Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (31): 5036-5041.doi: 10.12307/2024.709
Previous Articles Next Articles
Intracranial transplantation of human bone marrow mesenchymal stem cells alleviates rat brain ischemia-reperfusion injury
Song Wenxue1, Liao Yidong1, Ming Jiang1, He Longcai1, Chen Guangtang1, Chen Chen1, Wang Zili1, Xiong Mingsong1, Cui Junshuan2, Xu Kaya2, 3
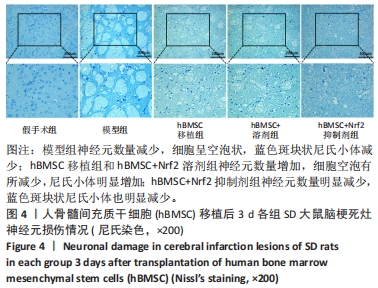
- 1Guizhou Medical University, Guiyang 550004, Guizhou Province, China; 2Department of Neurosurgery, 3Department of Hyperbaric Oxygen, Affiliated Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China
-
Received:2023-07-24Accepted:2023-10-12Online:2024-11-08Published:2024-01-22 -
Contact:Xu Kaya, MD, Chief physician, Department of Neurosurgery, Affiliated Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China; Department of Hyperbaric Oxygen, Affiliated Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
About author:Song Wenxue, Master candidate, Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
Supported by:National Natural Science Foundation of China, Nos. 81901173 and 82060231 (to XKY); Doctoral Research Start-up Fund Project of Affiliated Hospital of Guizhou Medical University, No. gyfybsky-2021-6 (to XKY); Cultivation Project Plan of National Natural Science Foundation of China in 2022, No. gyfynsfc-2022-08 (to XKY); Science and Technology Plan Project of Guizhou Province, No. ZK [2023] Key 039 (to XKY)
CLC Number:
Cite this article
Song Wenxue, Liao Yidong, Ming Jiang, He Longcai, Chen Guangtang, Chen Chen, Wang Zili, Xiong Mingsong, Cui Junshuan, Xu Kaya. Intracranial transplantation of human bone marrow mesenchymal stem cells alleviates rat brain ischemia-reperfusion injury[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(31): 5036-5041.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

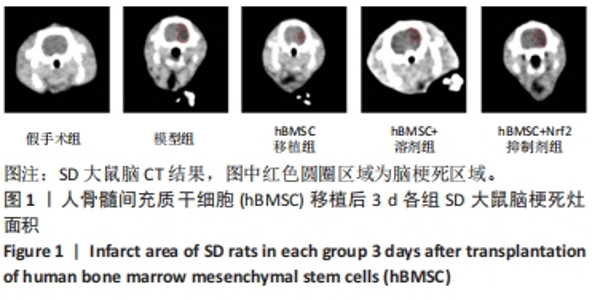
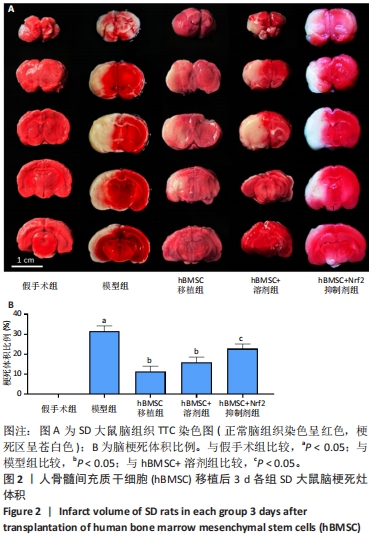
2.3 脑梗死灶体积 hBMSC移植后3 d,脑切片TTC染色显示模型组、hBMSC+溶剂组、hBMSC移植组和hBMSC+Nrf2抑制剂组均出现苍白色梗死灶,见图2A。通过Image J软件扫描脑片并计算梗死灶体积,与假手术组相比,模型组脑梗死体积增加(P < 0.05);与模型组相比,hBMSC移植组脑梗死体积减少(P < 0.05);hBMSC移植组与hBMSC+溶剂组无显著差异(P > 0.05);与hBMSC+溶剂组相比,hBMSC+Nrf2抑制剂组脑梗死体积增加(P < 0.05),见图2B。该结果提示颅内移植hBMSC有助于减少脑梗灶体积,而在抑制Nrf2表达后,颅内移植hBMSC改善脑梗灶体积的作用不明显。"

2.6 Western blot检测脑组织缺血区Nrf2、HO-1蛋白的表达 为了检测Nrf2/HO-1通路是否在该研究中存在作用,在脑组织缺血区观察Nrf2、HO-1蛋白的表达。如图5所示,与假手术组相比,模型组Nrf2和HO-1蛋白同时降低(均P < 0.05);与模型组相比,hBMSC移植组Nrf2和HO-1蛋白同时升高(均P < 0.05);hBMSC移植组和hBMSC+溶剂组无差异(P > 0.05);与hBMSC+溶剂组相比,hBMSC+Nrf2抑制剂组Nrf2和HO-1蛋白同时降低(均P < 0.05)。该结果表明Nrf2与HO-1蛋白表达存在一致性,抑制Nrf2蛋白表达相应会导致下游HO-1蛋白表达降低,提示Nrf2/HO-1通路的存在。"

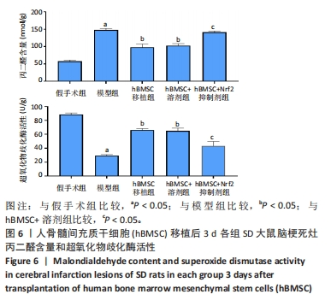
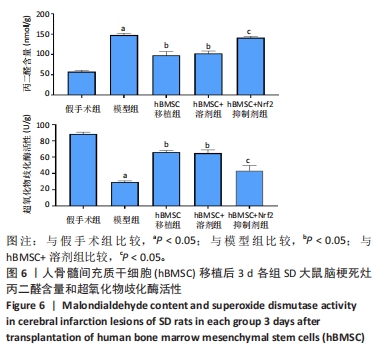
2.7 化学试剂盒检测脑组织氧化应激指标 为了探究hBMSC对MCAO大鼠缺血脑组织中氧化应激的抑制作用,分别检测了缺血区脑组织中丙二醛含量和超氧化物歧化酶活性。丙二醛的含量越高通常提示氧化应激损伤程度越高,而超氧化物歧化酶则相反。如图6所示,组内丙二醛和超氧化物歧化酶表达相反:与假手术组相比,模型组丙二醛升高而超氧化物歧化酶降低(均P < 0.05);与模型组相比,hBMSC移植组丙二醛降低而超氧化物歧化酶升高(均P < 0.05);hBMSC移植组和hBMSC+溶剂组无差异(P > 0.05);与hBMSC+溶剂组相比,hBMSC+Nrf2抑制剂组丙二醛升高而超氧化物歧化酶降低(均P < 0.05)。上述结果表明hBMSC具有通过Nrf2/HO-1通路改善MCAO大鼠脑组织氧化应激损伤的作用。"
| [1] WALTER K. What Is Acute Ischemic Stroke? JAMA. 2022;327(9):885. [2] SCHIAVONE S, TRABACE L. Small Molecules: Therapeutic Application in Neuropsychiatric and Neurodegenerative Disorders. Molecules. 2018;23(2):411. [3] ORELLANA-URZÚA S, ROJAS I, LÍBANO L, et al. Pathophysiology of Ischemic Stroke: Role of Oxidative Stress. Curr Pharm Des. 2020;26(34):4246-4260. [4] LIU L, LOCASCIO LM, DORÉ S. Critical Role of Nrf2 in Experimental Ischemic Stroke. Front Pharmacol. 2019;10:153. [5] LI Y, MENG F. Effects of icariside II on brain tissue oxidative stress and Nrf2/HO-1 expression in rats with cerebral ischemia-reperfusion injury1. Acta Cir Bras. 2019;34(2):e201900208. [6] XU L, GAO Y, HU M, et al. Edaravone dexborneol protects cerebral ischemia reperfusion injury through activating Nrf2/HO-1 signaling pathway in mice. Fundam Clin Pharmacol. 2022;36(5):790-800. [7] DUAN C, WANG H, JIAO D, et al. Curcumin Restrains Oxidative Stress of After Intracerebral Hemorrhage in Rat by Activating the Nrf2/HO-1 Pathway. Front Pharmacol. 2022;13:889226. [8] NIE P, BAI X, LOU Y, et al. Human umbilical cord mesenchymal stem cells reduce oxidative damage and apoptosis in diabetic nephropathy by activating Nrf2. Stem Cell Res Ther. 2021;12(1):450. [9] ZHAO D, YU W, XIE W, et al. Bone marrow-derived mesenchymal stem cells ameliorate severe acute pancreatitis by inhibiting oxidative stress in rats. Mol Cell Biochem. 2022;477(12):2761-2771. [10] YANG W, YANG Y, YANG JY, et al. Treatment with bone marrow mesenchymal stem cells combined with plumbagin alleviates spinal cord injury by affecting oxidative stress, inflammation, apoptotis and the activation of the Nrf2 pathway. Int J Mol Med. 2016;37(4):1075-1082. [11] 李洪亮,薛智慧,龙抗胜,等.线栓法制备MCAO模型大鼠的经验体会[J].中国中医急症,2014,23(12):2216-2219. [12] 潘杭,朱向情,何洁,等.骨髓间充质干细胞对衰老猕猴胸腺及脾脏结构和功能的影响[J].中国组织工程研究,2023,27(19):2953-2959. [13] 张小琴,赵优琴,黄莉莉,等.基于Keap-1/Nrf2/ARE信号通路探讨片仔癀改善MCAO大鼠氧化应激损伤的作用[J].中华中医药杂志,2022, 37(11):6466-6470. [14] MA S, ZHOU X, WANG Y, et al. MG53 protein rejuvenates hUC-MSCs and facilitates their therapeutic effects in AD mice by activating Nrf2 signaling pathway. Redox Biol. 2022;53:102325. [15] CHEN F, LIU J, LI FQ, et al. β2-Microglobulin exacerbates neuroinflammation, brain damage, and cognitive impairment after stroke in rats. Neural Regen Res. 2023;18(3):603-608. [16] ALLEN CL, BAYRAKTUTAN U. Oxidative stress and its role in the pathogenesis of ischaemic stroke. Int J Stroke. 2009;4(6):461-470. [17] SU XT, WANG L, MA SM, et al. Mechanisms of Acupuncture in the Regulation of Oxidative Stress in Treating Ischemic Stroke. Oxid Med Cell Longev. 2020; 2020:7875396. [18] MIAO R, LI J, MENG C, et al. Diet-Derived Circulating Antioxidants and Risk of Stroke: A Mendelian Randomization Study. Oxid Med Cell Longev. 2022; 2022:6457318. [19] FORRESTER SJ, KIKUCHI DS, HERNANDES MS, et al. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ Res. 2018;122(6):877-902. [20] SHEHJAR F, MAKTABI B, RAHMAN ZA, et al. Stroke: Molecular mechanisms and therapies: Update on recent developments. Neurochem Int. 2023;162: 105458. [21] ZHOU L, ZHU H, BAI X, et al. Potential mechanisms and therapeutic targets of mesenchymal stem cell transplantation for ischemic stroke. Stem Cell Res Ther. 2022;13(1):195. [22] CHUNG JW, CHANG WH, BANG OY, et al. Efficacy and Safety of Intravenous Mesenchymal Stem Cells for Ischemic Stroke. Neurology. 2021;96(7): e1012-e1023. [23] LEE J, CHANG WH, CHUNG JW, et al. Efficacy of Intravenous Mesenchymal Stem Cells for Motor Recovery After Ischemic Stroke: A Neuroimaging Study. Stroke. 2022;53(1):20-28. [24] CHEN H, ZHOU L. Treatment of ischemic stroke with modified mesenchymal stem cells. Int J Med Sci. 2022;19(7):1155-1162. [25] LEE S, KIM OJ, LEE KO, et al. Enhancing the Therapeutic Potential of CCL2-Overexpressing Mesenchymal Stem Cells in Acute Stroke. Int J Mol Sci. 2020;21(20):7795. [26] LIU C, YANG ZX, ZHOU SQ, et al. Overexpression of vascular endothelial growth factor enhances the neuroprotective effects of bone marrow mesenchymal stem cell transplantation in ischemic stroke. Neural Regen Res. 2023;18(6):1286-1292. [27] GERVOIS P, WOLFS E, RATAJCZAK J, et al. Stem Cell-Based Therapies for Ischemic Stroke: Preclinical Results and the Potential of Imaging-Assisted Evaluation of Donor Cell Fate and Mechanisms of Brain Regeneration. Med Res Rev. 2016;36(6):1080-1126. [28] ACOSTA SA, TAJIRI N, HOOVER J, et al. Intravenous Bone Marrow Stem Cell Grafts Preferentially Migrate to Spleen and Abrogate Chronic Inflammation in Stroke. Stroke. 2015;46(9):2616-2627. [29] ZHANG Y, DONG N, HONG H, et al. Mesenchymal Stem Cells: Therapeutic Mechanisms for Stroke. Int J Mol Sci. 2022;23(5):2550. [30] LI J, ZHANG Q, WANG W, et al. Mesenchymal stem cell therapy for ischemic stroke: A look into treatment mechanism and therapeutic potential. J Neurol. 2021;268(11):4095-4107. [31] CALIÓ ML, MARINHO DS, KO GM, et al. Transplantation of bone marrow mesenchymal stem cells decreases oxidative stress, apoptosis, and hippocampal damage in brain of a spontaneous stroke model. Free Radic Biol Med. 2014;70:141-154. [32] TAKAGI T, KITASHOJI A, IWAWAKI T, et al. Temporal activation of Nrf2 in the penumbra and Nrf2 activator-mediated neuroprotection in ischemia-reperfusion injury. Free Radic Biol Med. 2014;72:124-133. |
| [1] | Yang Yifeng, Ye Nan, Wang Lin, Guo Shuaicheng, Huang Jian. Signaling pathway of dexmedetomidine against ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1464-1469. |
| [2] | Yue Yun, Wang Peipei, Yuan Zhaohe, He Shengcun, Jia Xusheng, Liu Qian, Li Zhantao, Fu Huiling, Song Fei, Jia Menghui. Effects of croton cream on JNK/p38 MAPK signaling pathway and neuronal apoptosis in cerebral ischemia-reperfusion injury rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1186-1192. |
| [3] | Lou Guo, Zhang Yan, Fu Changxi. Role of endothelial nitric oxide synthase in exercise preconditioning-induced improvement of myocardial ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1283-1288. |
| [4] | Pan Xiaolong, Fan Feiyan, Ying Chunmiao, Liu Feixiang, Zhang Yunke. Effect and mechanism of traditional Chinese medicine on inhibiting the aging of mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1091-1098. |
| [5] | Ren Weiliang, Jiao Yongwei, Zhang Jian, Yang Liying, Yang Qi. Modulatory effect of resveratrol on oxidative stress and inflammatory factors in the joint fluid of rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5154-5158. |
| [6] | Li Yue, Qiao Hua. miRNA derived from mesenchymal stem cells and its derivatives in treatment of pathological scar [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(31): 5042-5047. |
| [7] | Cao Sheng, Kong Lingwei, Xu Kun, Sun Zhijie. Effect of gelatin methacryloyl hydrogel loaded with salvianolic acid B on intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 380-386. |
| [8] | Qian Longjie, Su Wenli, Zhu Wenxian, Wang Yixin. SRT1720, an activator of silent information regulator 1, alleviates acute traumatic brain injury in a rat model [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4447-4454. |
| [9] | Zhou Minghan, Zhang Hui, Zheng Xianbo, Xu Wuji. Significance of PI3K/Akt/HIF-1α signaling pathway expression in nucleus pulposus cells at different oxygen concentrations in delaying intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4491-4497. |
| [10] | Chen Chen, Zheng Runquan, Zhang Guichun. Effects of emodin on the proliferation, apoptosis and oxidative stress of chondrocytes in osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4528-4534. |
| [11] | Ma Jianglei, Zhang Huijie, Zhang Chenfang, Yang Xitong, Cheng Jianjie, Wang Guangming. Neuroprotective mechanism by which fenofibrate regulates superoxide dismutase 2 expression in transgenic C57BL/6J mice [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4547-4552. |
| [12] | Tao Jingwei, Zhou Jingya, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong, Fan Xiao. Effect and mechanism of tetramethylpyrazine regulating ferroptosis in rats with spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(26): 4158-4163. |
| [13] | Luo Shanchao, Tang Jiren. Effect of hesperetin on inflammatory degeneration of chondrocytes by inhibiting oxidative stress [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(26): 4184-4188. |
| [14] | Li Yanbing, Wang Jiwei, Liu Xiaoqin, Guo Minfang, Niu Xiaojie, Meng Tao, Su Qin, Wang Hanbin, Yang Lizhi, Ma Cungen, Yu Jiezhong. Regulatory effect of Ganoderma lucidum polysaccharides on H2O2-induced apoptosis and mitochondrial dysfunction in SH-SY5Y cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(25): 4041-4047. |
| [15] | He Bo, He Zhijun, Liu Tao, Ma Suilu, Wei Xiaotao, Wang Weiwei. Action mechanism and advantages of mesenchymal stem cells for treating flap ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(25): 4065-4071. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||