Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (33): 7181-7188.doi: 10.12307/2025.860
Previous Articles Next Articles
Percutaneous vertebroplasty via Kambin's triangle for treatment of osteoporotic compression fractures: evaluation of safety and effectiveness
Jiang Zehua, Du Wenjun, Ren Zhishuai, Cui Haojun, Zhu Rusen
- Department of Spine Surgery, Tianjin Union Medical Center, Tianjin 300121, China
-
Received:2024-08-09Accepted:2024-11-22Online:2025-11-28Published:2025-04-12 -
Contact:Zhu Rusen, Chief physician, Master’s supervisor, Department of Spine Surgery, Tianjin Union Medical Center, Tianjin 300121, China -
About author:Jiang Zehua, MS, Attending physician, Department of Spine Surgery, Tianjin Union Medical Center, Tianjin 300121, China -
Supported by:Tianjin Union Medical Center Research Fund, No. 2019JZPY08 (to JZH); Tianjin Municipal Health Commission Science and Technology Project (Youth Project), No. TJWJ2022QN040 (to RZS)
CLC Number:
Cite this article
Jiang Zehua, Du Wenjun, Ren Zhishuai, Cui Haojun, Zhu Rusen. Percutaneous vertebroplasty via Kambin's triangle for treatment of osteoporotic compression fractures: evaluation of safety and effectiveness[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7181-7188.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
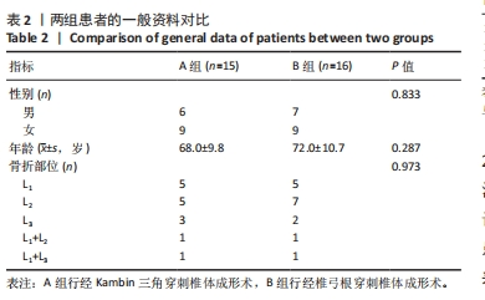
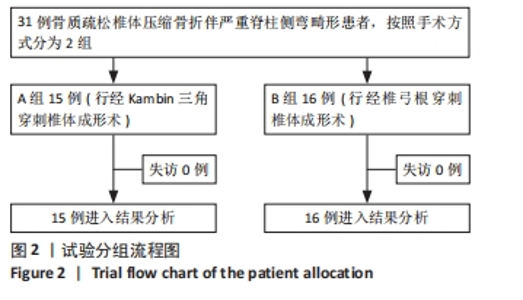
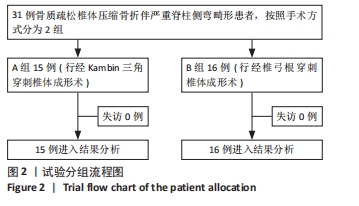
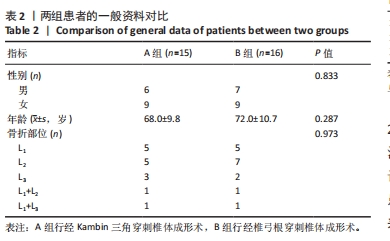
2.3 基线资料比较 如表2所示,A组患者男6例,女9例;B组患者男7例,女9例,两组性别构成比较无明显差异(Fisher精确检验,P > 0.999)。A组年龄平均(68.0±9.8)岁,B组平均(72.0±10.7)岁,两组年龄构成比较差异无显著性意义(t=1.083,P=0.287)。A组患者压缩骨折部位L1骨折5例,L2骨折5例,L3骨折3例,L1+L2 骨折1例,L1+L3 骨折1 例;B组患者压缩骨折部位L1 骨折5例,L2 骨折7例,L3 骨折2例,L1+L2骨折1例,L1+L3骨折1例,两组患者骨折部位构成比差异无显著性意义(χ2=0.501,P=0.973)。两组患者记录数据采用K-S检验结果sig > 0.05,满足正态分布条件。"
| [1] GIANGREGORIO LM, PAPAIOANNOU A, MACINTYRE NJ, et al. Too Fit To Fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int. 2014;25(3):821-835. [2] KENDLER DL, BAUER DC, DAVISON KS, et al. Vertebral Fractures: Clinical Importance and Management. Am J Med. 2016;129(2):221.e1-10. [3] LEE JT, KO MJ, LEE BJ, et al. Pain Intervention for Osteoporotic Compression Fracture, From Physical Therapy to Surgery: A Literature Review. Korean J Neurotrauma. 2024;20(3):159-167. [4] YANG EZ, XU JG, HUANG GZ, et al. Percutaneous Vertebroplasty Versus Conservative Treatment in Aged Patients With Acute Osteoporotic Vertebral Compression Fractures: A Prospective Randomized Controlled Clinical Study. Spine (Phila Pa 1976). 2016;41(8):653-660. [5] WANG B, GUO H, YUAN L, et al. A prospective randomized controlled study comparing the pain relief in patients with osteoporotic vertebral compression fractures with the use of vertebroplasty or facet blocking. Eur Spine J. 2016;25(11):3486-3494. [6] PARRY SM, PUTHUCHEARY ZA. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem Physiol Med. 2015; 4:16. [7] WANG Q, DONG JF, FANG X, et al. Application and modification of bone cement in vertebroplasty: A literature review. Jt Dis Relat Surg. 2022;33(2):467-478. [8] LIEBERMAN IH, TOGAWA D, KAYANJA MM. Vertebroplasty and kyphoplasty: filler materials. Spine J. 2005;5(6 Suppl):305S-316S. [9] BU BX, WANG MJ, LIU WF, et al. Short-segment posterior instrumentation combined with calcium sulfate cement vertebroplasty for thoracolumbar compression fractures: radiographic outcomes including nonunion and other complications. Orthop Traumatol Surg Res. 2015;101(2):227-233. [10] ZHAO S, XU CY, ZHU AR, et al. Comparison of the efficacy and safety of 3 treatments for patients with osteoporotic vertebral compression fractures: A network meta-analysis. Medicine (Baltimore). 2017;96(26):e7328. [11] RYU KS, HUH HY, JUN SC, et al. Single-balloon kyphoplasty in osteoporotic vertebral compression fractures: far-lateral extrapedicular approach. J Korean Neurosurg Soc. 2009;45(2):122-126. [12] LIU L, CHENG S, LU R, et al. Extrapedicular Infiltration Anesthesia as an Improved Method of Local Anesthesia for Unipedicular Percutaneous Vertebroplasty or Percutaneous Kyphoplasty. Biomed Res Int. 2016; 2016:5086414. [13] TAN G, LI F, ZHOU D, et al. Unilateral versus bilateral percutaneous balloon kyphoplasty for osteoporotic vertebral compression fractures-A systematic review of overlapping meta-analyses. Medicine (Baltimore). 2018;97(33):e11968. [14] CHENG X, LONG HQ, XU JH, et al. Comparison of unilateral versus bilateral percutaneous kyphoplasty for the treatment of patients with osteoporosis vertebral compression fracture (OVCF): a systematic review and meta-analysis. Eur Spine J. 2016;25(11):3439-3449. [15] HAIBIER A, YUSUFU A, LIN H, et al. Effect of different cement distribution in bilateral and unilateral Percutaneous vertebro plasty on the clinical efficacy of vertebral compression fractures. BMC Musculoskelet Disord. 2023;24(1):908. [16] KIM T, PARK J, CHO J, et al. Quantitative Comparison of Vertebral Structural Changes After Percutaneous Vertebroplasty Between Unilateral Extrapedicular Approach and Bilateral Transpedicular Approach Using Voxel-Based Morphometry. Neurospine. 2023;20(4): 1287-1302. [17] CHEN Y, ZHANG H, CHEN H, et al. Comparison of the effectiveness and safety of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100(51):e28453. [18] RINGER AJ, BHAMIDIPATY SV. Percutaneous access to the vertebral bodies: a video and fluoroscopic overview of access techniques for trans-, extra-, and infrapedicular approaches. World Neurosurg. 2013; 80(3-4):428-435. [19] HAIBIER A, YUSUFU A, LIN H, et al. Effect of different cement distribution in bilateral and unilateral Percutaneous vertebro plasty on the clinical efficacy of vertebral compression fractures. BMC Musculoskelet Disord. 2023;24(1):908. [20] SI L, WINZENBERG TM, JIANG Q, et al. Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos Int. 2015; 26(7):1929-1937. [21] BEALL DP, PARSONS B, BURNER S. Technical Strategies and Anatomic Considerations for an Extrapedicular Modified Inferior Endplate Access to Thoracic and Lumbar Vertebral Bodies. Pain Physician. 2016; 19(8):593-601. [22] LIU L, CHENG S, WANG Q, et al. An anatomical study on lumbar arteries related to the extrapedicular approach applied during lumbar PVP (PKP). PLoS One. 2019;14(3):e0213164. [23] HEO DH, CHO YJ. Segmental artery injury following percutaneous vertebroplasty using extrapedicular approach. J Korean Neurosurg Soc. 2011;49(2):131-133. [24] OZER AF, SUZER T, CAN H, et al. Anatomic Assessment of Variations in Kambin’s Triangle: A Surgical and Cadaver Study. World Neurosurg. 2017;100:498-503. [25] WAGUIA R, GUPTA N, GAMEL KL, et al. Current and Future Applications of the Kambin’s Triangle in Lumbar Spine Surgery. Cureus. 2022;14(6): e25686. [26] LIU Y, WANG B, LONG Y, et al. Extrapedicular unilateral percutaneous vertebroplasty via transverse process for osteoporotic vertebral compression fractures of upper lumbar. Chin J Trauma. 2018;34(4): 312-318. [27] MOLLOY S, MATHIS JM, BELKOFF SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976). 2003;28(14):1549-1554. [28] MATTIE R, LAIMI K, YU S, et al. Comparing Percutaneous Vertebroplasty and Conservative Therapy for Treating Osteoporotic Compression Fractures in the Thoracic and Lumbar Spine: A Systematic Review and Meta-Analysis. J Bone Joint Surg Am. 2016;98(12):1041-1051. [29] KWON HM, LEE SP, BAEK JW, et al. Appropriate Cement Volume in Vertebroplasty: A Multivariate Analysis with Short-Term Follow-Up. Korean J Neurotrauma. 2016;12(2):128-134. [30] MOLLOY S, MATHIS JM, BELKOFF SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976). 2003;28(14):1549-1554. [31] SUN HB, JING XS, LIU YZ, et al. The Optimal Volume Fraction in Percutaneous Vertebroplasty Evaluated by Pain Relief, Cement Dispersion, and Cement Leakage: A Prospective Cohort Study of 130 Patients with Painful Osteoporotic Vertebral Compression Fracture in the Thoracolumbar Vertebra. World Neurosurg. 2018;114:e677-e688. [32] CHENG X, LONG HQ, XU JH, et al. Comparison of unilateral versus bilateral percutaneous kyphoplasty for the treatment of patients with osteoporosis vertebral compression fracture (OVCF): a systematic review and meta-analysis. Eur Spine J. 2016;25(11): 3439-3449. [33] WIDMER SOYKA RP, HELGASON B, HAZRATI MARANGALOU J, et al. The Effectiveness of Percutaneous Vertebroplasty Is Determined by the Patient-Specific Bone Condition and the Treatment Strategy. PLoS One. 2016;11(4):e0151680. [34] SUN Y, LI X, MA S, et al. Comparison of the efficacy and safety of unilateral and bilateral approach kyphoplasty in the treatment of osteoporotic vertebral compression fractures: A meta-analysis. Jt Dis Relat Surg. 2024;35(3):491-503. [35] ZHAN Y, JIANG J, LIAO H, et al. Risk Factors for Cement Leakage After Vertebroplasty or Kyphoplasty: A Meta-Analysis of Published Evidence. World Neurosurg. 2017;101:633-642. [36] HONG SJ, LEE S, YOON JS, et al. Analysis of intradiscal cement leakage during percutaneous vertebroplasty: multivariate study of risk factors emphasizing preoperative MR findings. J Neuroradiol. 2014;41(3): 195-201. [37] COSAR M, SASANI M, OKTENOGLU T, et al. The major complications of transpedicular vertebroplasty. J Neurosurg Spine. 2009;11(5): 607-613. [38] YALTIRIK K, ASHOUR AM, REIS CR, et al. Vertebral augmentation by kyphoplasty and vertebroplasty: 8 years experience outcomes and complications. J Craniovertebr Junction Spine. 2016;7(3):153-160. [39] LIM JB, PARK JS, KIM E. Nonaneurysmal subarachnoid hemorrhage: rare complication of vertebroplasty. J Korean Neurosurg Soc. 2009; 45(6):386-389. [40] BAEK IH, PARK HY, KIM KW, et al. Paraplegia due to intradural cement leakage after vertebroplasty: a case report and literature review. BMC Musculoskelet Disord. 2021;22(1):741. [41] TSAI YD, LILIANG PC, CHEN HJ, et al. Anterior spinal artery syndrome following vertebroplasty: a case report. Spine (Phila Pa 1976). 2010; 35(4):E134-E136. [42] BIRKENMAIER C, SEITZ S, WEGENER B, et al. Acute paraplegia after vertebroplasty caused by epidural hemorrhage. A case report. J Bone Joint Surg Am. 2007;89(8):1827-1831. [43] XIE S, CUI L, WANG C, et al. Contact between leaked cement and adjacent vertebral endplate induces a greater risk of adjacent vertebral fracture with vertebral bone cement augmentation biomechanically. Spine J. 2024:S1529-9430(24)01034-9. [44] ZHAO Z, WANG R, GAO L, et al. Pulmonary embolism and intracardiac foreign bodies caused by bone cement leakage: a case report and literature review. J Cardiothorac Surg. 2024;19(1):544. [45] NIEUWENHUIJSE MJ, VAN ERKEL AR, DIJKSTRA PD. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J. 2011;11(9):839-848. [46] WU Y, XU LJ. Incidence of Cement Leakage and Potential Risk Factors in Surgery for Spinal Metastasis: A Systematic Review and Meta-Analysis. World Neurosurg. 2024;184:e95-e110. [47] ZHU D, HU JN, WANG L, et al. A Modified Unilateral Extrapedicular Approach Applied to Percutaneous Kyphoplasty to Treat Lumbar Osteoporotic Vertebral Compression Fracture: A Retrospective Analysis. Pain Physician. 2023;26(3):E191-E201. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Jing Ruyi, Chen Yingxin, Cao Lei . Prognosis of deep lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1626-1633. |
| [3] | Zhang Lichuang, Yang Wen, Ding Guangjiang, Li Peikun, Xiao Zhongyu, Chen Ying, Fang Xue, Zhang Teng. Dispersion effect of bone cement after vertebroplasty using individualized unilateral external pedicle approach and bilateral pedicle approach [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 800-808. |
| [4] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| [5] | Wang Rongqiang, Yang Liu, Wu Xiangkun, Shang Lilin. Analysis of factors associated with prognosis of osteoporosis patients after hip arthroplasty and construction of Nomogram prediction model [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7137-7142. |
| [6] | Abuduainijiang·Abulimiti, Alimu·Mamuti, Li Simi. Artificial femoral head replacement for femoral neck fracture in the elderly: validation of a risk prediction model for hip dysfunction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7143-7149. |
| [7] | Liu Ning, Sun Yingjin, Huang Long, Feng Shuo, Chen Xiangyang. Optimal rotational alignment of the tibial component during Oxford unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7158-7164. |
| [8] | Yang Wanzhong, Ma Rong, Guo Wei, Wang Zhiqiang, Yang Wei, Chen Zhen, Wang Zemin, Zhang Honglai, Ge Zhaohui. One-stage posterior hemivertebra resection and pedicle screw fixation in treatment of congenital scoliosis: a 2-year follow-up of correction effect [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7173-7180. |
| [9] | Yan Jinlian, Xu Zhengquan, Wei Renjie, Wang Yehua. Hip joint function recovery and prediction model construction after proximal femoral nail antirotation for intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7189-7195. |
| [10] | Cao Yong, Li Xin, Chen Zhigang, Gu Honglin, Lyu Shujun. Compensatory alignment changes of cervical and thoracic spine after correction of lumbar degenerative scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7196-7202. |
| [11] | Liang Jiachang, Guan Hua, Feng Enhui, Chen Pu, Huang Weiming, He Jianbo, Xie Jiewei. Ilizarov technique for treatment of congenital brachymetatarsia of the fourth: subgroup analysis of prolongation ratio [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7217-7222. |
| [12] | Liao Qiyu, Ru Jiangying. Complications of intra-prosthetic dissociation after hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7241-7249. |
| [13] | Zhao Yihan, Sun Xuhang, Zhao Lin, Jiang Shiqing. Effects and mechanisms of exosomal miRNA in treatment of multiple myeloma [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6743-6752. |
| [14] | Zhao Xingcheng, Wang Jun, Lu Ming. Repair strategies for nonunion in old osteoporotic vertebral compression fractures: a case analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 538-546. |
| [15] | Shi Lei, Shi Song, Lu Yue, Tao Ran, Ma Hongdong. Comparison of unicondylar knee arthroplasty and high tibial osteotomy in treatment of medial knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 503-509. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||