24],主要原因为未报告是否在不了解结果信息的情况下评估预测因子;③结果领域:4项研究为高偏倚风险[7,13,21,24],主要原因是复发性腰椎间盘突出症未依据国际标准,而是采用了次优的分类方法而容易导致分类错误;11项研究为偏倚风险不清楚[6,12,14-20,22-23],主要原因是无法得知预测因子评估和结果确定的时间间隔信息;④分析领域:15项研究均为高偏倚风险[6-7,12-24],主要原因在于大部分研究均未明确提及缺失数据的处理方法。结果见表2及图3。 2.3.2 适用性评价结果 2项研究为低适用性风险[13,16],其余13项研究为高适用性风险[6-7,12,14-15,17-24]。其中,3项研究限定为L4/5或L5/S1单节段突出[14-15,24],3项研究要求症状持续时间至少3个月且保守治疗无效[18,22-23],1项研究限定为非椎间盘钙化引起,且保守治疗6周无缓解[21],1项研究限定为≥60岁的腰椎间盘突出症患者[19],结果见表2。 2.3.3 报告质量评价结果 纳入的15项研究整体报告质量较低,仅有1项研究达到至少70%的TRIPOD依从性[23],11项研究为40%-70%[6-7,12-18,21-22],3项研究低于40%的TRIPOD依从性[19-20,24],结果见表3。 TRIPOD清单中,除“讨论”部分外,其余5个部分报告质量均较低:①标题和摘要(条目1-2):仅5项研究同时符合标题和摘要描述要求[6,16-17,22-23],7项研究未在标题中注明是否为模型开发或验证[7,13-14,19-21,24],3项研究未说明研究场所[12,15,18];②前言(条目3):4项研究充分报道了研究背景[20-23],其余11项研究未充分阐述模型开发或验证的基本原理[6-7,12-19,24];③方法(条目4-12):15项研究均对数据来源进行较好地描述[6-7,12-24]; 其中3项研究充分描述了研究对象的基本特征[7,13,19],剩余12项研究未详述研究对象接受干预措施的具体细节而不符合要求[6,12,14-18,20-24];15项研究均未对结局指标和预测因子盲法评估的具体细节进行描述;4项研究对样本量的计算方法进行描述[14,16,20,22],其余11项研究未说明样本量是如何确定的[6-7,12-13,15,17-19,21,23-24];1项研究采用相邻平均法处理缺失数据[13],其余14项研究未描述缺失数据的处理方法[6-7,12,14-24];13项研究充分描述统计分析方法[6-7,12-13,15,17-24];2项研究实现了风险分层[14,16];④结果(条目13-17):大部分研究充分描述了研究对象特征和模型建立过程,但仅有6项研究达到模型详述报告要求[7,13,15,17,22-23],其余9项未介绍如何使用预测模型[6,12,14,16,18-21,24];10项研究充分描述了模型区分度和校准度等相关评价指标[6-7,12,14-18,23-24];15项研究均未涉及模型更新;⑤讨论(条目18-20):除3项研究未讨论局限性外[6,19-20],其余12项研究均较好地阐述了研究局限性和未来临床应用价值[7,12-18,21-24];⑥其他信息(条目21-22):仅3项研究提供补充信息或网页计算器[13,22-23];2项研究同时描述了资金来源及其在研究中的作用[21,23]。结果见表3,4及图4。"
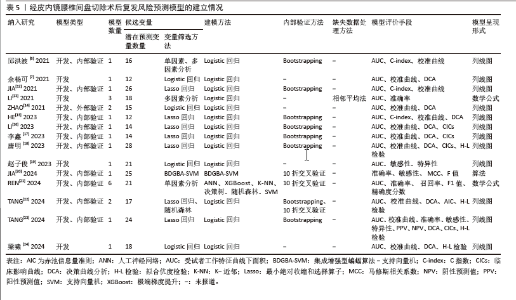
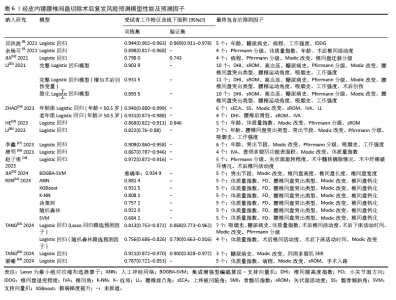
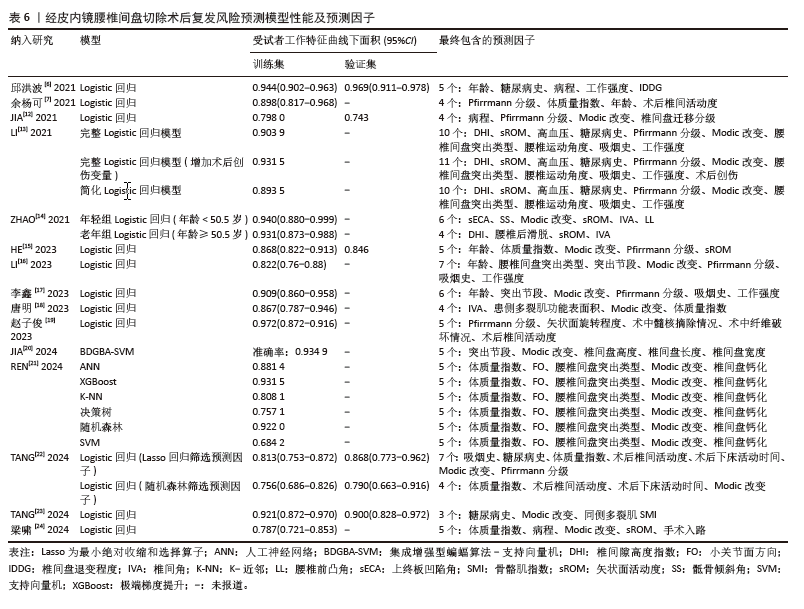
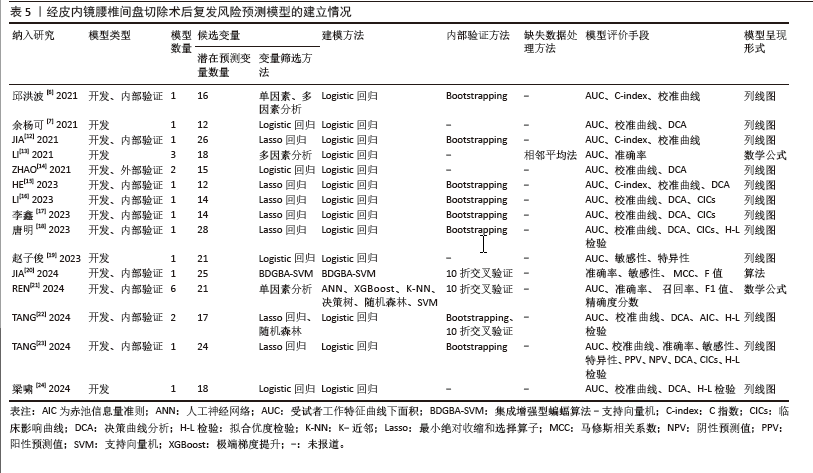
2.4 风险预测模型的建立情况及性能 纳入的15项研究中包含24个模型,其中4项为模型的开发研究[7,13,19,24],10项为模型的开发与内部验证[6,12,15-18,20-23],包括Bootstrapping法、10折交叉验证以及两者结合,另有1项为模型的开发与外部验证[14]。在建模方法选择上,除JIA等[20]采用集成增强型蝙蝠算法-支持向量机模型和REN等[21]选取人工神经网络、极端梯度提升、K近邻、决策树、随机森林和支持向量机模型外,其余13项研究均采取Logistic回归分析方法建模[6-7,12-19,22-24]。 潜在预测变量数量范围为15-28个,变量筛选方法包括最小绝对收缩和选择算子回归、单因素分析、多因素分析和Logistic回归分析等。仅有1项研究描述缺失数据的处理方法为相邻平均法[13],其余研究未报告缺失数据的处理情况。模型呈现形式方面,12项研究采用列线图[6-7,12,14-19,22-24],2项应用数学公式表达[13,21],1项描述为算法形式[20]。结果见表5。 在模型性能方面,14项研究采用受试者工作特征曲线下面积报告区分度[6,7,12-19,21-24],范围为0.684-0.972,模型性能良好;JIA等[20]通过报道模型准确率为0.934 9,提示模型预测性能较好。11项研究通过校准曲线报道模型校准度[6-7,12,14-18,22-24],9项研究采用决策曲线分析法评估其临床应用价值[7,14-18,22-24]。结果见表6。"
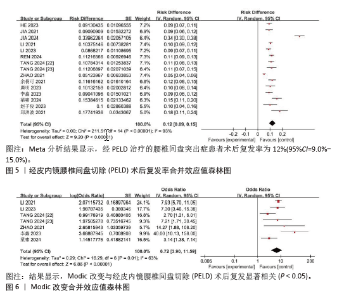
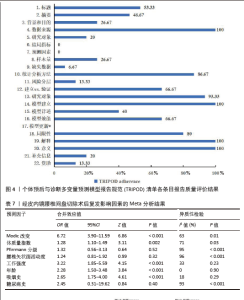
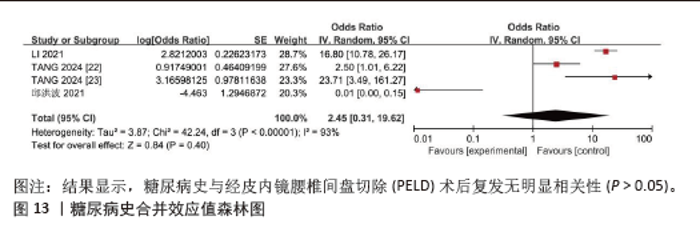
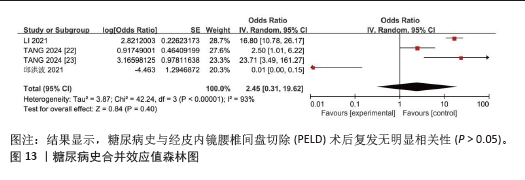
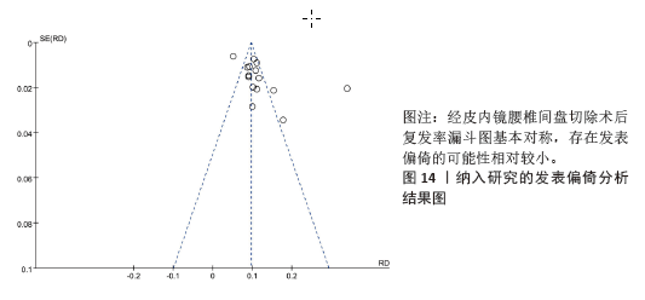
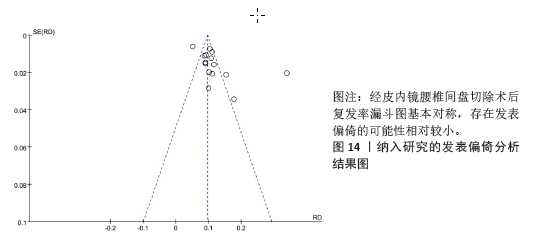
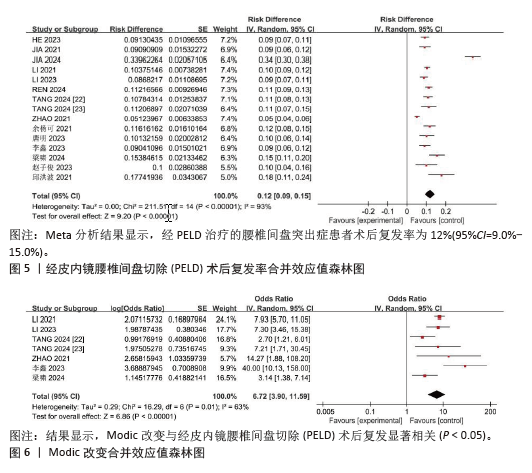
2.5 Meta分析结果 将15项研究中预测因子重复出现较多者进行Meta合并,预测因子分别是Modic改变、体质量指数、Pfirrmann分级、腰椎矢状面活动度、工作强度、年龄、吸烟史和糖尿病史,具体Meta分析结果见表7。 2.5.1 PELD术后复发率 针对15项研究中的PELD术后复发率进行Meta合并,各研究间存在异质性(I2=93%,P < 0.001),对该复发率进行敏感性分析,剔除任一研究后结果变化不大,故采用随机效应模型,Meta分析结果显示,经PELD治疗的腰椎间盘突出症患者术后复发率为12%(95%CI=9.0%-15.0%),见图5。 2.5.2 Modic改变 共12项研究纳入此变量[12-18,20-24],其中JIA等[12]、HE等[15]、JIA等[20]和REN等[21]的研究未提供相关数据,无法进行Meta合并。由于异质性较大,在将唐明等[18]的研究剔除后异质性显著改善(I2=63%,P=0.01),仍采用随机效应模型进行Meta合并。结果显示,Modic改变是PELD术后复发的独立危险因素(OR=6.72,95%CI=3.90-11.59,P < 0.001),结果见图6。 "
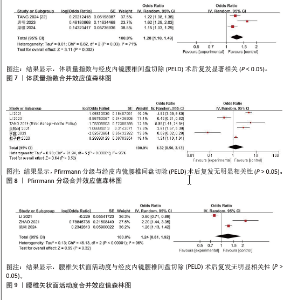
2.5.3 体质量指数 共6项研究纳入此变量[7,15,18,21-22,24],其中HE等[15]和REN等[21]的研究未提供相关数据,无法进行Meta合并。由于异质性较大,将余杨可等[7]研究剔除后异质性改善(I2=71%,P=0.03),仍需采用随机效应模型合并效应值。结果显示,体质量指数是PELD术后复发的独立危险因素(OR=1.28,95%CI=1.10-1.49,P=0.002),结果见图7。 2.5.4 Pfirrmann分级 共8项研究纳入此变量[7,12-13,15-17,19,22],其中JIA等[12]和HE等[15]的研究未提供相关数据,无法进行Meta合并。各研究间存在较高异质性(I2=95%,P < 0.001),剔除任一研究后结果变化不大,仍采用随机效应模型。结果显示,Pfirrmann分级经Meta合并后无统计学差异(P=0.52),结果见图8。 2.5.5 腰椎矢状面活动度 共4项研究纳入此变量[13-15,24],其中HE等[15]的研究未提供相关数据,无法进行Meta合并。各研究间存在较高异质性(I2=96%,P < 0.001),剔除任一研究后结果变化不大,仍采用随机效应模型。结果显示,腰椎矢状面活动度经Meta合并后无统计学差异(P=0.32),结果见图9。"
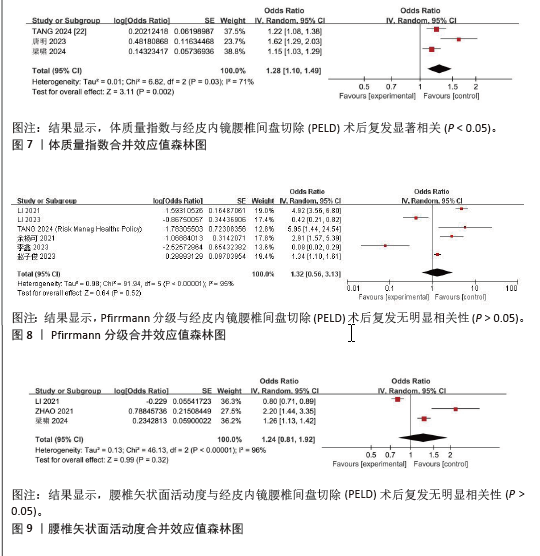
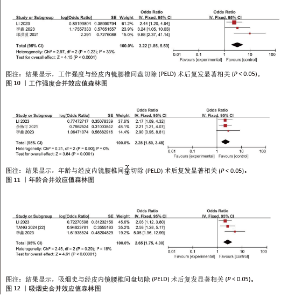
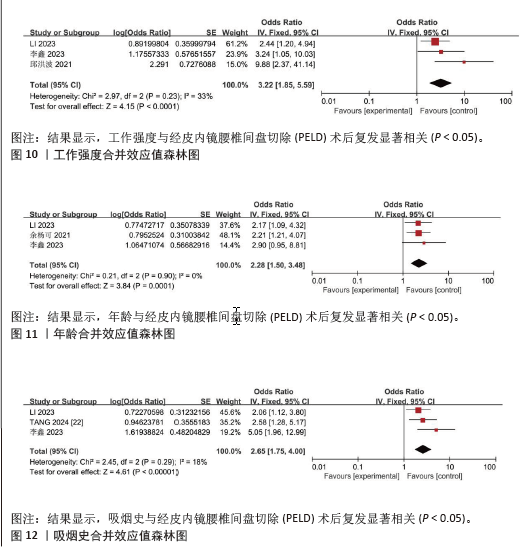
2.5.6 工作强度 共4项研究纳入此变量[6,13,16-17],由于异质性较大,将LI等[13]研究剔除后异质性改善(I2=33%,P=0.23),采用固定效应模型合并效应值。结果显示,工作强度是PELD术后复发的独立危险因素(OR=3.22,95%CI=1.85-5.59,P < 0.001),结果见图10。 2.5.7 年龄 共5项研究纳入此变量[6-7,15-17],其中HE等[15]的研究未提供相关数据,无法进行Meta合并。由于异质性较大,将邱洪波等[6]研究剔除后异质性改善(I2=0%,P=0.90),采用固定效应模型进行Meta合并。结果显示,年龄是PELD术后复发的独立危险因素(OR=2.28,95%CI=1.50-3.48,P=0.0001),结果见图11。 2.5.8 吸烟史 共4项研究纳入此变量[13,16-17,22],由于异质性较大,将LI等[13]研究剔除后异质性降低(I2=18%,P=0.29),采用固定效应模型合并效应值。结果显示,吸烟史是PELD术后复发的独立危险因素(OR=2.65,95%CI=1.75-4.00,P < 0.001),结果见图12。"
| [1] 中华医学会骨科学分会脊柱外科学组, 中华医学会骨科学分会骨科康复学组. 腰椎间盘突出症诊疗指南[J]. 中华骨科杂志,2020,40(8):477-487. [2] POJSKIC M, BISSON E, OERTEL J, et al. Lumbar disc herniation: Epidemiology, clinical and radiologic diagnosis WFNS spine committee recommendations. World Neurosurg X. 2024;22:100279. [3] MUTHU S, RAMAKRISHNAN E, CHELLAMUTHU G. Is Endoscopic Discectomy the Next Gold Standard in the Management of Lumbar Disc Disease? Systematic Review and Superiority Analysis. Global Spine J. 2021;11(7):1104-1120. [4] KONG M, XU D, GAO C, et al. Risk Factors for Recurrent L4-5 Disc Herniation After Percutaneous Endoscopic Transforaminal Discectomy: A Retrospective Analysis of 654 Cases. Risk Manag Healthc Policy. 2020;13: 3051-3065. [5] 莫航沣, 陈亚萍, 韩慧, 等. 临床预测模型研究方法与步骤[J]. 中国循证医学杂志,2024,24(2):228-236. [6] 邱洪波, 唐乐, 何甜, 等. 椎间孔镜治疗腰椎间盘突出症患者术后复发的个体化预警模型的建立[J]. 西安交通大学学报(医学版),2021,42(6):817-822. [7] 余杨可, 夏磊. 经皮内镜腰椎间盘切除术术后复发的危险因素分析及概率预测[J]. 河南医学研究,2021,30(6):973-977. [8] GEERSING GJ, BOUWMEESTER W, ZUITHOFF P, et al. Search filters for finding prognostic and diagnostic prediction studies in Medline to enhance systematic reviews. PLoS One. 2012;7(2):e32844. [9] MOONS KG, DE GROOT JA, BOUWMEESTER W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11(10): e1001744. [10] MOONS KGM, WOLFF RF, RILEY RD, et al. PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann Intern Med. 2019;170(1):W1-W33. [11] COLLINS GS, REITSMA JB, ALTMAN DG, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594. [12] JIA M, SHENG Y, CHEN G, et al. Development and validation of a nomogram predicting the risk of recurrent lumbar disk herniation within 6 months after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. 2021; 16(1):274. [13] LI Y, WANG B, LI H, et al. Adjuvant surgical decision-making system for lumbar intervertebral disc herniation after percutaneous endoscopic lumber discectomy: a retrospective nonlinear multiple logistic regression prediction model based on a large sample. Spine J. 2021;21(12):2035-2048. [14] ZHAO C, ZHANG H, WANG Y, et al. Nomograms for Predicting Recurrent Herniation in PETD with Preoperative Radiological Factors. J Pain Res. 2021;14: 2095-2109. [15] HE H, MA J, XIONG C, et al. Development and Validation of a Nomogram to Predict the Risk of Lumbar Disk Reherniation within 2 Years After Percutaneous Endoscopic Lumbar Discectomy. World Neurosurg. 2023;172:e349-e356. [16] LI X, PAN B, CHENG L, et al. Development and Validation of a Prognostic Model for the Risk of Recurrent Lumbar Disc Herniation After Percutaneous Endoscopic Transforaminal Discectomy. Pain Physician. 2023;26(1):81-90. [17] 李鑫, 罗鸣然, 李根, 等. 建立与验证经皮内窥镜腰椎间盘切除后复发风险的预测模型[J]. 中国组织工程研究,2023, 27(13):2087-2092. [18] 唐明, 曾凡袆, 常新东, 等. 椎旁功能性肌肉横截面积预测腰椎间盘突出症术后复发的Nomogram建立与验证[J]. 暨南大学学报(自然科学与医学版),2023, 44(6):602-611. [19] 赵子俊, 王轶, 张志强, 等. 老年腰椎间盘突出症患者经皮椎间孔镜髓核摘除术后复发的影响因素及列线图预测模型[J]. 川北医学院学报,2023,38(4): 500-504. [20] JIA M, LAI J, LI K, et al. Optimizing prediction accuracy for early recurrent lumbar disc herniation with a directional mutation-guided SVM model. Comput Biol Med. 2024;173:108297. [21] REN G, LIU L, ZHANG P, et al. Machine Learning Predicts Recurrent Lumbar Disc Herniation Following Percutaneous Endoscopic Lumbar Discectomy. Global Spine J. 2024;14(1):146-152. [22] TANG M, WANG S, WANG Y, et al. Development and Validation of a Nomogram Predicting Postoperative Recurrent Lumbar Disc Herniation Based on Activity Factors. Risk Manag Healthc Policy. 2024;17: 689-699. [23] TANG M, WANG S, WANG Y, et al. Nomogram Development and Validation for Predicting Postoperative Recurrent Lumbar Disc Herniation Based on Paraspinal Muscle Parameters. J Pain Res. 2024;17:2121-2131. [24] 梁啸, 李东儒, 陈筱, 等. 内镜腰椎间盘切除术后复发的因素及预测模型[J].中国矫形外科杂志,2024,32(9):775-780. [25] YEN HK, OGINK PT, HUANG CC, et al. A machine learning algorithm for predicting prolonged postoperative opioid prescription after lumbar disc herniation surgery. An external validation study using 1,316 patients from a Taiwanese cohort. Spine J. 2022;22(7):1119-1130. [26] BERG B, GOROSITO MA, FJELD O, et al. Machine Learning Models for Predicting Disability and Pain Following Lumbar Disc Herniation Surgery. JAMA Netw Open. 2024; 7(2):e2355024. [27] AZIMI P, MOHAMMADI HR, BENZEL EC, et al. Use of artificial neural networks to predict recurrent lumbar disk herniation. J Spinal Disord Tech. 2015;28(3):E161-E165. [28] HARADA GK, SIYAJI ZK, MALLOW GM, et al. Artificial intelligence predicts disk re-herniation following lumbar microdiscectomy: development of the “RAD” risk profile. Eur Spine J. 2021;30(8): 2167-2175. [29] SHAN ZM, REN XS, SHI H, et al. Machine Learning Prediction Model and Risk Factor Analysis of Reoperation in Recurrent Lumbar Disc Herniation Patients After Percutaneous Endoscopic Lumbar Discectomy. Global Spine J. 2023;10:21925682231173353. [30] ZHAO J, ZENG L, ZHAO S, et al. Associations of recurrent lumbar disc herniation after percutaneous endoscopic lumbar discectomy with age, body mass index, modic change, disc degeneration and sacral slope: A quantitative review. Exp Ther Med. 2024;27(5):195. [31] JIANG L, XIE X, HE R, et al. Analysis of risk factors for post-operative recurrence after percutaneous endoscopic lumbar discectomy in patients with lumbar disc herniation: a meta-analysis. J Orthop Surg Res. 2023;18(1):935. [32] ZHAO Z, QI H, WANG C, et al. Investigating the impact of cartilaginous endplate herniation on recovery from percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. 2024;19(1):264. [33] FENG X, NIAN S, CHEN J, et al. Modic changes in patients with lumbar disc herniation followed more than 1 year after lumbar discectomy: a systematic review and meta-analysis. PeerJ. 2024;12:e17851. [34] KE S, HE X, YANG M, et al. The biomechanical influence of facet joint parameters on corresponding segment in the lumbar spine: a new visualization method. Spine J. 2021;21(12):2112-2121. [35] YANG W, YANG Y, WANG Y, et al. Metformin prevents the onset and progression of intervertebral disc degeneration: New insights and potential mechanisms (Review). Int J Mol Med. 2024;54(2):71. [36] 周顺, 黄品强, 杨勇. 基于病因学角度探究LDH中医证型职业风险的相关性[J]. 浙江中医药大学学报,2021,45(10): 1125-1129. [37] LAASIK R, LANKINEN P, KIVIMAKI M, et al. Return to work after lumbar disc herniation surgery: an occupational cohort study. Acta Orthop. 2021;92(6):638-643. [38] WALTER SS, LORBEER R, HEFFERMAN G, et al. Correlation between thoracolumbar disc degeneration and anatomical spinopelvic parameters in supine position on MRI. PLoS One. 2021;16(6):e0252385. [39] ELMASRY S, ASFOUR S, DE RIVERO VACCARI JP, et al. Effects of Tobacco Smoking on the Degeneration of the Intervertebral Disc: A Finite Element Study. PLoS One. 2015;10(8): e0136137. [40] 陈小英. 腰椎间盘突出症术后复发的影响因素研究[J]. 中国全科医学,2020,23(S1): 140-142. [41] 陈香萍, 张奕, 庄一渝, 等. PROBAST: 诊断或预后多因素预测模型研究偏倚风险的评估工具[J]. 中国循证医学杂志,2020, 20(6): 737-744. [42] RILEY RD, ENSOR J, SNELL KIE, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;368:m441. [43] VAN SMEDEN M, MOONS KG, DE GROOT JA, et al. Sample size for binary logistic prediction models: Beyond events per variable criteria. Stat Methods Med Res. 2019;28(8):2455-2474. [44] DWAN K, GAMBLE C, WILLIAMSON PR, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias - an updated review. PLoS One. 2013;8(7):e66844. |
| [1] | Wang Zhipeng, Zhang Xiaogang, Zhang Hongwei, Zhao Xiyun, Li Yuanzhen, Guo Chenglong, Qin Daping, Ren Zhen. A systematic review of application value of machine learning to prognostic prediction models for patients with lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 740-748. |
| [2] | Xue Hui, Li Dongnan, Zhao Yadi, Chen Chao, Xie Zongyuan. Relationship between BCR/ABL gene expression and recurrence before and after allogeneic transplantation in Ph chromosome positive acute lymphoblastic leukemia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 139-144. |
| [3] | Xu Fanping, Li Qinchun, Tang Dongfang. Targeting diverse chimeric antigen receptor T cell-related targets in treatment of B-cell hematological malignancies: a review of long-term follow-up data [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 248-259. |
| [4] | Lu Qi, Sun Maji, Wang Xuezhi, Song Ting, Ma Yiming, Yuan Feng, Chen Hongliang. Two visual arthroplasty techniques for L5-S1 disc herniation: a half-year follow-up evaluation of clinical outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1841-1847. |
| [5] | Feng Zhimeng, Sun Ning, Sun Zhaozhong, Li Yuefei, Liu Changzhen, Li Sa. Three-dimensional image reconstruction can safely assist one-hole split endoscope in treatment of #br# L5/S1 far lateral lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1876-1882. |
| [6] | Zhang Chunlin, Hou Zhaohua, Yan Xu, Jiang Yan, Fu Su, Ning Yongming, Li Dongzhe, Dong Chao, Liu Xiaokang, Wang Yongkui, Cao Zhengming, Yang Tengyue. Decompression mechanism of symmetrically adduction of lumbar decompression induced resorption of herniated nucleus pulpous [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1810-1819. |
| [7] | Jing Ruyi, Chen Yingxin, Cao Lei . Prognosis of deep lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1626-1633. |
| [8] | Zhi Fang, Zhu Manhua, Xiong Wei, Lin Xingzhen. Analgesic effect of acupuncture in a rat model of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 936-941. |
| [9] | Yang Yu, Li Yinghao, Duo Zhuangzhi, Zhou Dingrong. Effect of overall functional physical exercise on lumbar biomechanics in patients with lumbar disc herniation after surgery [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7096-7101. |
| [10] | Liang Jiyao, Zhou Honghai, Wei Guikang, Su Shaoting, Chen Longhao, He Xinyu, Liu Liangpu. Quantification of in vivo biomechanics and analysis of influencing factors in cervical spine fixed-point rotation manipulation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 486-492. |
| [11] | Zhang Ziyu, Chen Longhao, Sheng Wei, Lyu Hanzhe, Shen Ying, Wang Binghao, Lyu Zhizhen, Lyu Lijiang. Application of artificial intelligence in the diagnosis and treatment of lumbar disc herniation: evolution towards standardization, efficiency, and precision of diagnosis and treatment methods [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6269-6276. |
| [12] | Bai Liang, Fu Su, Yan Xu, Zhang Chunlin, Li Ying . Measurement of intervertebral disc height and analysis of strength after induced resorption of herniated nucleus pulpous [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5785-5794. |
| [13] | Tu Zesong, Xu Daxing, Luo Hongbin, Wang Yusheng, Feng Xinglun, Peng Zhonghua, Du Shaolong. Construction of a risk prediction model for failure of proximal femoral nail antirotation fixation in intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5845-5853. |
| [14] |
Wang Qianliang, Zhang Qianzhongyi, Peng Yujian, Yan Jun.
Effects of unilateral biportal endoscopic transforaminal lumbar interbody fusion on paraspinal muscles
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5862-5868.
|
| [15] | Zhang Ruofan, Guan Huanhuan, He Zhuoqun, Zhang Yunfeng, Jin Feng, Wang Zhiqiang, Wang Jianzhong, Li Xiaohe, Zhu Yong, Wang Haiyan, Zhang Kai. Effect of minimally invasive interbody fusion device height on lumbar biomechanics in patients with adolescent lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4421-4429. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||