Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (19): 3992-3999.doi: 10.12307/2025.056
Previous Articles Next Articles
Effect of oxymatrine on expression of stem markers and osteogenic differentiation of periodontal ligament stem cells
Luo Jing1, 2, Yong Min3, Chen Qi3, Yang Changyi4, Zhao Tian3, Ma Jing3, Mei Donglan3, Hu Jinpeng1, Yang Zhaojun1, Wang Yuran1, Liu Bo1
- 1School of Stomatology, Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China; 2Key Laboratory of Stem Cell and Regenerative Medicine of Ningxia Hui Autonomous Region, Yinchuan 750004, Ningxia Hui Autonomous Region, China; 3Department of Orthodontics, General Hospital of Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China; 4Department of Periodontology, General Hospital of Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China
-
Received:2024-01-13Accepted:2024-04-03Online:2025-07-08Published:2024-09-12 -
Contact:Yong Min, Master, Associate professor, Chief physician, Department of Orthodontics, General Hospital of Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China -
About author:Luo Jing, Master candidate, School of Stomatology, Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China; Key Laboratory of Stem Cell and Regenerative Medicine of Ningxia Hui Autonomous Region, Yinchuan 750004, Ningxia Hui Autonomous Region, China -
Supported by:2021 First-Class Discipline Construction Project of Ningxia Medical University, No. 0019110104 (to YM); Science and Technology Benefit People Special Project of Ningxia Hui Autonomous Region, No. 2022CMG03029 (to YM)
CLC Number:
Cite this article
Luo Jing, Yong Min, Chen Qi, Yang Changyi, Zhao Tian, Ma Jing, Mei Donglan, Hu Jinpeng, Yang Zhaojun, Wang Yuran, Liu Bo. Effect of oxymatrine on expression of stem markers and osteogenic differentiation of periodontal ligament stem cells[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(19): 3992-3999.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

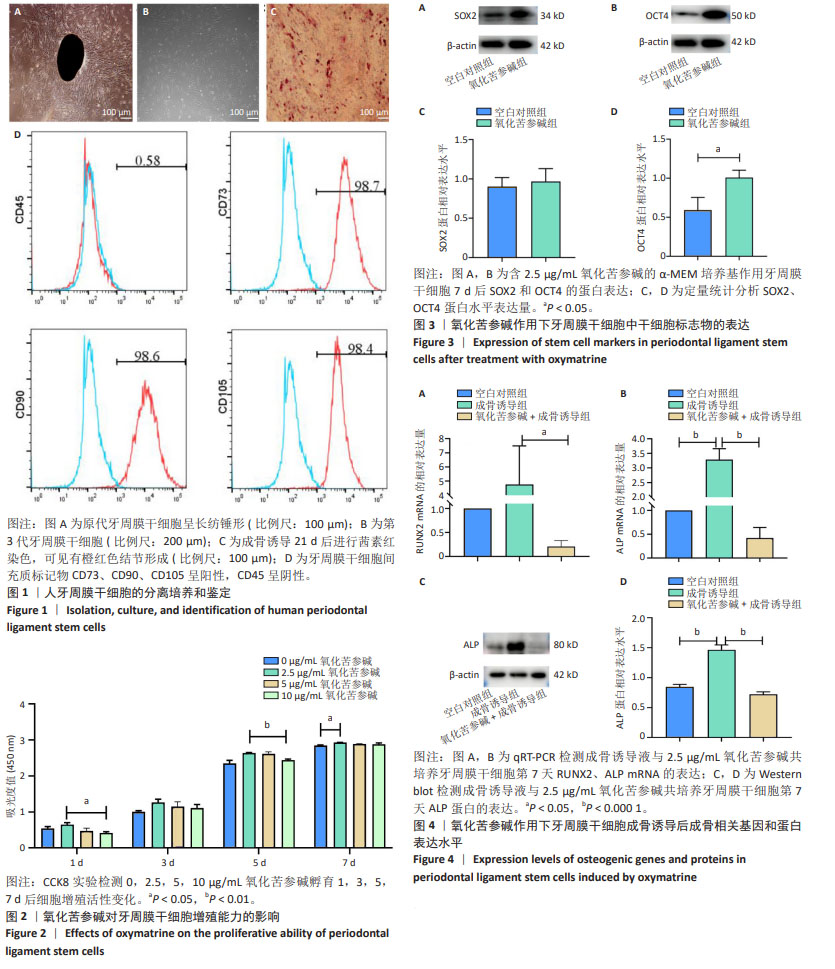
2.1 牙周膜干细胞形态、表面标志物表达及骨向分化能力鉴定 人牙周组织块在T25培养瓶内培养,5-7 d后在倒置显微镜下可见组织块周围长出纺锤形细胞,细胞排列稀疏不均匀,生长较慢,见图1A。第3代牙周膜干细胞在倒置显微镜下呈长梭形,生长较快,排列紧密,见图1B;第3代牙周膜干细胞成骨诱导21 d后进行茜素红染色,镜下可见培养板底部有橙红色结节形成,说明分离出来的细胞具有成骨分化能力,见图1C。流式细胞仪检测牙周膜干细胞阳性表达间充质干细胞表面标志物CD73、CD90、CD105;阴性表达白细胞共同抗原CD45,体现了间充质干细胞的干性特点,见图1D。 2.2 氧化苦参碱对牙周膜干细胞增殖能力的影响 CCK8实验检测0,2.5,5,10 μg/mL氧化苦参碱孵育1,3,5,7 d后细胞增殖活性变化,用于评估氧化苦参碱对牙周膜干细胞增殖能力的影响。如图2所示,随着时间的延长,各组细胞数量呈增加趋势。第1天时,10 μg/mL氧化苦参碱组细胞数量低于2.5 μg/mL氧化苦参碱组(P < 0.05);第3天时组间没有明显差异;第5天时,10 μg/mL氧化苦参碱组细胞数量低于2.5 μg/mL氧化苦参碱组(P < 0.01);第7天时,4组细胞生长趋势减缓,2.5 μg/mL氧化苦参碱组细胞数量高于0 μg/mL氧化苦参碱组(P < 0.05)。综上,初步选择低质量浓度2.5 μg/mL氧化苦参碱进行后续实验。 2.3 氧化苦参碱作用下牙周膜干细胞中干细胞标志物的表达 培养7 d后,采用Western blot检测空白对照组和氧化苦参碱组牙周膜干细胞中干细胞标志物SOX2和OCT4 的表达。由图3所示,氧化苦参碱组SOX2蛋白表达较空白对照组无明显变化(P > 0.05);与空白对照组相比,氧化苦参碱组OCT4蛋白表达明显上升,差异有显著性意义(P < 0.05)。 2.4 氧化苦参碱作用下牙周膜干细胞成骨诱导后成骨相关基因和蛋白表达水平 与空白对照组相比,成骨诱导组早期成骨基因ALP表达明显上调,表明牙周膜干细胞成骨分化诱导成功,由于培养时间短,故成骨诱导组中RUNX2基因表达差异不明显;与成骨诱导组相比,氧化苦参碱+成骨诱导组牙周膜干细胞成骨相关基因RUNX2(P < 0.05)、ALP(P < 0.000 1)表达明显降低,以上实验结果说明氧化苦参碱可以抑制牙周膜干细胞的成骨向分化,见图4A,B。同期,Western blot实验结果表明,成骨相关蛋白ALP的表达趋势与ALP成骨基因表达的趋势一样,即:与空白对照组相比,成骨诱导组早期成骨相关蛋白ALP表达水平明显上调(P < 0.000 1);与成骨诱导组相比,氧化苦参碱+成骨诱导组牙周膜干细胞成骨相关蛋白ALP的表达水平显著下降(P < 0.000 1),见图4C,D。"

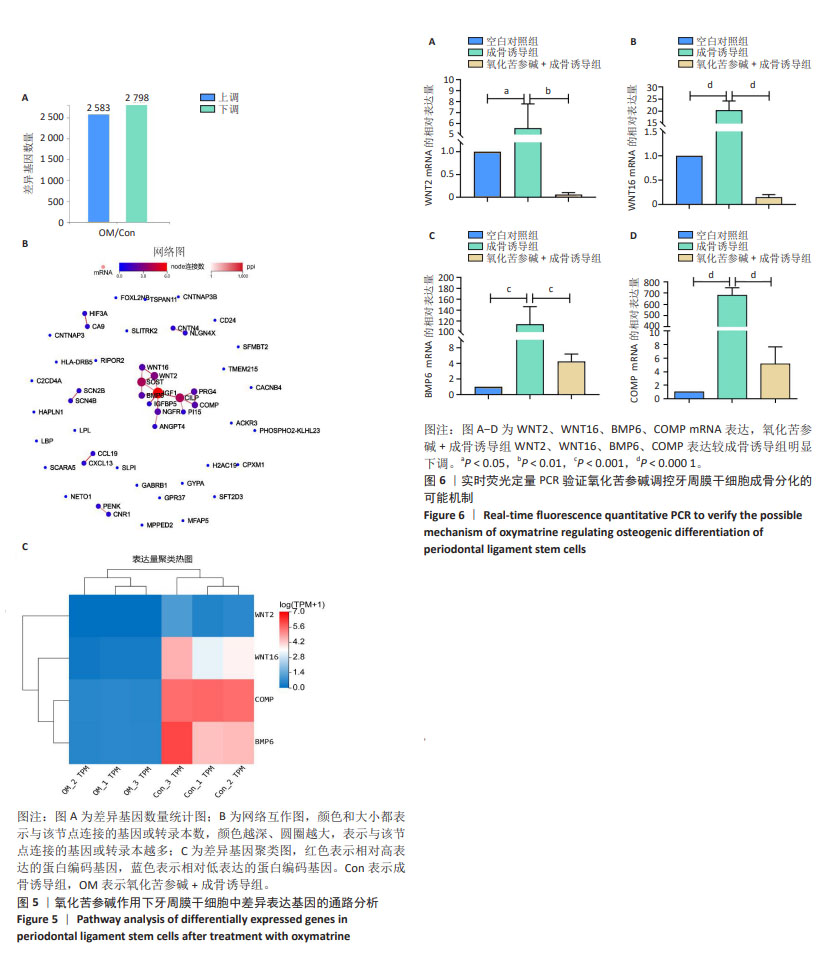
2.5 高通量测序分析氧化苦参碱对牙周膜干细胞成骨分化抑制的潜在机制 测序结果显示成骨诱导组、氧化苦参碱+成骨诱导组共表达5 381个差异基因,其中2 583个上调基因,2 798个下调基因,见图5A。对2 798个下调基因进行筛选,筛选条件为Q值(OM/Con) ≤ 0.05,并将Log2 (OM/Con)值升序排列,得到下调前50个基因,将这些基因进行网络互作分析,见图5B;检索国内外相关文献,从上述50个基因中挑选出调节间充质干细胞成骨的相关基因,以更好地了解氧化苦参碱对牙周膜干细胞成骨分化的影响,寻找潜在的可能机制,文献显示,调节间充质干细胞骨向分化信号通路中WNT2、WNT16、COMP、BMP6基因参与其中[22-25];利用聚类热图检测这4个基因在两组牙周膜干细胞的表达,根据两组样本的颜色对比,WNT16、COMP、BMP6在成骨诱导组和氧化苦参碱+成骨诱导组中颜色差异较WNT2大,说明在送检两组样本中WNT16、COMP、BMP6基因表达较WNT2差异更大,同时WNT2、WNT16、COMP、BMP6基因在氧化苦参碱+成骨诱导组中颜色偏蓝,表示这4个基因在该组中表达下调,见图5C。 2.6 PCR验证氧化苦参碱对牙周膜干细胞成骨分化抑制的潜在机制 图6A-D为选择WNT2、WNT16、BMP6、COMP这4个下调的mRNA进行实时荧光定量PCR验证,与空白对照组相比,成骨诱导组牙周膜干细胞中WNT2、WNT16、BMP6、COMP表达均明显增强,说明这些基因与牙周膜干细胞成骨分化呈正相关;氧化苦参碱+成骨诱导组WNT2、WNT16、BMP6、COMP表达较成骨诱导液组下调,表明氧化苦参碱负向调控牙周膜干细胞的骨向分化。"
| [1] ZHAO Z, LIU J, WEIR MD, et al. Periodontal ligament stem cell-based bioactive constructs for bone tissue engineering. Front Bioeng Biotechnol. 2022;10:1071472. [2] MERT S, MALYARAN H, CRAVEIRO RB, et al. Comparative analysis of proliferative and multilineage differentiation potential of human periodontal ligament stem cells from maxillary and mandibular molars. J Periodontol. 2023;94(7):882-895. [3] OSORIO MT, TOLEDANO R, HUANG H, et al. Effect of doxycycline doped nanoparticles on osteogenic/cementogenic and anti-inflammatory responses of human cells derived from the periodontal ligament. J Dent. 2023;137:104668. [4] ALHASAN MA, TOMOKIYO A, HAMANO S, et al. Hyaluronic Acid Induction Promotes the Differentiation of Human Neural Crest-like Cells into Periodontal Ligament Stem-like Cells. Cells. 2023;12(23):2743. [5] MROZIK KM, WADA N, MARINO V, et al. Regeneration of periodontal tissues using allogeneic periodontal ligament stem cells in an ovine model. Regen Med. 2013;8(6):711-723. [6] WANG W, WANG A, HU G, et al. Potential of an Aligned Porous Hydrogel Scaffold Combined with Periodontal Ligament Stem Cells or Gingival Mesenchymal Stem Cells to Promote Tissue Regeneration in Rat Periodontal Defects. ACS Biomater Sci Eng. 2023;9(4):1961-1975. [7] IWASAKI K, AKAZAWA K, NAGATA M, et al. The Fate of Transplanted Periodontal Ligament Stem Cells in Surgically Created Periodontal Defects in Rats. Int J Mol Sci. 2019;20(1):192. [8] FRANZEN J, GEORGOMANOLIS T, SELICH A, et al. DNA methylation changes during long-term in vitro cell culture are caused by epigenetic drift. Commun Biol. 2021;4(1):598. [9] XIE W, ZHANG Y, ZHANG S, et al. Oxymatrine enhanced anti-tumor effects of Bevacizumab against triple-negative breast cancer via abating Wnt/β-Catenin signaling pathway. Am J Cancer Res. 2019;9(8):1796-1814. [10] DING Y, LI N, SUN J, et al. Oxymatrine Inhibits Bocavirus MVC Replication, Reduces Viral Gene Expression and Decreases Apoptosis Induced by Viral Infection. Virol Sin. 2019;34(1):78-87. [11] YANG Y, SUN M, LI W, et al. Rebalancing TGF-β/Smad7 signaling via Compound kushen injection in hepatic stellate cells protects against liver fibrosis and hepatocarcinogenesis. Clin Transl Med. 2021;11(7):e410. [12] LI S, FENG G, ZHANG M, et al. Oxymatrine attenuates TNBS-induced colinutis in rats through TLR9/Myd88/NF-κB signal pathway. Hum Exp Toxicol. 2022;41:9603271221078866. [13] LUO R, XIE L, LIN Y, et al. Oxymatrine suppresses oral squamous cell carcinoma progression by suppressing CXC chemokine receptor 4 in an m6A modification decrease dependent manner. Oncol Rep. 2022;48(4):177. [14] WU Y, CHEN L, LUO K, et al. The effects of oxymatrine on expression of interleukin-6 and interleukin-1beta mRNA of human periodontal ligament cell stimulated by lipopolysaccharides. Hua Xi Kou Qiang Yi Xue Za Zhi. 2010;28(6):656-659. [15] YANG L, LU Y, ZHANG Z, et al. Oxymatrine boosts hematopoietic regeneration by modulating MAPK/ERK phosphorylation after irradiation-induced hematopoietic injury. Exp Cell Res. 2023;427(2):113603. [16] LI J, CAO Y, LI LN, et al. Neuroprotective Effects of Oxymatrine via Triggering Autophagy and Inhibiting Apoptosis Following Spinal Cord Injury in Rats. Mol Neurobiol. 2023;60(8):4450-4471. [17] IDA-YONEMOCHI H, OTSU K, IRIÉ T, et al. Loss of Autophagy Disrupts Stemness of Ameloblast-Lineage Cells in Aging. J Dent Res. 2024;103(2): 156-166. [18] JIANG C, MA Q, WANG S, et al. Oxymatrine Attenuates Osteoclastogenesis via Modulation of ROS-Mediated SREBP2 Signaling and Counteracts Ovariectomy-Induced Osteoporosis. Front Cell Dev Biol. 2021;9:684007. [19] ZHOU K, LIU D, JIN Y, et al. Oxymatrine ameliorates osteoarthritis via the Nrf2/NF-κB axis in vitro and in vivo. Chem Biol Interact. 2023;380:110539. [20] MOHETAER D, CAO L, WANG Y. Oxymatrine Protects Chondrocytes against IL-1β-triggered Apoptosis in Vitro and Inhibits Osteoarthritis in Mice Model. Evid Based Complement Alternat Med. 2022;2022:2745946. [21] JIANG Y, SANG W, WANG C, et al. Oxymatrine exerts protective effects on osteoarthritis via modulating chondrocyte homoeostasis and suppressing osteoclastogenesis. J Cell Mol Med. 2018;22(8):3941-3954. [22] LUO Y, DING X, JI H, et al. MicroRNA-503-3p affects osteogenic differentiation of human adipose-derived stem cells by regulation of Wnt2 and Wnt7b under cyclic strain. Stem Cell Res Ther. 2020;11(1):318. [23] HILDEBRANDT S, BASCHANT U, THIELE S, et al. Glucocorticoids suppress Wnt16 expression in osteoblasts in vitro and in vivo. Sci Rep. 2018;8(1): 8711. [24] CAI C, WANG J, HUO N, et al. Msx2 plays an important role in BMP6-induced osteogenic differentiation of two mesenchymal cell lines: C3H10T1/2 and C2C12. Regen Ther. 2020;14:245-251. [25] WU J, HU M, JIANG H, et al. Endothelial Cell-Derived Lactate Triggers Bone Mesenchymal Stem Cell Histone Lactylation to Attenuate Osteoporosis. Adv Sci (Weinh). 2023;10(31):e2301300. [26] CHOUDHERY MS. Strategies to improve regenerative potential of mesenchymal stem cells. World J Stem Cells. 2021;13(12):1845-1862. [27] YANG Y, LEE EH, YANG Z. Hypoxia-Conditioned Mesenchymal Stem Cells in Tissue Regeneration Application. Tissue Eng Part B Rev. 2022;28(5):966-977. [28] CHEN Y, ZHAO Q, YANG X, et al. Effects of cobalt chloride on the stem cell marker expression and osteogenic differentiation of stem cells from human exfoliated deciduous teeth. Cell Stress Chaperones. 2019;24(3):527-538. [29] YANG X, ZHAO Q, CHEN Y, et al. Effects of graphene oxide and graphene oxide quantum dots on the osteogenic differentiation of stem cells from human exfoliated deciduous teeth. Artif Cells Nanomed Biotechnol. 2019; 47(1):822-832. [30] CHE L, ZHU C, HUANG L, et al. Ginsenoside Rg2 Promotes the Proliferation and Stemness Maintenance of Porcine Mesenchymal Stem Cells through Autophagy Induction. Foods. 2023;12(5):1075. [31] LAN X, ZHAO J, ZHANG Y, et al. Oxymatrine exerts organ- and tissue-protective effects by regulating inflammation, oxidative stress, apoptosis, and fibrosis: From bench to bedside. Pharmacol Res. 2020;151:104541. [32] CHAI NL, XU SP, WAN J, et al. Oxymatrine could promote mesenchymal stem cell therapy in hepatic fibrosis rats: an experimental research. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2013;33(6):840-844. [33] SONG S, ZHOU J, WAN J, et al. Three-dimensional printing of microfiber- reinforced hydrogel loaded with oxymatrine for treating spinal cord injury. Int J Bioprint. 2023;9(3):692. [34] YANG Y, CHEN S, TAO L, et al. Inhibitory Effects of Oxymatrine on Transdifferentiation of Neonatal Rat Cardiac Fibroblasts to Myofibroblasts Induced by Aldosterone via Keap1/Nrf2 Signaling Pathways In Vitro. Med Sci Monit. 2019;25:5375-5388. [35] 陈凌,吴赟,骆凯,等.氧化苦参碱对内毒素作用下人牙周膜细胞增殖、细胞周期和超微结构的影响[J].中国生化药物杂志,2010,31(6):369-372. [36] YOON DS, KIM YH, JUNG HS, et al. Importance of Sox2 in maintenance of cell proliferation and multipotency of mesenchymal stem cells in low-density culture. Cell Prolif. 2011;44(5):428-440. [37] HAN D, WU G, CHEN R, et al. A balanced Oct4 interactome is crucial for maintaining pluripotency. Sci Adv. 2022;8(7):eabe4375. [38] BOROJEVIĆ A, JAUKOVIĆ A, KUKOLJ T, et al. Vitamin D3 Stimulates Proliferation Capacity, Expression of Pluripotency Markers, and Osteogenesis of Human Bone Marrow Mesenchymal Stromal/Stem Cells, Partly through SIRT1 Signaling. Biomolecules. 2022;12(2):323. [39] ZHU Z, RUAN S, JIANG Y, et al. α-Klotho released from HK-2 cells inhibits osteogenic differentiation of renal interstitial fibroblasts by inactivating the Wnt-β-catenin pathway. Cell Mol Life Sci. 2021;78(23):7831-7849. [40] QU X, LIAO M, LIU W, et al. Loss of Wnt16 Leads to Skeletal Deformities and Downregulation of Bone Developmental Pathway in Zebrafish. Int J Mol Sci. 2021;22(13):6673. [41] JIN Y, SUN X, PEI F, et al. Wnt16 signaling promotes osteoblast differentiation of periosteal derived cells in vitro and in vivo. PeerJ. 2020;8:e10374. [42] 付秋月,兰兴明,徐溶蔚,等.不同信号通路对牙周膜干细胞成骨分化的影响[J].中国组织工程研究,2023,27(24):3910-3919. [43] ZHU XY, DIAO S, YANG DM, et al. The Mechanism of GREM1’s Effect on Osteogenic/Odontogenic Differentiation of Stem Cells from Apical Papilla. Sichuan Da Xue Xue Bao Yi Xue Ban. 2021;52(3):409-415. [44] TOPRAK Ö, TOPUZ B, MONSEF YA, et al. BMP-6 carrying metal organic framework-embedded in bioresorbable electrospun fibers for enhanced bone regeneration. Mater Sci Eng C Mater Biol Appl. 2021;120:111738. [45] FREITAS J, MOURA SR, BARBOSA MA, et al. Long non-coding RNA CASC2 regulates osteoblasts matrix mineralization. Front Bioeng Biotechnol. 2023;11:1155596. |
| [1] | Chi Wenxin, Zhang Cunxin, Gao Kai, Lyu Chaoliang, Zhang Kefeng. Mechanism by which nobiletin inhibits inflammatory response of BV2 microglia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1321-1327. |
| [2] | Yu Ting, Lyu Dongmei, Deng Hao, Sun Tao, Cheng Qian. Icariin pretreatment enhances effect of human periodontal stem cells on M1-type macrophages [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1328-1335. |
| [3] | Hu Taotao, Liu Bing, Chen Cheng, Yin Zongyin, Kan Daohong, Ni Jie, Ye Lingxiao, Zheng Xiangbing, Yan Min, Zou Yong. Human amniotic mesenchymal stem cells overexpressing neuregulin-1 promote skin wound healing in mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1343-1349. |
| [4] | Liu Qi, Li Linzhen, Li Yusheng, Jiao Hongzhuo, Yang Cheng, Zhang Juntao. Icariin-containing serum promotes chondrocyte proliferation and chondrogenic differentiation of stem cells in the co-culture system of three kinds of cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1371-1379. |
| [5] | Aikepaer · Aierken, Chen Xiaotao, Wufanbieke · Baheti. Osteogenesis-induced exosomes derived from human periodontal ligament stem cells promote osteogenic differentiation of human periodontal ligament stem cells in an inflammatory microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1388-1394. |
| [6] | Zhao Zengbo, Li Chenxi, Dou Chenlei, Ma Na, Zhou Guanjun. Anti-inflammatory and osteogenic effects of chitosan/sodium glycerophosphate/sodium alginate/leonurine hydrogel [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 678-685. |
| [7] |
Li Yunzhe, Niu Zefan, Wang Zirou, Ai Chongyi, Chen Gang, Wang Xinxing.
Asperosaponin VI promotes osteogenic differentiation of MC3T3-E1 cells under hypoxia environment #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7481-7489.
|
| [8] | Liu Chengyuan, Guo Qianping. Differential effects of kartogenin on chondrogenic and osteogenic differentiation of rat and rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7490-7498. |
| [9] | Fang Yuan, Qian Zhiyong, He Yuanhada, Wang Haiyan, Sha Lirong, Li Xiaohe, Liu Jing, He Yachao, Zhang Kai, Temribagen. Mechanism of Mongolian medicine Echinops sphaerocephalus L. in proliferation and angiogenesis of vascular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7519-7528. |
| [10] | Shi Tongtong, Deng Rongxia, Zhang Jianguang. Differences in physicochemical properties and collagen secretion stimulation of natural and synthetic hydroxyapatite particles [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7278-7285. |
| [11] | Yin Hang, Song Kui. Effect of crocin hydrogel on chondrocytes and MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7293-7300. |
| [12] | Shao Xuekun, Shi Dianhua, Ding Zhiping, Qiu Zhuoya, Wang Ping, Wang Yi, Wang Cheng, Ding Xiaoyan, Sun Tiefeng. Calcined deer antler slices promote proliferation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6601-6608. |
| [13] | Lin Shuqian, Zhao Xilong, Gao Jing, Pan Xinghua, Li Zian, Ruan Guangping. Comparison of biological characteristics of mouse bone marrow mesenchymal stem cells after interference and overexpression of telomere Cajal body protein-1 [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6616-6624. |
| [14] | Wang Zhaoyan, Wang Qian, Liu Weipeng, Yang Hui, Luan Zuo, Qu Suqing. Effect of fibronectin on differentiation of human neural stem cells into oligodendrocyte precursor cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6661-6666. |
| [15] | Liu Haowen, Qiao Weiping, Meng Zhicheng, Li Kaijie, Han Xuan, Shi Pengbo. Regulation of osteogenic effects by bone morphogenetic protein/Wnt signaling pathway: revealing molecular mechanisms of bone formation and remodeling [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 563-571. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||