Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (19): 4172-4180.doi: 10.12307/2025.036
Cuproptosis-related genes in natural killer cells of Alzheimer’s disease
Chen Guilin, Tang Qiqiang
- Department of Neurology, Provincial Hospital Affiliated to Anhui Medical University, Hefei 230001, Anhui Province, China
-
Received:2024-01-02Accepted:2024-03-01Online:2025-07-08Published:2024-09-13 -
Contact:Tang Qiqiang, MD, Professor, Chief physician, Department of Neurology, Provincial Hospital Affiliated to Anhui Medical University, Hefei 230001, Anhui Province, China -
About author:Chen Guilin, Master candidate, Department of Neurology, Provincial Hospital Affiliated to Anhui Medical University, Hefei 230001, Anhui Province, China -
Supported by:Strategic Leading Science and Technology Project of Chinese Academy of Sciences (Class B), No. XDB39040400 (to TQQ)
CLC Number:
Cite this article
Chen Guilin, Tang Qiqiang. Cuproptosis-related genes in natural killer cells of Alzheimer’s disease[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(19): 4172-4180.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

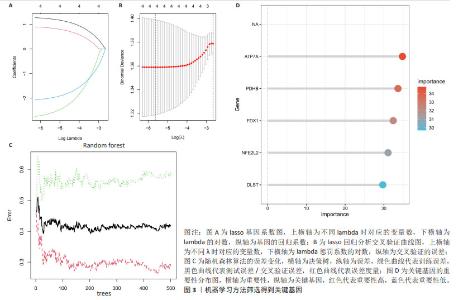
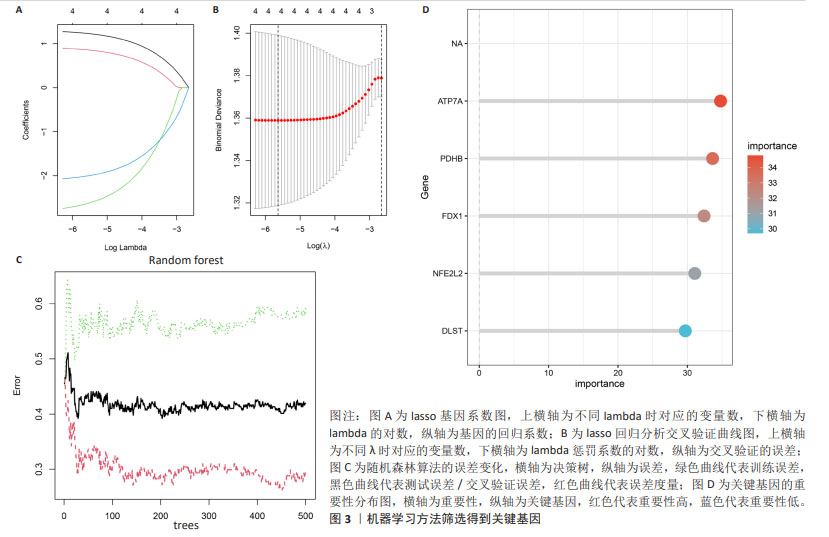
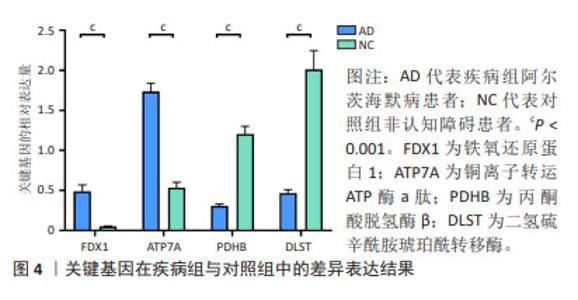
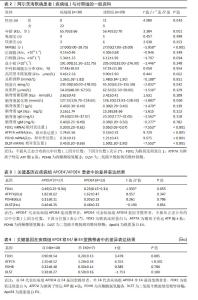
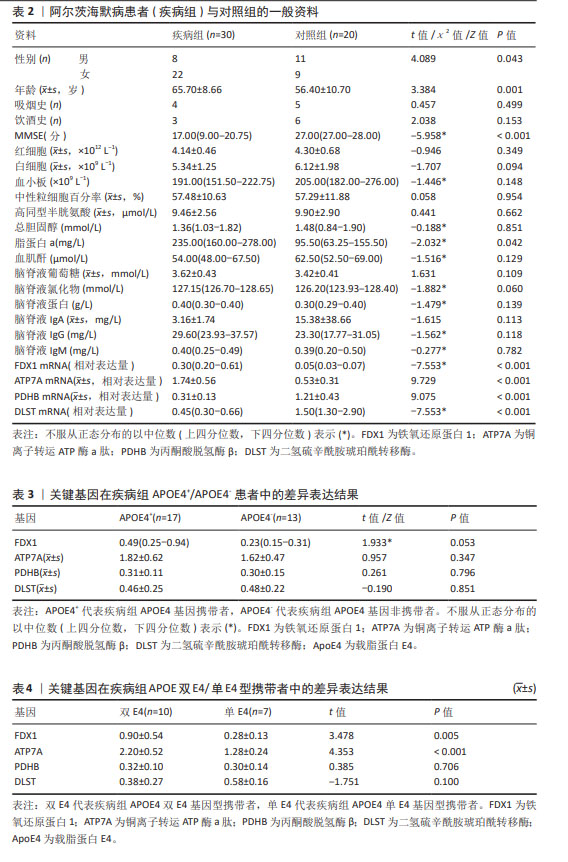
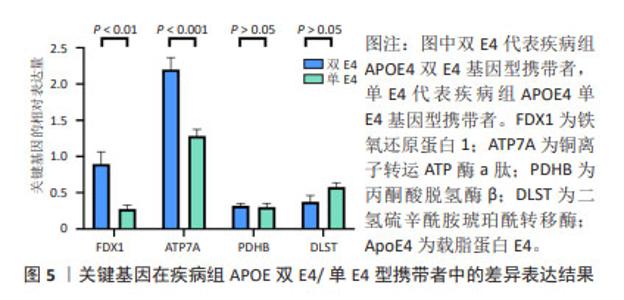
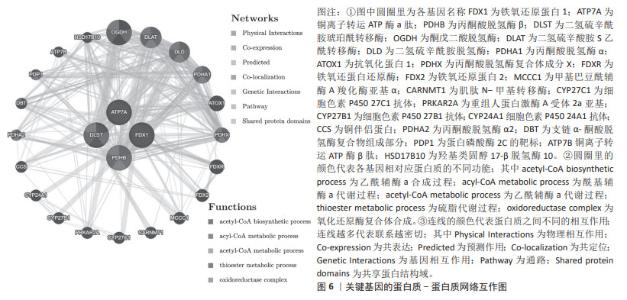
2.1 数据集信息及关键基因筛选结果 经仔细筛选后下载芯片编号为GSE63060(疾病组145例,对照组184例)原始文件,使用limma包对阿尔茨海默病患者及健康受试者外周血中差异基因进行分析,以P < 0.05,|logFC|>1作为条件筛选,共有21 684个基因符合要求,其中11 043个基因表达上调,10 641个基因表达下调,使用ggplot2包和pheatmap包绘制关键基因的火山图及热图见图1。将处理校正后的数据与收集到的铜死亡基因,以及阿尔茨海默病的单细胞数据集GSE168522(疾病组4例,对照组2例)中已报告过的NK细胞相关基因,进行交集筛选,共获得4个关键基因,绘制韦恩图见图2,其中FDX1和ATP7A在阿尔茨海默病中表达上调,DLST和PDHB在阿尔茨海默病中表达下调。"


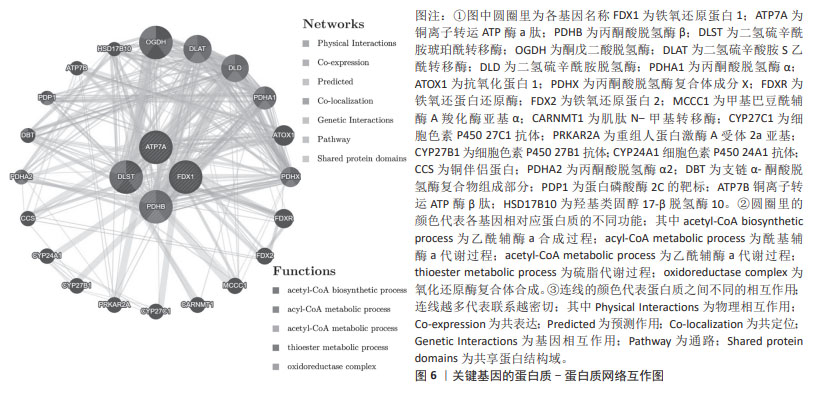
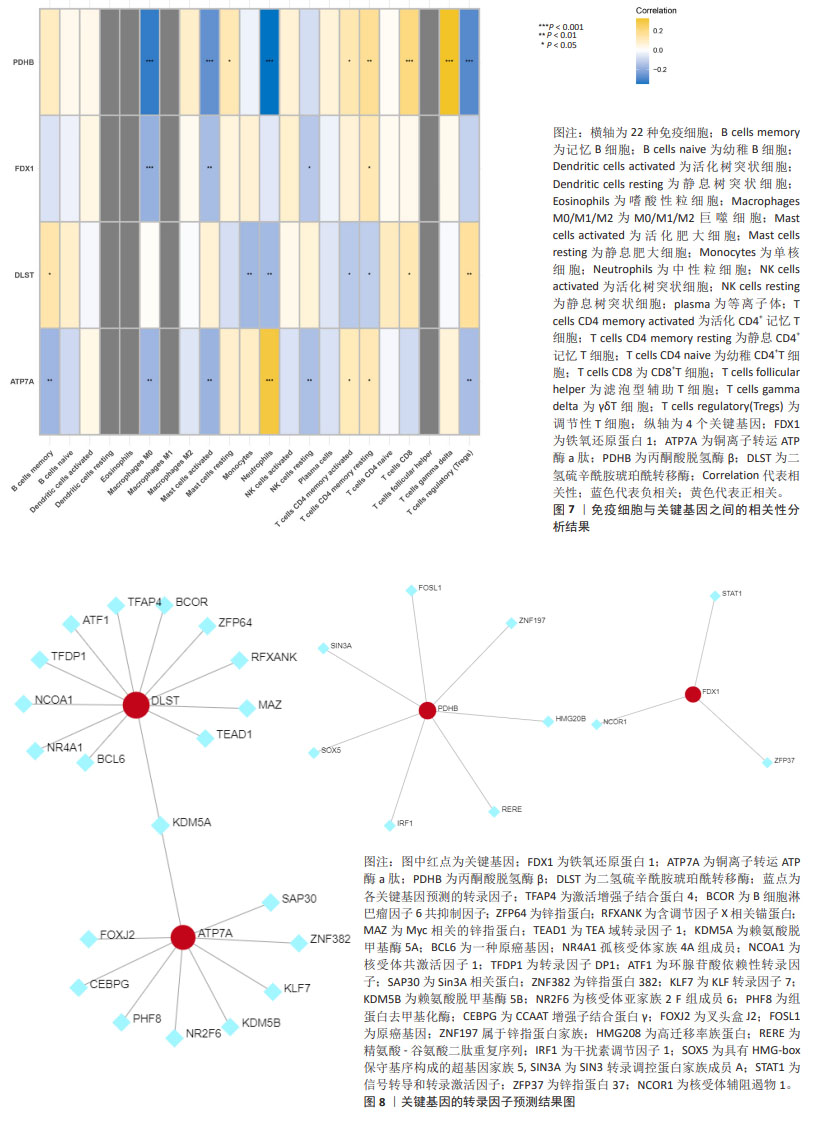
2.5 关键基因的免疫浸润差异 图7显示,在22个免疫细胞与关键基因的相关性分析中,FDX1,ATP7A,PDHB和DLST与12个免疫细胞具有显著相关性:PDHB与M0巨噬细胞、肥大细胞、中性粒细胞及调节性T细胞呈强负相关,与CD8+、滤泡型T细胞呈强正相关(P < 0.001);FDX1与M0巨噬细胞呈强负相关(P < 0.001);DLST与单核细胞、中性粒细胞呈负相关,与调节性T细胞呈正相关(P < 0.01);ATP7A与中性粒细胞呈强正相关(P < 0.001),其中NK细胞与ATP7A呈最强负相关(P < 0.01)。 2.6 关键基因的转录因子预测结果 基于ENCODE数据库预测与关键基因相关的转录因子,结果见图8。调控DLST的转录因子12个:BCL6,NR4A1,NCOA1,TFDP1,ATF1,TFAP4,BCOR,ZFP64,RFXANK,MAZ和TEAD1;调控ATP7A的转录因子9个:FOXJ2,CEBPG,PHF8,NR2F6,KDM5B,KLF7,ZNF382和SP30,二者共有的转录因子为KDM5A;调控PDHB的转录因子7个:FOSL1,ZNF197,HMG20B,RERE,IRF1,SOX5和SIN3A;调控FDX1的转录因子3个:STAT1,ZFP37和NCOR1。"
| [1] MATTHEWS KA, XU W, GAGLIOTI AH, et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015-2060) in adults aged ≥65 years. Alzheimers Dement. 2019;15(1):17-24. [2] BENILOVA I, KARRAN E, DE STROOPER B. The toxic Aβ oligomer and Alzheimer’s disease: an emperor in need of clothes. Nat Neurosci. 2012;15(3):349-57. [3] LU Y, LI K, HU Y, et al. Expression of immune related genes and possible regulatory mechanisms in Alzheimer’s disease. Front Immunol. 2021;12:768966. [4] LIU Z, LI H, PAN S. Discovery and validation of key biomarkers based on immune infiltrates in Alzheimer’s disease. Front Genet. 2021;12:658323. [5] ZHANG Y, FUNG ITH, SANKAR P, et al. Depletion of NK cells improves cognitive function in the Alzheimer disease mouse model. J Immunol. 2020;205(2):502-510. [6] JEVTIC S, SENGAR AS, SALTER MW, et al. The role of the immune system in Alzheimer disease: etiology and treatment. Ageing Res Rev. 2017;40:84-94. [7] WYATT-JOHNSON SK, BRUTKIEWICZ RR. The complexity of microglial interactions with innate and adaptive immune cells in Alzheimer’s disease. Front Aging Neurosci. 2020;12:592359. [8] MOYNIER F, CREECH J, DALLAS J, et al. Serum and brain natural copper stable isotopes in a mouse model of Alzheimer’s disease. Sci Rep. 2019;9(1):11894. [9] SQUITTI R, VENTRIGLIA M, SIMONELLI I, et al. Copper imbalance in Alzheimer’s disease: meta-analysis of serum, plasma, and brain specimens, and replication study evaluating ATP7B gene variants. Biomolecules. 2021;11(7):960. [10] TSVETKOV P, COY S, PETROVA B, et al. Copper induces cell death by targeting lipoylated TCA cycle proteins. Science. 2022;375(6586):1254-1261. [11] TANG D, CHEN X, KROEMER G. Cuproptosis: a copper-triggered modality of mitochondrial cell death. Cell Res. 2022; 32(5):417-418. [12] CHEN L, MIN J, WANG F. Copper homeostasis and cuproptosis in health and disease. Signal Transduct Target Ther. 2022;7(1):378. [13] NOBILI A, LATAGLIATA EC, VISCOMI MT, et al. Dopamine neuronal loss contributes to memory and reward dysfunction in a model of Alzheimer’s disease. Nat Commun. 2017; 8:14727. [14] PISOSCHI AM, POP A, IORDACHE F, et al. Oxidative stress mitigation by antioxidants – an overview on their chemistry and influences on health status. Eur J Med Chem. 2021;209:112891. [15] KALITA J, KUMAR V, MISRA UK, et al. Memory and learning dysfunction following copper toxicity: biochemical and immunohistochemical basis. Mol. Neurobiol. 2018;55:3800-3811. [16] LI X, CHEN X, GAO X. Copper and cuproptosis: new therapeutic approaches for Alzheimer’s disease. Front Aging Neurosci. 2023;15:1300405. [17] LAI Y, LIN C, LIN X, et al. Identification and immunological characterization of cuproptosis-related molecular clusters in Alzheimer’s disease. Front Aging Neurosci. 2022;14:932676. [18] ZHANG E, DAI F, CHEN T, et al. Diagnostic models and predictive drugs associated with cuproptosis hub genes in Alzheimer’s disease. Front Neurol. 2023;13:1064639. [19] ZOU Q, MROZEK D, MA Q, et al. Scalable data mining algorithms in computational biology and biomedicine. BioMed Res. Int. 2017;2017:5652041. [20] KOCH I, ANDRADE-NAVARRO M, SCHULZ MH, et al. Bioinformatics in theory and application - highlights of the 36th german conference on bioinformatics. J Biol Chem. 2021;402(8):869-870. [21] MCKHANN GM, KNOPMAN DS, CHERTKOW H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the national institute on aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263-269. [22] RITCHIE ME, PHIPSON B, WU D, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43(7):e47. [23] ENGEBRETSEN S, BOHLIN J. Statistical predictions with glmnet. Clin Epigenetics. 2019;11(1):123. [24] YILDIZ GULHAN P, EROZ R, ATAOGLU O, et al. The evaluation of both the expression and serum protein levels of Caspase-3 gene in patients with different degrees of SARS-CoV2 infection. J Med Virol. 2022;94(3):897-905. [25] LAM B, MASELLIS M, FREEDMAN M, et al. Clinical, imaging, and pathological heterogeneity of the Alzheimer’s disease syndrome. Alzheimers Res Ther. 2013; 5(1):1. [26] BYUN MS, KIM SE, PARK J, et al. Heterogeneity of regional brain atrophy patterns associated with distinct progression rates in Alzheimer’s disease. PLoS One. 2015;10(11):e0142756. [27] 郭佳旗,魏颖鸿,张慧,等.阿尔茨海默病发病机制及基于神经递质治疗的研究进展[J].医学综述,2021,27(19):3761-3766. [28] FENG D, ZHAO Y, LI W, et al. Copper neurotoxicity: induction of cognitive dysfunction: a review. Medicine (Baltimore). 2023;102(48):e36375. [29] GRINBERG AV, HANNEMANN F, SCHIFFLER B, et al. Adrenodoxin: structure, stability, and electron transfer properties. Proteins. 2000;40(4):590-612. [30] ZHANG Z, MA Y, GUO X,et al. FDX1 can impact the prognosis and mediate the metabolism of lung adenocarcinoma. Front Pharmacol. 2021;12:749134. [31] ZHANG J,KONG X,ZHANG Y,et al. FDXR regulates TP73 tumor suppressor via IRP2 to modulate aging and tumor suppression. J Pathol. 2020;251(3):284-296. [32] ZHANG Y, ZHOU Q, LU L, et al. Copper induces cognitive impairment in mice via modulation of cuproptosis and CREB signaling. Nutrients. 2023;15(4):972. [33] CHEN G, ZHANG J, TENG W, et al. FDX1 inhibits thyroid cancer malignant progression by inducing cuprotosis. Heliyon. 2023;9(8):e18655. [34] PETRIS MJ, MERCER JF, CULVENOR JG, et al. Ligand-regulated transport of the Menkes copper P-type ATPase efflux pump from the Golgi apparatus to the plasma membrane: a novel mechanism of regulated trafficking. EMBO J. 1996; 15(22):6084-6095. [35] YAMAGUCHI Y, HEINY ME, SUZUKI M, et al. Biochemical characterization and intracellular localization of the Menkes disease protein. Proc Natl Acad Sci U S A. 1996;93(24):14030-14035. [36] ZHENG Z, WHITE C, LEE J, et al. Altered microglial copper homeostasis in a mouse model of Alzheimer’s disease. J Neurochem. 2010;114(6):1630-1638. [37] CHEN L, HUANG D, ZHENG G, et al. Lead exposure aggravates Aβ1-42-induced microglial activation and copper ion accumulation in microglial cells. Nan Fang Yi Ke Da Xue Xue Bao. 2023;43(10): 1752-1760. [38] KEßLER M, BERGER IM, JUST S, et al. Loss of dihydrolipoyl succinyltransferase (DLST) leads to reduced resting heart rate in the zebrafish. Basic Res Cardiol. 2015;110(2):14. [39] KANAMSORI T, NISHIMAKI K, AOH S, et al. Truncated product of the bifunctional DLST gene involved in biogenesis of the respiratory chain. EMBO J. 2003;22(12): 2913-2923. [40] SCHULZ JB, LINDENAU J, SEYFRIED J, et al. Glutathione, oxidative stress and neurodegeneration. Eur J Biochem. 2000; 267(16):4904-4911. [41] CHEN W, ZHOU X, DUAN Y, et al. Association of OGG1 and DLST promoter methylation with Alzheimer’s disease in Xinjiang population. Exp Ther Med. 2018;16(4):3135-3142. [42] SOLMONSON A, DEBERARDINIS RJ. Lipoic acid metabolism and mitochondrial redox regulation. J Biol Chem. 2018;293(20): 7522-7530. [43] WANG H, YANG Z, HE X, et al. Cuproptosis related gene PDHB is identified as a biomarker inversely associated with the progression of clear cell renal cell carcinoma. BMC Cancer. 2023;23(1):804. [44] JIA D, WANG F, YU H. Systemic alterations of tricarboxylic acid cycle enzymes in Alzheimer’s disease. Front Neurosci. 2023;17:1206688. [45] KOMAI M, NODA Y, IKEDA A, et al. Nuclear SphK2/S1P signaling is a key regulator of ApoE production and Aβ uptake in astrocytes. J Lipid Res. 2024;25:100510. [46] STRITTMATTER WJ, SAUNDERS AM, SCHMECHEL D, et al. Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci U S A. 1993;90(5):1977-1981. [47] LIU Y, TAN Y, ZHANG Z, et al. The interaction between ageing and Alzheimer’s disease: insights from the hallmarks of ageing. Transl Neurodegener. 2024;13(1):7. [48] OVEISGHARAN S, ARVANITAKIS Z, YU L, et al. Sex differences in Alzheimer’s disease and common neuropathologies of aging. Acta Neuropathol. 2018;136(6):887-900. [49] BIECHELE G, RAUCHMANN BS, JANOWITZ D,et al. Associations between sex, body mass index and the individual microglial response in Alzheimer’s disease. J Neuroinflammation. 2024;21(1):30. [50] KAMSTRUP PR. Lipoprotein(a) and cardiovascular disease. Clin Chem. 2021; 67(1):154-166. [51] LARSSON SC, GILL D, MASON AM, et al. Lipoprotein(a) in Alzheimer, atherosclerotic, cerebrovascular, thrombotic, and valvular disease: mendelian randomization investigation. Circulation. 2020;141(22):1826-1828. [52] GONG J, HARRIS K, PETERS SAE, et al. Serum lipid traits and the risk of dementia: a cohort study of 254,575 women and 214,891 men in the UK Biobank. EClinicalMedicine. 2022;54:101695. |
| [1] | Deng Keqi, Li Guangdi, Goswami Ashutosh, Liu Xingyu, He Xiaoyong. Screening and validation of Hub genes for iron overload in osteoarthritis based on bioinformatics [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1972-1980. |
| [2] | Liu Lin, Liu Shixuan, Lu Xinyue, Wang Kan. Metabolomic analysis of urine in a rat model of chronic myofascial trigger points [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1585-1592. |
| [3] | Zhao Jiacheng, Ren Shiqi, Zhu Qin, Liu Jiajia, Zhu Xiang, Yang Yang. Bioinformatics analysis of potential biomarkers for primary osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1741-1750. |
| [4] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [5] | Zhang Haojun, Li Hongyi, Zhang Hui, Chen Haoran, Zhang Lizhong, Geng Jie, Hou Chuandong, Yu Qi, He Peifeng, Jia Jinpeng, Lu Xuechun. Identification and drug sensitivity analysis of key molecular markers in mesenchymal cell-derived osteosarcoma [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1448-1456. |
| [6] | Wang Mi, Ma Shujie, Liu Yang, Qi Rui. Identification and validation of characterized gene NFE2L2 for ferroptosis in ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1466-1474. |
| [7] | Xie Liugang, Cui Shuke, Guo Nannan, Li Aoyu, Zhang Jingrui. Research hotspots and frontiers of stem cells for Alzheimer’s disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1475-1485. |
| [8] |
Li Tian, Ren Yuhua, Gao Yanping, Su Qiang.
Mechanism of agomelatine alleviating anxiety- and depression-like behaviors in APP/PS1 transgenic mice #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1176-1182.
|
| [9] | Liu Yani, Yang Jinghuan, Lu Huihui, Yi Yufang, Li Zhixiang, Ou Yangfu, Wu Jingli, Wei Bing . Screening of biomarkers for fibromyalgia syndrome and analysis of immune infiltration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1091-1100. |
| [10] | Ma Weibang, Xu Zhe, Yu Qiao, Ouyang Dong, Zhang Ruguo, Luo Wei, Xie Yangjiang, Liu Chen. Screening and cytological validation of cartilage degeneration-related genes in exosomes from osteoarthritis synovial fluid [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7783-7789. |
| [11] | Jiang Qiyu, Zeng Huiyan. A novel analysis and prediction method for potential mechanisms of traditional Chinese medicine based on artificial intelligence and omics data-driven approach [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7552-7561. |
| [12] | Chen Ying, Guo Xiaojing, Mo Xueni, Ma Wei, Wu Shangzhi, Li Xiangling, Xie Tingting. Analysis of diagnostic biomarkers for ischemic stroke and experimental validation of targeted cuproptosis related genes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7562-7570. |
| [13] | Gong Yuehong, Wang Mengjun, Ren Hang, Zheng Hui, Sun Jiajia, Liu Junpeng, Zhang Fei, Yang Jianhua, Hu Junping. Machine learning combined with bioinformatics screening of key genes for pulmonary fibrosis associated with cellular autophagy and experimental validation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7679-7689. |
| [14] | Han Jie, Pan Chengzhen, Shang Yuzhi, Zhang Chi. Identification of immunodiagnostic biomarkers and drug screening for steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7690-7700. |
| [15] | Wang Kairu, Fu Shizhe, Li Jiahui, Yan Ru, Ma Yuru, Shi Bo, Ye Congyan , Yan Rui, Cong Guangzhi, Jia Shaobin. Spermidine/spermine N1-acetyltransferase 1 participates in vascular smooth muscle cell calcification [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6836-6842. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||