[1] MCCLOSKEY E, TAN ATH, SCHINI M. Update on fracture risk assessment in osteoporosis. Curr Opin Endocrinol Diabetes Obes. 2024;31(4):141-148.
[2] 丁一,李玉民,韩晓斌,等.个性化快速康复外科理念管理方案在微创防旋型股骨近端髓内钉治疗高龄股骨粗隆间骨折中的应用[J].中国临床医生杂志,2022,50(4):468-471.
[3] 陈夏平,吴天然,敖庆芳,等.PFNA内固定治疗股骨粗隆间骨折常见并发症的原因及应对策略[J].中国骨与关节损伤杂志,2023,38(12):1270-1274.
[4] KWAK DK, LEE S, LEE KU, et al. Incidence and Risk Factors of Osteonecrosis of the Femoral Head after Cephalomedullary Nailing for Pertrochanteric Fractures: Observational Single-Center Study. Clin Orthop Surg. 2024;16(3): 397-404.
[5] CHANG SM, HOU ZY, HU SJ, et al. Intertrochanteric Femur Fracture Treatment in Asia: What We Know and What the World Can Learn. Orthop Clin North Am. 2020;51(2):189-205.
[6] HEIDEN JJ, GOODIN SR, MORMINO MA, et al. Early Ambulation After Hip Fracture Surgery Is Associated With Decreased 30-Day Mortality. J Am Acad Orthop Surg. 2021;29(5):e238-e242.
[7] CHENG YX, SHENG X. Optimal surgical methods to treat intertrochanteric fracture: a Bayesian network meta-analysis based on 36 randomized controlled trials. J Orthop Surg Res. 2020;15(1):402.
[8] GHASEMI F, ESMAEILNEJAD-GANJI SM, MANAFI RASI A, et al. Evaluation of quality of life and associated factors in patients with intertrochanteric femoral fracture. PLoS One. 2023;18(11):e0293686.
[9] SOCCI AR, CASEMYR NE, LESLIE MP, et al. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99-B(1):128-133.
[10] GU J, HE S, WANG L. Analysis of one-year postoperative mortality and risk factors of elderly patients with intertrochanteric fractures after PFNA. Niger J Clin Pract. 2022;25(9):1557-1562.
[11] 郭天庆,薛飞,冯卫. 股骨转子间骨折不同外侧壁分型的内固定治疗策略[J].中国组织工程研究,2020,24(6):917-923.
[12] ZHENG L, WONG DW, CHEN X, et al. Risk of proximal femoral nail antirotation (PFNA) implant failure upon different lateral femoral wall thickness in intertrochanteric fracture: a finite element analysis. Comput Methods Biomech Biomed Engin. 2022;25(5):512-520.
[13] HU J, XIE K, WU S, et al. Osteoporosis and Fracture Risk Associated with Novel Antidepressants: A Systematic Review and Meta-Analysis. Actas Esp Psiquiatr. 2024;52(3):334-346.
[14] LING L, QU Z, ZHOU K. Effect of Fracture Reduction with Different Medial Cortical Support on Stability After Cephalomedullary Nail Fixation of Unstable Pertrochanteric Fractures: A Biomechanical Analysis. Indian J Orthop. 2021;56(1):34-40.
[15] 武英楷,王瑞强,宁尚攀,等.股骨近端防旋髓内钉固定股骨粗隆间骨折失败的因素[J].中国矫形外科杂志,2022,30(22):2050-2054.
[16] T J, KWEK EBK. Are Intertrochanteric Fractures Evolving? Trends in the Elderly Population over a 10-Year Period. Clin Orthop Surg. 2022;14(1):13-20.
[17] SHU WB, ZHANG XB, LU HY, et al. Comparison of effects of four treatment methods for unstable intertrochanteric fractures: A network meta-analysis. Int J Surg. 2018;60:173-181.
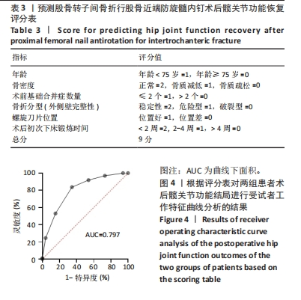
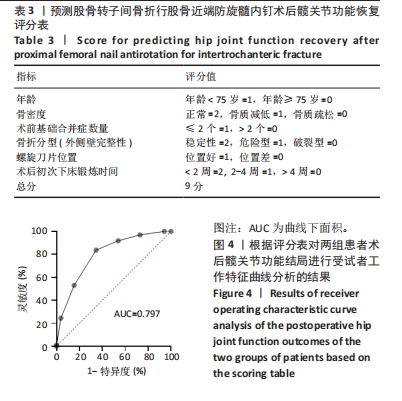
[18] PHRUETTHIPHAT OA, PINIJPRAPA P, SATRAVAHA Y, et al. An innovative scoring system for predicting an excellent Harris hip score after proximal femoral nail anti-rotation in elderly patients with intertrochanteric fracture. Sci Rep. 2022;12(1):19939.
[19] BODDAERT J, NA N, LE MANACH Y, et al. Prediction of postoperative mortality in elderly patients with hip fracture: are specific and geriatric scores better than general scores? Br J Anaesth. 2017;118(6):952-954.
[20] CHENG C, SHOBACK D. Mechanisms Underlying Normal Fracture Healing and Risk Factors for Delayed Healing. Curr Osteoporos Rep. 2019;17(1):36-47.
[21] HAYES WC, MYERS ER, ROBINOVITCH SN, et al. Etiology and prevention of age-related hip fractures. Bone. 1996;18(1 Suppl):77S-86S.
[22] TARANTINO U, CEROCCHI I, SCIALDONI A, et al. Bone healing and osteoporosis. Aging Clin Exp Res. 2011;23(2 Suppl):62-64.
[23] FOSTER AL, MORIARTY TF, ZALAVRAS C, et al. The influence of biomechanical stability on bone healing and fracture-related infection: the legacy of Stephan Perren. Injury. 2021;52(1):43-52.
[24] HAK DJ. The biology of fracture healing in osteoporosis and in the presence of anti-osteoporotic drugs. Injury. 2018;49(8):1461-1465.
[25] KITCHARANANT N, ATTHAKOMOL P, KHORANA J, et al. Prognostic Factors for Functional Recovery at 1-Year Following Fragility Hip Fractures. Clin Orthop Surg. 2024;16(1):7-15.
[26] SHI Z, QIANG M, JIA X, et al. Association of the lateral wall integrity with clinical outcomes in older patients with intertrochanteric hip fractures treated with the proximal femoral nail anti-rotation-Asia. Int Orthop. 2021; 45(12):3233-3242.
[27] 周龙,王亮,徐锐,等.股骨转子间骨折不同外侧壁分型髓内钉治疗的有限元分析[J].中国组织工程研究,2023,27(29):4652-4657.
[28] HUANG C, XU W, YE X, et al. Changes in nail position and antirotation blade angles on the risk of femoral head varus in PFNA fixed patients: a clinical review and comprehensive biomechanical research. Eur J Med Res. 2024;29(1):336.
[29] ZENG J, YE J, XIE Y, et al. Effect of screw blade position on proximal femoral nail anti-rotation internal fixation for unstable intertrochanteric fractures in the elderly. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(5):569-573.
[30] FISCHER K, TROMBIK M, FREYSTÄTTER G, et al. Timeline of functional recovery after hip fracture in seniors aged 65 and older: a prospective observational analysis. Osteoporos Int. 2019;30(7):1371-1381.
[31] TARRANT SM, ATTIA J, BALOGH ZJ. The influence of weight-bearing status on post-operative mobility and outcomes in geriatric hip fracture. Eur J Trauma Emerg Surg. 2022;48(5):4093-4103.
[32] YANG Y, ZHAO Z, QI X, et al. Computational Modeling of Bone Fracture Healing Under Different Initial Conditions and Mechanical Load. IEEE Trans Biomed Eng. 2024;71(7):2105-2118. |