Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (20): 4389-4400.doi: 10.12307/2025.701
Bibliometric and visual analysis of Theta burst transcranial magnetic stimulation
Gao Wenyan1, Zheng Zhaoyan2, Pan Shang2, Wang Peipei2, Ji Chunhui3, Lyu Shaoping2
- 1College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 2Department of Rehabilitation Medicine, Qingdao Central Hospital of Rehabilitation University, Qingdao 266042, Shandong Province, China; 3College of Mechanical Engineering, Tianjin University, Tianjin 300350, China
-
Received:2024-08-05Accepted:2024-09-23Online:2025-07-18Published:2024-12-25 -
Contact:Lyu Shaoping, PhD, Chief physician, Professor, Department of Rehabilitation Medicine, Qingdao Central Hospital of Rehabilitation University, Qingdao 266042, Shandong Province, China -
About author:Gao Wenyan, Master’s candidate, College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
Supported by:the National Natural Science Foundation of China, No. 32271432 (to JCH); Qingdao Medical Research Guidance Projects, Nos. 2023-WJZD206 (to LSP), 2022-WJZD052 (to LSP), 2023-WJZD224 (to WPP), and 2022-WJZD053 (to WPP)
CLC Number:
Cite this article
Gao Wenyan, Zheng Zhaoyan, Pan Shang, Wang Peipei, Ji Chunhui, Lyu Shaoping. Bibliometric and visual analysis of Theta burst transcranial magnetic stimulation[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4389-4400.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
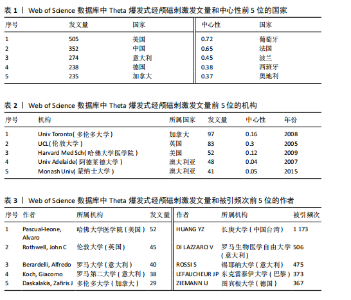
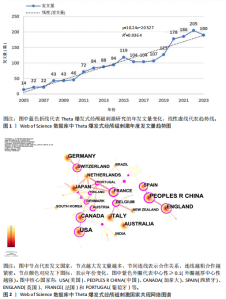
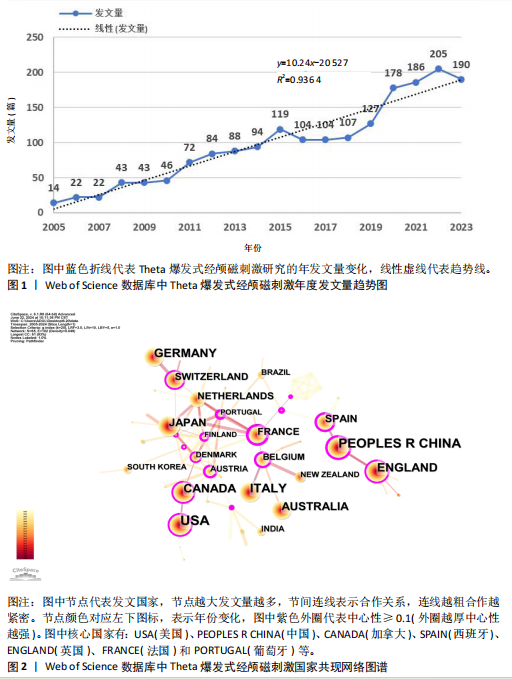
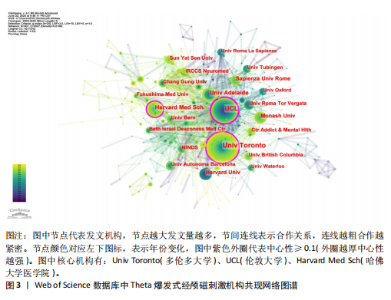
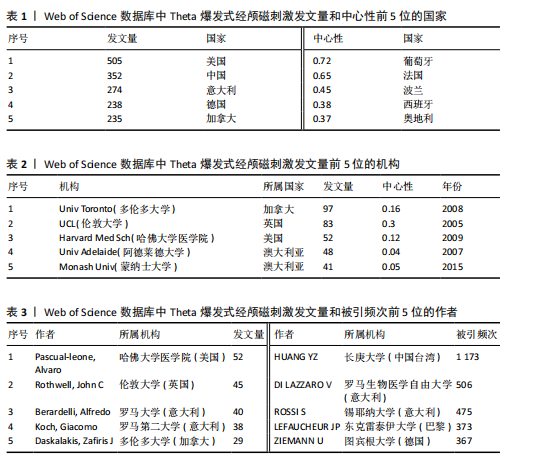
2.1 TBS研究年度发文量分析 由于2024年的数据尚未完全统计,文章仅分析了2005-2023年TBS相关文献的发文量。如图1所示,2005-2015年发文量稳步上升,这一时期TBS应用处于起步阶段并逐渐受到关注;2016-2018年发文量短暂下降;2018年后,发文量开始大幅增长,TBS进入快速发展阶段,2022年达最大值205篇。趋势线显示,拟合方程y=10.24x-20 527,R2=0.936 4(R2越接近1,拟合效果越好),2005-2023年TBS发文量在趋势线周围上下波动,2023年回落趋势线上,预测未来发文量将继续增加。 2.2 TBS研究国家共现合作分析 国家网络图谱共包括65个节点和102条连线,网络密度为0.049,见图2。其中,美国、中国、意大利等在2005年便开始关注TBS研究并持续至今,起步较早。如表1所示,美国(505篇)发文量最多,中国(352篇)、意大利(274篇)紧随其后。葡萄牙(0.72)、法国(0.65)、波兰(0.45)中心性较高,国家间合作较频繁。总体来看,区域间形成了以中国为枢纽的中国、西班牙、英国合作网络,以及以美国、加拿大为代表的北美国家与以葡萄牙、法国、奥地利为代表的欧洲国家的紧密合作网络,显示了国际TBS研究的区域性分布和密切合作关系。 2.3 TBS研究机构共现合作分析 机构网络图谱共包括507个研究机构,构成2 027条合作关系,网络密度为0.015 8,见图3。其中,加拿大多伦多大学(97篇)发文量最多,其次为英国伦敦大学(83篇)和美国哈佛大学医学院(52篇)。同时这3所大学的中心性也最高,在网络中起桥梁作用,见表2。整体来看,发文量前10位的机构以各国大学为主,占比90%,机构间形成了以多伦多大学、伦敦大学和哈佛大学医学院为枢纽的紧密且频繁的合作网络,且这些机构大多来自北美和欧洲等发达国家,与国家合作网络所示结果一致。 2.4 TBS研究核心作者分析 作者共现图谱共包括701名学者,形成1 757条合作关系,网络密度为0.007 2,见图4。哈佛大学医学院的Pascual-Leone,Alvaro以52篇论文居首位,伦敦大学的Rothwell,John C和罗马大学的Berardelli,Alfredo紧随其后,主要自北美和欧洲等发达国家,与机构共现结果一致,见表3。然而,所有作者中心性值均 < 0.1,相比于国家和机构的合作模式,多呈现相对均匀的合作关系,缺乏枢纽性的核心作者。利用普莱斯定律公式:M=0.749×√ Nmax,计算显示M=5.4,说明发文量≥6篇为该领域核心作者,文章共64名核心作者,论文量为888篇,占总量的40.3%,虽接近普莱斯定律的50%标准,但仍说明TBS研究的核心学者群尚未形成。 作者共被引图谱共包括981个节点和8 416条连线,网络密度为0.017 5,见图5。其中,被引频次最高的是中国长庚大学的HUANG YZ教授(1 173次),罗马生物医学自由大学的DILAZZARO V教授(506次)和锡耶纳大学的ROSSI S教授(475次)位列第2,3位,见表3。然而,仅新西兰奥塔哥大学的ABRAHAM WC中心性 > 0.1,对此关键节点进一步研究发现,ABRAHAM WC的研究主要涉及突触可塑性、长时程增强和长时程抑制等内容,说明TBS相关神经调节机制的研究是后续研究的基础。 2.5 文献共被引、聚类和突现分析 文献共被引图谱共包含1 258篇文献和5 941条连线,网络密度为0.007 5,见图6。其中,被引频次前10位的文献类型包括5篇综述[15-19]、5项临床"

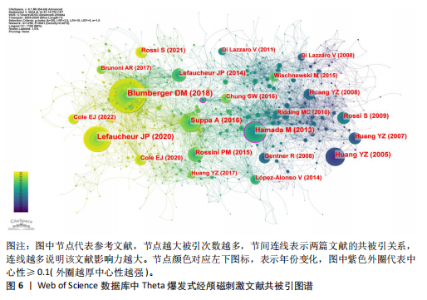
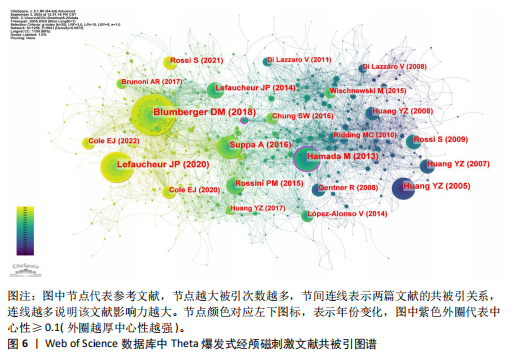
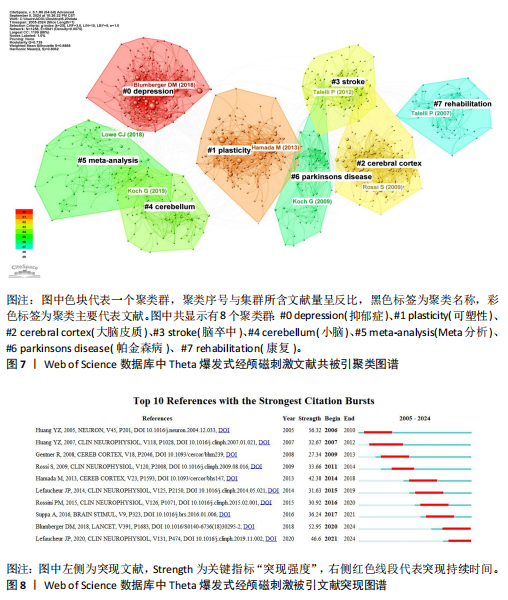
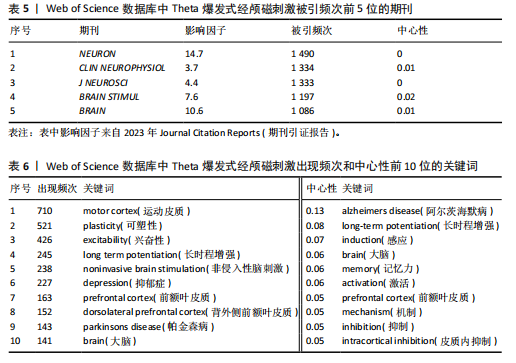
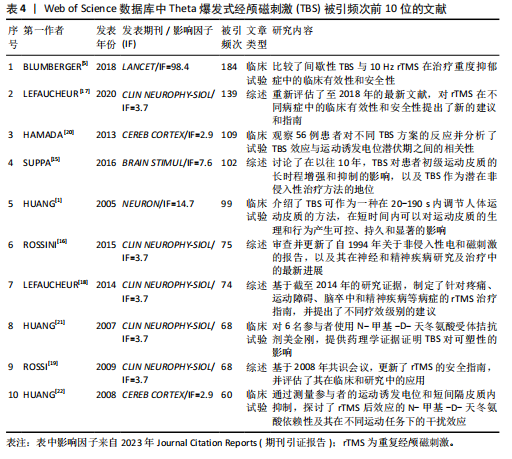
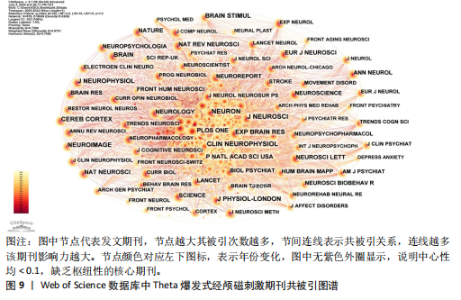
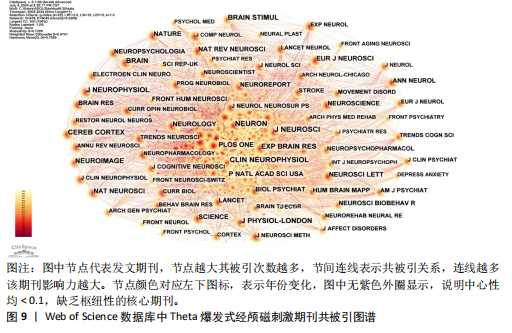
试验[1,5,20-22],见表4。综述性研究通过总结现有证据,可为后续研究提供参考基础,而临床试验则直接提供权威数据并指导实际应用,因此两者引用较为频繁。BLUMBERGER等[5]发表在《LANCET》的一项随机对照试验被引用184次,居首位。LEFAUCHEUR等[17]基于以往研究更新了rTMS的应用指南,被引用139次,位列第二。然而,仅2篇文献中心性值 > 0.1,分别是HAMADA等[20]关于不同TBS方案与运动诱发电位潜伏期相关性的随机对照试验,以及NETTEKOVEN等[23]关于不同iTBS脉冲量对皮质兴奋性和功能连接影响的研究。总之,以上关键节点的内容说明,TBS治疗抑郁症等精神疾病的疗效仍是研究重点,而系统化的应用指南也备受关注,TBS的作用机制和原理则是其他研究开展的基础,与其他研究共同引用最为密切。 文献共被引聚类图谱共显示8个聚类群,分别是:#0抑郁症(代表文献BLUMBERGER等[5])、#1可塑性(代表文献HAMADA等[20])、#2大脑皮质(代表文献ROSSI等[19])、#3脑卒中(代表文献TALELLI等[24])、#4小脑(代表文献KOCH等[25])、#5 Meta分析(代表文献LOWE等[26])、#6帕金森病(代表文献KOCH等[27])、#7康复(代表文献TALELLI等[28]),见图7。图中,Q值=0.739 0 > 0.3,S值=0.886 8 > 0.7,说明文献聚类结构显著且可信。 文献突现指某文献在特定时段内被频繁引用,通常反映领域内新的研究热点或重要发现。如图8所示,近20年内最早出现突现的是HUANG等[1]于2005年发表的一项临床试验,突现强度为56.32,位居首位。在2007年,该团队的另一项随机对照试验突现持续时间最长,为5年[21]。LEFAUCHEUR等[17]在2020年发表的rTMS应用指南突现年份最晚,并持续至今。 2.6 期刊共被引和双图叠加分析 期刊共被引图谱共包括878个节点和8 049条连线,网络密度为0.020 9,见图9。《NEURON》(1 490次)被引频次最高,其次是《CLIN NEUROPHYSIOL》(1 334次)和《J NEUROSCI》(1 333次)。其中《NEURON》影响因子(IF=14.7)"


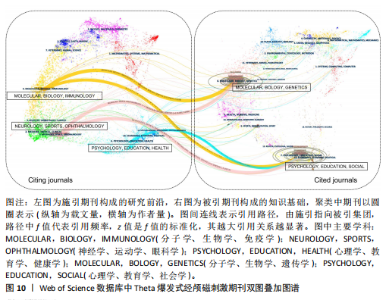
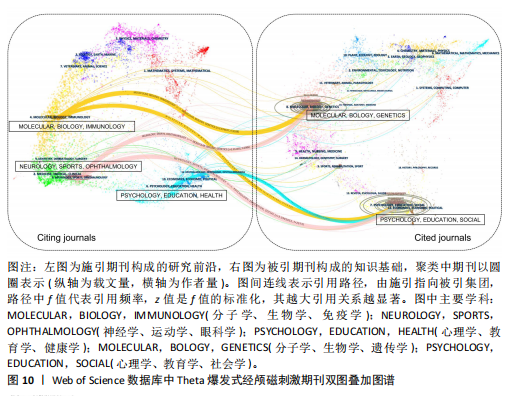
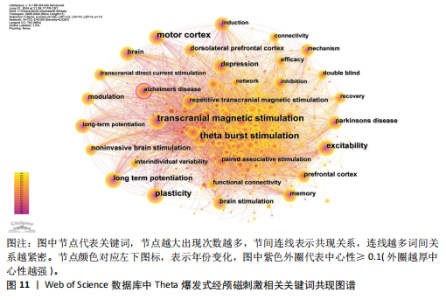
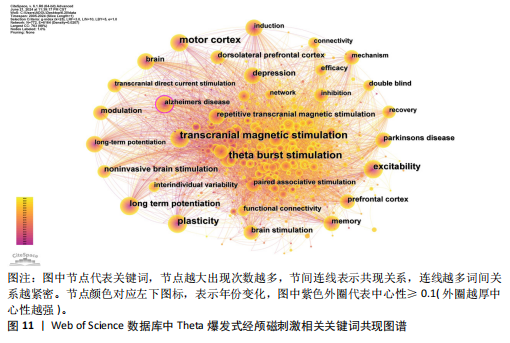
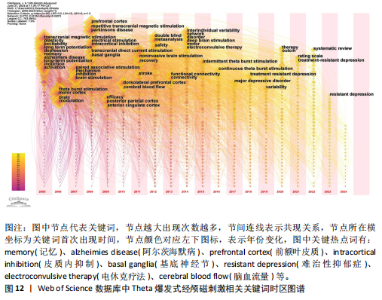
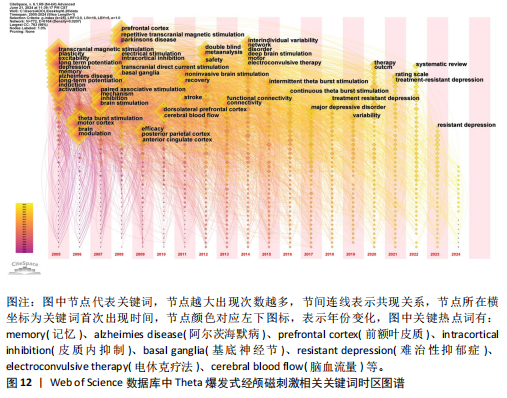
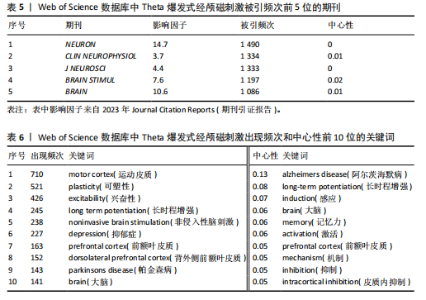
和被引频次均最高,在TBS领域有重要学术影响力,这表明TBS研究主要集中在神经学领域。然而,期刊中心性值均 < 0.1,说明TBS研究在不同学术期刊上的知识传播较为分散,见表5。 基于Journal Citation Reports 2011地图对期刊进行双图叠加,见图10。图中主要存在3条突出引用路径,其中分子学、生物学、免疫学(黄色轨迹)出版物明显受分子学、生物学、遗传学(z=3.67,f=3 188)和心理学、教育学、社会学(z=2.58,f=2 335)的影响;神经学、运动学、眼科学(粉色轨迹)则受分子学、生物学、遗传学(z=3.31,f=2 906)和心理学、教育学、社会学(z=3.40,f=2 973)出版物的影响,这两条路径展示了TBS领域的多学科交叉发展模式。此外,被引集团的心理学、教育学、社会学(z=2.08,f=1 944)表现为向施引集团的心理学、教育学、健康学(蓝色轨迹)领域的独立发展趋势,这表明TBS研究的知识流动呈多样化,未来应重视多学科合作与发展。 2.7 TBS研究热点分析 2.7.1 关键词共现和时区图分析 关键词共现图谱共包含772个节点和6 164条连线,网络密度为0.020 7,见图11。排除与检索策略相关的主题词:如“经颅磁刺激、Theta爆发式刺激、重复经颅磁刺激”后,热点词包括“运动皮质、可塑性、兴奋性、长时程增强、抑郁症、背外侧前额叶皮质、帕金森病”等,见表6。其中“阿尔茨海默病”中心性最高(0.13),在网络中起枢纽作用。时区图显示,2005-2013年,研究主要集中在TBS对不同脑区(如运动皮质、前额叶皮质、后顶叶皮质、背外侧前额叶皮质)的不同作用机制(如可塑性、兴奋性、长时程增强、皮质内抑制、脑血流量、功能连接性)及其对各种疾病(如抑郁症、阿尔茨海默病、帕金森病、脑卒中)的影响。2014-2016年“个体间异质性”“电休克疗法”“间歇性Theta爆发刺激”和“连续性Theta爆发刺激”开始引起学者关注;2017-2024年,研究热点则转向“重度抑郁症”和“难治性抑郁症”并关注至今,见图12。"
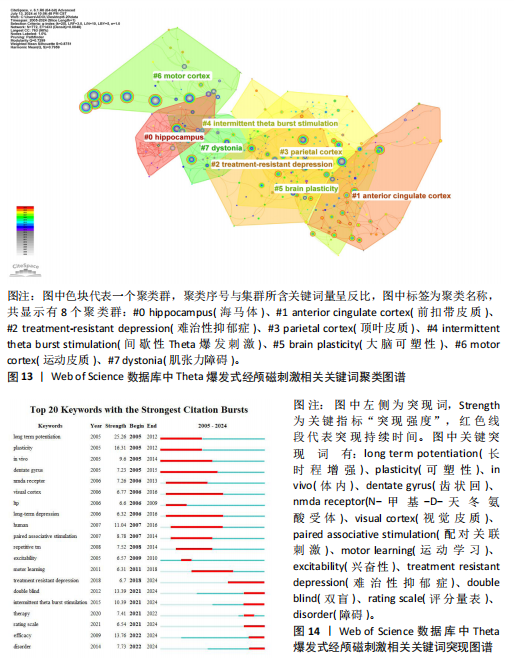
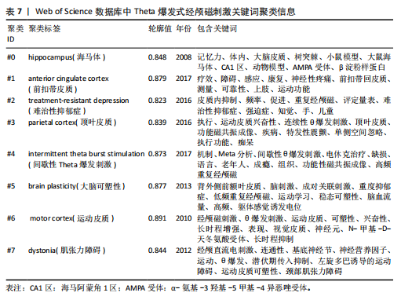
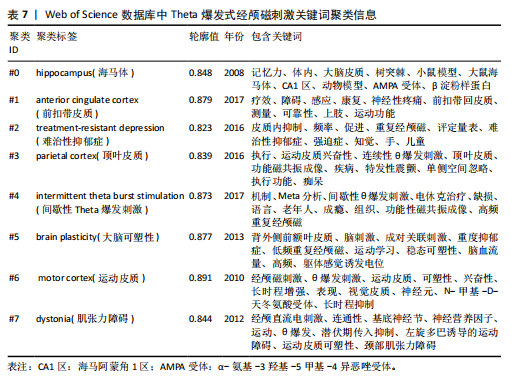
2.7.2 关键词聚类和突现分析 关键词聚类可反映领域内不同研究主题下的知识结构,图中显示有8个聚类主题:#0海马体、#1前扣带皮质、#2难治性抑郁症、#3顶叶皮质、#4间歇性Theta爆发刺激、#5大脑可塑性、#6运动皮质、#7肌张力障碍,见图13。其中,Q值=0.729 9 > 0.3,S值=0.875 1 > 0.7,说明聚类结构显著且可信,具体聚类信息见表7。 关键词突现分析可反映特定时段的研究重点并预测未来趋势。最早突现的关键词有“长时程增强、可塑性、体内、齿状回”,其中“长时程增强”突现强度最高(38.4),“齿状回”突现持续最长(10年)。“疗效”和“障碍”突现最晚,2022年首次出现并持续至今。此外,突现保持至今的还有“难治性抑郁症、双盲、间歇性Theta爆发刺激和评定量表”,未来可重点关注,见图14。"
| [1] HUANG YZ, EDWARDS MJ, ROUNIS E, et al. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201-206. [2] ACEVES-SERRANO L, NEVA J L, MUNRO J, et al. Continuous but not intermittent theta burst stimulation decreases striatal dopamine release and cortical excitability. Exp Neurol. 2022;354(8):114106. [3] WRIGHTSON JG, COLE J, SOHN MN, et al. The effects of D-Cycloserine on corticospinal excitability after repeated spaced intermittent theta-burst transcranial magnetic stimulation: a randomized controlled trial in healthy individuals. Neuropsychopharmacol. 2023;48(8): 1217-1224. [4] KIRKOVSKI M, DONALDSON PH, DO M, et al. A systematic review of the neurobiological effects of theta-burst stimulation (TBS) as measured using functional magnetic resonance imaging (fMRI). Brain Struct Funct. 2023;228(3-4):717-749. [5] BLUMBERGER DM, VILA-RODRIGUEZ F, THORPE KE, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet. 2018;391(1):1683-1692. [6] NINKOV A, FRANK JR, MAGGIO LA. Bibliometrics: Methods for studying academic publishing. Perspect Med Educ. 2022;11(3):173-176. [7] 赵盾,祁令臣,徐金凡,等.膝骨关节炎疼痛领域热点与前沿的可视化分析[J].中国组织工程研究,2025,29(15):3280-3289. [8] LIU X, ZHAO S, TAN L, et al. Frontier and hot topics in electrochemiluminescence sensing technology based on CiteSpace bibliometric analysis. Biosens Bioelectron. 2022;201(7):113932. [9] CAI DB, QIN XD, QIN ZJ, et al. Adjunctive continuous theta burst stimulation for major depressive disorder or bipolar depression: a meta-analysis of randomized controlled studies. J Affect Disord. 2024;346(3):266-272. [10] JEMNA N, ZDRENGHEA AC, FRUNZA G, et al. Theta-burst stimulation as a therapeutic tool in neurological pathology: a systematic review. Neurol Sci. 2024;45(3):911-940. [11] BLUMBERGER DM, MULSANT BH, THORPE KE, et al. Effectiveness of standard sequential bilateral repetitive transcranial magnetic stimulation vs bilateral theta burst stimulation in older adults with depression: the FOUR-D randomized noninferiority clinical trial. JAMA Psychiatry. 2022;79(11):1065-1073. [12] FERRARELLI F, PHILLIPS ML. Examining and modulating neural circuits in psychiatric disorders with transcranial magnetic stimulation and electroencephalography: present practices and future developments. Am J Psychiatry. 2021;178(5):400-413.
[13] COLE E, O’SULLIVAN SJ, TIK M, et al. Accelerated theta burst stimulation: safety, efficacy, and future advancements. Biol Psychiatry. 2024;95(6):523-535. [14] XU S, XU D, WEN L, et al. Integrating unified medical language system and kleinberg’s burst detection algorithm into research topics of medications for post-traumatic stress disorder. Drug Des Devel Ther. 2020;14:3899-3913. [15] SUPPA A, HUANG YZ, FUNKE K, et al. Ten years of theta burst stimulation in humans: established knowledge, unknowns and prospects. Brain Stimul. 2016;9(3):323-335. [16] ROSSINI PM, BURKE D, CHEN R, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application. An updated report from an I.F.C.N. Committee. Clin Neurophysiol. 2015;126(6):1071-1107. [17] LEFAUCHEUR JP, ALEMAN A, BAEKEN C, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014-2018). Clin Neurophysiol. 2020; 131(2):474-528. [18] LEFAUCHEUR JP, ANDRE-OBADIA N, ANTAL A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150-2206. [19] ROSSI S, HALLETT M, ROSSINI PM, et al. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120(12):2008-2039. [20] HAMADA M, MURASE N, HASAN A, et al. The role of interneuron networks in driving human motor cortical plasticity. Cereb Cortex. 2013;23(7):1593-1605. [21] HUANG YZ, CHEN RS, ROTHWELL JC, et al. The after-effect of human theta burst stimulation is NMDA receptor dependent. Clin Neurophysiol. 2007;118(5):1028-1032. [22] HUANG YZ, ROTHWELL JC, EDWARDS MJ, et al. Effect of physiological activity on an NMDA-dependent form of cortical plasticity in human. Cereb Cortex. 2008;18(3):563-570. [23] NETTEKOVEN C, VOLZ LJ, KUTSCHA M, et al. Dose-dependent effects of theta burst rTMS on cortical excitability and resting-state connectivity of the human motor system. J Neurosci. 2014;34(20):6849-6859. [24] TALELLI P, WALLACE A, DILEONE M, et al. Theta burst stimulation in the rehabilitation of the upper limb: a semirandomized, placebo-controlled trial in chronic stroke patients. Neurorehabil Neural Repair. 2012;26(8):976-987. [25] KOCH G, BONNI S, CASULA EP, et al. Effect of cerebellar stimulation on gait and balance recovery in patients with hemiparetic stroke: a randomized clinical trial. JAMA Neurol. 2019;76(2):170-178. [26] LOWE CJ, MANOCCHIO F, SAFATI AB, et al. The effects of theta burst stimulation (TBS) targeting the prefrontal cortex on executive functioning: a systematic review and meta-analysis. Neuropsychologia. 2018;111(4):344-359. [27] KOCH G, BRUSA L, CARRILLO F, et al. Cerebellar magnetic stimulation decreases levodopa-induced dyskinesias in Parkinson disease. Neurology. 2009;73(2):113-119. [28] TALELLI P, GREENWOOD RJ, ROTHWELL JC. Exploring theta burst stimulation as an intervention to improve motor recovery in chronic stroke. Clin Neurophysiol. 2007; 118(2):333-342. [29] JANNATI A, OBERMAN LM, ROTENBERG A, et al. Assessing the mechanisms of brain plasticity by transcranial magnetic stimulation. Neuropsychopharmacol. 2023; 48(1):191-208. [30] CAPPON D, den BOER T, JORDAN C, et al. Transcranial magnetic stimulation (TMS) for geriatric depression. Ageing Res Rev. 2022;74(2):101531. [31] MENARDI A, ROSSI S, KOCH G, et al. Toward noninvasive brain stimulation 2.0 in Alzheimer’s disease. Ageing Res Rev. 2022;75(3):101555. [32] SABBAGH M, SADOWSKY C, TOUSI B, et al. Effects of a combined transcranial magnetic stimulation (TMS) and cognitive training intervention in patients with Alzheimer’s disease. Alzheimers Dement. 2020;16(4):641-650. [33] SEYBERT C, COTOVIO G, RODRIGUES DSD, et al. Replicability of motor cortex-excitability modulation by intermittent theta burst stimulation. Clin Neurophysiol. 2023;152(8):22-33. [34] SOLOMON EA, SPERLING MR, SHARAN AD, et al. Theta-burst stimulation entrains frequency-specific oscillatory responses. Brain Stimul. 2021;14(5):1271-1284. [35] LI J, REN M, WANG W, et al. Human Theta burst stimulation combined with subsequent electroacupuncture increases corticospinal excitability. Evid Based Complement Alternat Med. 2020; 2020(1):8824530. [36] QIU S, WANG S, PENG W, et al. Continuous theta-burst stimulation modulates resting-state EEG microstates in healthy subjects. Cogn Neurodyn. 2022;16(3):621-631. [37] VINK J, VAN LIESHOUT E, OTTE WM, et al. Continuous theta-burst stimulation of the contralesional primary motor cortex for promotion of upper limb recovery after stroke: a randomized controlled trial. Stroke. 2023;54(8):1962-1971. [38] RASHID-LOPEZ R, MACIAS-GARCIA P, SANCHEZ-FERNANDEZ FL, et al. Neuroimaging and serum biomarkers of neurodegeneration and neuroplasticity in Parkinson’s disease patients treated by intermittent theta-burst stimulation over the bilateral primary motor area: a randomized, double-blind, sham-controlled, crossover trial study. Front Aging Neurosci. 2023;15:1258315. [39] ZAVOROTNYY M, ZOLLNER R, REKATE H, et al. Intermittent theta-burst stimulation moderates interaction between increment of N-Acetyl-Aspartate in anterior cingulate and improvement of unipolar depression. Brain Stimul. 2020;13(4):943-952. [40] CHANG CH, LIU CY, CHEN SJ, et al. Accelerated theta-burst transcranial magnetic stimulation of the bilateral dorsolateral prefrontal cortex in a patient with post-traumatic stress disorder and major depressive disorder: case report. Front Psychiatry. 2023;14:1061088. [41] POORGANJI M, GOEKE K, ZOMORRODI R, et al. The use of theta burst stimulation in patients with schizophrenia-A systematic review. Schizophr Res. 2023;261(11):245-255. [42] NGETICH R, JIN D, LI W, et al. Enhancing visuospatial working memory performance using intermittent theta-burst stimulation over the right dorsolateral prefrontal cortex. Front Hum Neurosci. 2022;16:752519. [43] JIN X, XU CY, FEI JF, et al. Alzheimer’s disease with depressive symptoms: clinical effect of intermittent theta burst stimulation repetitive transcranial magnetic stimulation. World J Psychiatry. 2024;14(8):1216-1223.
[44] NEUTEBOOM D, ZANTVOORD JB, GOYA-MALDONADO R, et al. Accelerated intermittent theta burst stimulation in major depressive disorder: a systematic review. Psychiatry Res. 2023;327(9):115429.
[45] CAI DB, QIN ZJ, LAN XJ, et al. Accelerated intermittent theta burst stimulation for major depressive disorder or bipolar depression: a systematic review and meta-analysis. Asian J Psychiatr. 2023; 85(7):103618. [46] TSAI PY, LIN WS, TSAI KT, et al. High-frequency versus theta burst transcranial magnetic stimulation for the treatment of poststroke cognitive impairment in humans. J Psychiatry Neurosci. 2020;45(4):262-270. [47] FENG Y, HUANG Z, MA X, et al. Intermittent theta-burst stimulation alleviates hypoxia-ischemia-caused myelin damage and neurologic disability. Exp Neurol. 2024; 378(8):114821. [48] WU Y, WANG L, YU F, et al. Intermittent theta burst stimulation (iTBS) as an optimal treatment for schizophrenia risk decision: an ERSP study. Front Psychiatry. 2021;12:594102. [49] GOH KK, CHEN CH, WU TH, et al. Efficacy and safety of intermittent theta-burst stimulation in patients with schizophrenia: a meta-analysis of randomized sham-controlled trials. Front Pharmacol. 2022; 13:944437. [50] STEKIC A, ZELJKOVIC M, ZARIC KM, et al. Intermittent theta burst stimulation ameliorates cognitive deficit and attenuates neuroinflammation via PI3K/Akt/mTOR signaling pathway in Alzheimer’s-Like disease model. Front Aging Neurosci. 2022;14:889983. [51] ZHAO H, JIANG C, ZHAO M, et al. Comparisons of accelerated continuous and intermittent theta burst stimulation for treatment-resistant depression and suicidal ideation. Biol Psychiatry. 2024;96(1):26-33. [52] SANNA A, FOLLESA P, PULIGHEDDU M, et al. Cerebellar continuous theta burst stimulation reduces levodopa-induced dyskinesias and decreases serum BDNF levels. Neurosci Lett. 2020;716(3):134653. [53] LI H, CUI L, LI J, et al. Comparative efficacy and acceptability of neuromodulation procedures in the treatment of treatment-resistant depression: a network meta-analysis of randomized controlled trials. J Affect Disord. 2021;287(10):115-124. [54] BAKER TE, ROBLES D. Theta burst stimulation of the hyperdirect pathway boosts inhibitory control and reduces craving and smoking in nicotine-dependent adults. Biol Psychiatry Cogn Neurosci Neuroimaging. 2023;8(11):1072-1074. [55] SU H, CHEN T, JIANG H, et al. Intermittent theta burst transcranial magnetic stimulation for methamphetamine addiction: a randomized clinical trial. Eur Neuropsychopharmacol. 2020;31(2):158-161. [56] BOZZAY ML, BRIGIDO S, VAN TWM, et al. Intermittent theta burst stimulation in veterans with mild alcohol use disorder. J Affect Disord. 2021;293(16):314-319. [57] HUANG D, CHAI D, HUANG P, et al. Continuous theta burst stimulation for the treatment of delirium after non-cardiac surgery. J Clin Anesth. 2023;90(7):111217. [58] BOUCHER PO, OZDEMIR RA, MOMI D, et al. Sham-derived effects and the minimal reliability of theta burst stimulation. Sci Rep. 2021;11(1):21170. [59] TANG Z, LIU T, LIU Y, et al. Different doses of intermittent theta burst stimulation for upper limb motor dysfunction after stroke: a study protocol for a randomized controlled trial. Front Neurosci. 2023;17:1259872. [60] STRAFELLA R, MOMI D, ZOMORRODI R, et al. Identifying neurophysiological markers of intermittent theta burst stimulation in treatment-resistant depression using transcranial magnetic stimulation-electroencephalography. Biol Psychiatry. 2023;94(6):454-465. [61] CAULFIELD KA, BROWN JC. The problem and potential of TMS’ infinite parameter space: a targeted review and road map forward. Front Psychiatry. 2022;13:867091. [62] EIBL T, SCHREY M, LIEBERT A, et al. Influence of clinical and tumor-specific factors on the resting motor threshold in navigated transcranial magnetic stimulation. Neurophysiol Clin. 2023;53(6):102920. [63] CAI G, XU J, DING Q, et al. Electroencephalography oscillations can predict the cortical response following theta burst stimulation. Brain Res Bull. 2024;208(3):110902. [64] STRUCKMANN W, BODEN R, GINGNELL M, et al. Modulation of dorsolateral prefrontal cortex functional connectivity after intermittent theta-burst stimulation in depression: combining findings from fNIRS and fMRI. Neuroimage Clin. 2022;34(2): 103028. [65] WANG J, ZHANG J, YU H, et al. Editorial: human machine interface-based neuromodulation solutions for neurorehabilitation. Front Neurosci. 2022; 16:987455. [66] WANG H, ZHENG H, WU H, et al. Behavior-dependent corticocortical contributions to imagined grasping: a BCI-triggered TMS study. IEEE Trans Neural Syst Rehabil Eng. 2022;31:519-529. [67] WEN Y, HAO X, CHEN X, et al. Theta-burst stimulation combined with virtual-reality reconsolidation intervention for methamphetamine use disorder: study protocol for a randomized-controlled trial. Front Psychiatry. 2022;13:903242. |
| [1] | Liang Haobo, Wang Zeyu, Ma Wenlong, Liu Hao, Liu Youwen. Hot issues in the field of joint revision: infection, rehabilitation nursing, bone defect, and prosthesis loosening [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1963-1971. |
| [2] | Lyu Liting, Yu Xia, Zhang Jinmei, Gao Qiaojing, Liu Renfan, Li Meng, Wang Lu. Bibliometric analysis of research process and current situation of brain aging and exosomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1457-1465. |
| [3] | Xie Liugang, Cui Shuke, Guo Nannan, Li Aoyu, Zhang Jingrui. Research hotspots and frontiers of stem cells for Alzheimer’s disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1475-1485. |
| [4] | Chang Jinxia, Liu Yufei, Niu Shaohui, Wang Chang, Cao Jianchun. Visualization analysis of macrophage polarization in tissue repair process [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1486-1496. |
| [5] | Zhang Shuai, Li Zichun, Xu Yihao, Xie Xiaofeng, Guo Zhongsheng, Zhao Qingyang. Effect of transcranial magneto-acousto-electrical stimulation on the plasticity of the prefrontal cortex network in mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1108-1117. |
| [6] | Li Huijun, Li Huangyan, Zhang Yeting. Physical activity and cognition in older adults: research hotspot and topic evolution [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1073-1080. |
| [7] | Dang Xiaowen, Huang Hailiang, Huang Lei, Wang Yajie . Research frontiers and hotspots of carbon nanomaterials in biomedical field over the past 10 years [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 752-760. |
| [8] | Ma Yucong, Ouyang Zhengzheng, Liu Xiaojie, Yang Sifei. Tracking of research trends and hotspots in medical magnesium alloy materials [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7470-7480. |
| [9] | Guo Haizhen, Cong Zidong, Zhao Yuke, Li Xiaofeng, Yu Lu, Qian Shule, Wang Runying, Du Wuxun. Development of patch clamp technology in the past 10 years: visual analysis based on CiteSpace and VOSviewer [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6717-6726. |
| [10] | Wang Xuesong, Wang Yue, Xu Yan, Zeng Wenhui, Lu Wenming, Tang Xingkun, Chen Wenjie, Ye Junsong. Brain-computer interface combined with different therapies for limb dysfunction in stroke patients: effectiveness and mechanism analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6538-6546. |
| [11] | Zhao Xiaoxuan, Liu Shuaiyi, Xing Zheng, Li Qingwen, Chu Xiaolei, Li Qi. Research hotspots and trends in application of tissue engineering in peripheral nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6591-6600. |
| [12] | Xu Qiang, Qin Jialin, Lian Zeshuang, Wang Aoting, Li Ding, Wang Ye, Wang Junfang. Visual analysis of hot spots and trends in the study of ligamentum flavum ossification [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 628-636. |
| [13] | Song Haoran, Zhang Yuqiang, Gu Na, Zhi Xiaodong, Wang Wei. Visualization analysis of artificial intelligence in bone trauma research based on Citespace [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 493-502. |
| [14] | Zheng Xiaodong, Gao Shan, Han Wenjin, Liu Lijun, Jia Menglong, Yu Longtan. Visual analysis of treatment of adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 645-653. |
| [15] | Liu Jian, Liu Qing, Huang Ye, Cao Guanglei, Liu Yuan, Song Qingpeng. Growth factors promote knee cartilage regeneration: a bibliometric analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6351-6359. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||