Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (33): 7173-7180.doi: 10.12307/2025.858
Previous Articles Next Articles
One-stage posterior hemivertebra resection and pedicle screw fixation in treatment of congenital scoliosis: a 2-year follow-up of correction effect
Yang Wanzhong1, 2, Ma Rong1, 2, Guo Wei2, Wang Zhiqiang2, Yang Wei2, Chen Zhen1, Wang Zemin2, Zhang Honglai2, Ge Zhaohui1
- 1First Clinical Medical School of Ningxia Medical University, Yinchuan 750001, Ningxia Hui Autonomous Region, China; 2Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China
-
Received:2024-07-31Accepted:2024-10-23Online:2025-11-28Published:2025-04-12 -
Contact:Ge Zhaohui, Professor, Doctoral supervisor, First Clinical Medical School of Ningxia Medical University, Yinchuan 750001, Ningxia Hui Autonomous Region, China -
About author:Yang Wanzhong, Doctoral candidate, First Clinical Medical School of Ningxia Medical University, Yinchuan 750001, Ningxia Hui Autonomous Region, China; Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China Ma Rong, Doctoral candidate, First Clinical Medical School of Ningxia Medical University, Yinchuan 750001, Ningxia Hui Autonomous Region, China; Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China -
Supported by:2023 Ningxia Key Research & Development Project, No. 2023BEG02017 (to GZH); 2021 Ningxia Key Research & Development Project, No. 2022BEG03087 (to MR); Special Medical Engineering Project of General Hospital of Ningxia Medical University, No. NYZYYG-005 (to GZH)
CLC Number:
Cite this article
Yang Wanzhong, Ma Rong, Guo Wei, Wang Zhiqiang, Yang Wei, Chen Zhen, Wang Zemin, Zhang Honglai, Ge Zhaohui. One-stage posterior hemivertebra resection and pedicle screw fixation in treatment of congenital scoliosis: a 2-year follow-up of correction effect[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7173-7180.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
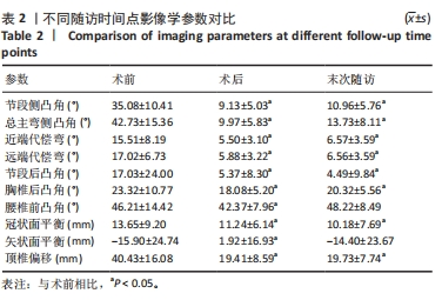
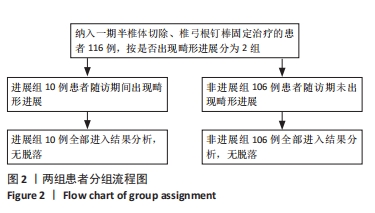
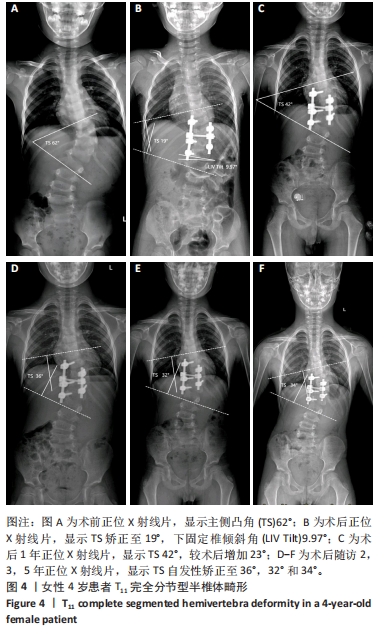
2.3 畸形矫正情况 节段侧凸角由术前(35.08±10.41)°矫正至术后(9.13±5.03)°、末次随访时(10.96±5.76)°,均较术前明显改善(P < 0.05),矫正率分别为67.3%和 64.5%。总主弯侧凸角明显由术前(42.73±15.36)°矫正至术后(9.97±5.83)°、末次随访时(13.73±8.11)°,较术前明显矫正(P < 0.05),矫正率分别为73.2%和 70.2%。 远端代偿弯由术前(17.02±6.73)°矫正至术后(5.88±3.22)°、末次随访时(6.56±3.59)°,畸形明显较术前改善(P < 0.05),最终矫正率为50.5%;近端代偿弯由术前(15.51±8.19)°减少至术后(5.50±3.10)°、末次随访时(6.57±3.59)°(P < 0.05),最终矫正率为55.4%。 节段后凸角由术前(17.03±24.00)°矫正至术后(5.37±8.30)°(P < 0.05),并在末次随访时维持稳定,最终矫正率为71.2%。术后、末次随访时顶椎偏距明显较术前改善(P < 0.05),最终矫正率为68.7%。胸椎后凸角、腰椎前凸角、矢状面平衡及冠状面平衡虽有一定程度矫正,均在正常范围内。见表2。"

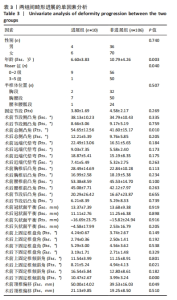
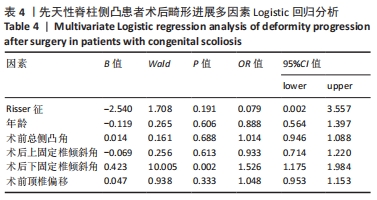
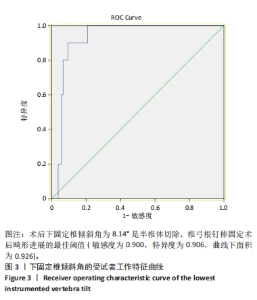
2.4 并发症 随访期间,3例患者出现椎弓根螺钉松动,其中 1例因上固定椎螺钉松动,畸形矫正丢失,行翻修手术;6例患者出现近端交界性后凸畸形,2例行翻修手术;11例出现冠状面失代偿,其中1例为远端附加现象,10例表现为畸形进展,所有失代偿患者均不需要行二次矫形手术,通过延长支具佩戴时间后均明显改善。所有患者在随访期间均未出现迟发性神经损伤,未出现曲轴现象、内植物断裂、假关节形成及椎弓根骨折等并发症。所有患者均未出现内植物不相容情况,包括植入物周围感染、过敏反应及免疫排斥反应。 2.5 畸形进展单因素分析 116例患者中,10例患者在随访期间出现畸形进展,将其与未进展病例进行对比;通过单因素分析发现:年龄(P=0.003)、Risser征(P=0.040)、术前总侧凸角(P=0.010)、术前顶椎偏移(P=0.049)、术后上固定椎倾斜角(P=0.021)及术后下固定椎倾斜角(P=0.000)与畸形进展有关,见表3。"
| [1] MCMASTER MJ, SINGH H. Natural history of congenital kyphosis and kyphoscoliosis. A study of one hundred and twelve patients. J Bone Joint Surg Am. 1999;81(10):1367-1383. [2] MCMASTER MJ, DAVID CV. Hemivertebra as a cause of scoliosis. A study of 104 patients. J Bone Joint Surg Br. 1986;68(4):588-595. [3] KAWAKAMI N, TSUJI T, IMAGAMA S, et al. Classification of congenital scoliosis and kyphosis: a new approach to the three-dimensional classification for progressive vertebral anomalies requiring operative treatment. Spine (Phila Pa 1976). 2009;34(17):1756-1765. [4] NASCA RJ, STILLING FR, STELL HH. Progression of congenital scoliosis due to hemivertebrae and hemivertebrae with bars. J Bone Joint Surg Am. 1975;57(4):456-466. [5] MARKS DS, QAIMKHANI SA. The Natural History of Congenital Scoliosis and Kyphosis. Spine (Phila Pa 1976). 2009;34(17):1751-1755. [6] JOHAL J, LOUKAS M, FISAHN C, et al. Hemivertebrae: a comprehensive review of embryology, imaging, classification, and management. Childs Nerv Syst. 2016;32(11):2105-2109. [7] CHANG D, KIM J, HA K, et al. Posterior Hemivertebra Resection and Short Segment Fusion With Pedicle Screw Fixation for Congenital Scoliosis in Children Younger Than 10 Years : greater than 7-year follow-up. Spine (Phila Pa 1976). 2015;40(8):E484-E491. [8] SHONO Y, ABUMI K, KANEDA K. One-stage posterior hemivertebra resection and correction using segmental posterior instrumentation. Spine (Phila Pa 1976). 2001;26(7):752-757. [9] YANG JH, CHANG DG, SUH SW, et al. Clinical and radiological outcomes of hemivertebra resection for congenital scoliosis in children under age 10 years: More than 5-year follow-up. Medicine (Baltimore). 2020;99(32):e21720. [10] OKSANEN HM, JALANKO T, HELENIUS IJ. Outcomes of early hemivertebrectomy in children with congenital scoliosis: A prospective follow-up study. Scand J Surg. 2021;110(4):542-549. [11] LI H, CHEN Z, GAO B, et al. Surgical outcomes in children under 10 years old in the treatment of congenital scoliosis due to single nonincarcerated thoracolumbar hemivertebra: according to the age at surgery. J Orthop Surg Res. 2021;16(1):721. [12] CROSTELLI M, MAZZA O, MARIANI M, et al. Hemivertebra Resection and Spinal Arthrodesis by Single-Stage Posterior Approach in Congenital Scoliosis and Kyphoscoliosis: Results at 9.6 Years Mean Follow-up. Int J Spine Surg. 2022;16(1):194-201. [13] HUANG Y, FENG G, LIU L, et al. Posterior hemivertebral resection for upper thoracic congenital scoliosis: be aware of high risk of complications. J Pediatr Orthop B. 2019;28(1):1-9. [14] BAO B, SU Q, HAI Y, et al. Posterior thoracolumbar hemivertebra resection and short-segment fusion in congenital scoliosis: surgical outcomes and complications with more than 5-year follow-up. BMC Surg. 2021;21(1):165. [15] PIANTONI L, FRANCHERI WILSON IA, TELLO CA, et al. Hemivertebra Resection With Instrumented Fusion by Posterior Approach in Children. Spine Deform. 2015;3(6):541-548. [16] 涂志明, 王冰, 吕国华, 等. 先天性脊柱侧凸半椎体切除短节段融合术后失代偿的研究进展[J]. 中国脊柱脊髓杂志,2018,28(7): 648-651. [17] YANG X, SONG Y, LIU L, et al. Emerging S-shaped curves in congenital scoliosis after hemivertebra resection and short segmental fusion. Spine J. 2016;16(10):1214-1220. [18] LI S, CHEN Z, QIU Y, et al. Coronal Decompensation After Posterior-only Thoracolumbar Hemivertebra Resection and Short Fusion in Young Children With Congenital Scoliosis. Spine (Phila Pa 1976). 2018;43(9):654-660. [19] BAO B, YAN H, TANG J. A review of the hemivertebrae and hemivertebra resection. Br J Neurosurg. 2022;36(5):546-554. [20] KAROL LA. The Natural History of Early-onset Scoliosis. J Pediatr Orthop. 2019;39((Issue 6, Supplement 1 Suppl 1):S38-S43. [21] MACKEL CE, JADA A, SAMDANI AF, et al. A comprehensive review of the diagnosis and management of congenital scoliosis. Childs Nerv Syst. 2018;34(11):2155-2171. [22] GAO R, ZHANG X, GUO D, et al. Medium-term and Long-term Follow-up Surgical Outcomes of the 1-stage Posterior-only Lumbosacral Hemivertebra Resection With Short-segment Fusion in Children. J Pediatr Orthop. 2023;43(2):e120-e126. [23] XUE X, ZHAO S. Posterior hemivertebra resection with unilateral instrumented fusion in children less than 10 years old: preliminary results at minimum 5-year follow-up. J Orthop Surg Res. 2018; 13(1):240. [24] BARIK S, MISHRA D, GUPTA T, et al. Surgical outcomes following hemivertebrectomy in congenital scoliosis: a systematic review and observational meta-analysis. Eur Spine J. 2021;30(7):1835-1847. [25] WANG Y, LIU Z, DU C, et al. The radiological outcomes of one-stage posterior-only hemivertebra resection and short segmental fusion for lumbosacral hemivertebra: a minimum of 5 years of follow-up. J Orthop Surg Res. 2019;14(1):426. [26] 张福勇,王晓东,甄允方,等.后路半椎体切除短节段固定儿童先天性脊柱畸形[J].中国矫形外科杂志,2024,32(7):650-653. [27] GUO J, ZHANG J, WANG S, et al. Surgical outcomes and complications of posterior hemivertebra resection in children younger than 5 years old. J Orthop Surg Res. 2016;11(1):48. [28] SÁNCHEZ-MÁRQUEZ JM, PIZONES J, MARTÍN-BUITRAGO MP, et al. Midterm Results of Hemivertebrae Resection and Transpedicular Short Fusion in Patients Younger Than 5 Years: How Do Thoracolumbar and Lumbosacral Curves Compare? Spine Deform. 2019;7(2):267-274. [29] WANG S, ZHANG J, QIU G, et al. Posterior-only Hemivertebra Resection With Anterior Structural Reconstruction With Titanium Mesh Cage and Short Segmental Fusion for the Treatment of Congenital Scoliokyphosis. Spine (Phila Pa 1976). 2017;42(22):1687-1692. [30] ZHUANG Q, ZHANG J, LI S, et al. One-stage posterior-only lumbosacral hemivertebra resection with short segmental fusion: a more than 2-year follow-up. Eur Spine J. 2016;25(5):1567-1574. [31] 王升儒, 林莞锋, 杨阳, 等. 后路一期半椎体切除治疗先天性脊柱侧凸的疗效及并发症研究[J]. 中华骨与关节外科杂志,2020, 13(12):976-981. [32] SHI BL, LI Y, ZHU ZZ, et al. Failed Primary Surgery in Congenital Scoliosis Caused by a Single Hemivertebra: Reasons and Revision Strategies. Orthop Surg. 2022;14(2):349-355. [33] XU Y, LI J, LI D, et al. Presence of compensatory curve predicts postoperative curve progression in congenital scoliosis after thoracolumbar hemivertebra resection and short fusion. Eur Spine J. 2024. doi: 10.1007/s00586-024-08398-0. [34] 杨曦, 宋跃明, 刘立岷, 等. 先天性半椎体切除术后新发侧凸畸形的临床分析[J]. 中国脊柱脊髓杂志,2018,28(7):586-592. [35] 蒋彬, 王冰, 吕国华, 等. 上胸段半椎体切除术后远端冠状面S畸形进展的危险因素[J]. 中国脊柱脊髓杂志,2021,31(5):394-401. [36] WANG Y, SHI B, LIU Z, et al. The Upper Instrumented Vertebra Horizontalization: An Essential Factor Predicting the Spontaneous Correction of Compensatory Curve After Lumbosacral Hemivertebra Resection and Short Fusion. Spine (Phila Pa 1976). 2020;45(19): E1272-E1278. [37] 曹隽,张学军,白云松,等.后路半椎体切除短节段融合固定术治疗儿童腰骶段半椎体畸形及近端代偿侧凸自发矫正的影响因素[J].中国脊柱脊髓杂志,2021,31(5):408-415. [38] CHANG D, YANG J, LEE J, et al. Congenital scoliosis treated with posterior vertebral column resection in patients younger than 18 years: longer than 10-year follow-up. J Neurosurg Spine. 2016; 25(2):225-233. [39] 邹传奇,初同伟,周跃.一期经后路半椎体切除矫治先天性脊柱半椎体侧后凸畸形研究进展[J].中国修复重建外科杂志,2014, 28(7):909-912. [40] 刘威,陈文昊.先天性脊柱侧弯半椎体切除的研究进展[J].中国矫形外科杂志,2024,32(19):1776-1779+1785. |
| [1] | Zhang Hao, Wang Qing, Zhang Jian, Li Guangzhou, Wang Gaoju. Comparison of posterior C2-3 fixation combined with bucking bar technique and posterior C2-3 fixation alone in treatment of unstable Hangman fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1848-1854. |
| [2] | Su Lintao, Jiang Jianfeng, Ma Jun, Huang Liangliang, Lei Changyu, Han Yaozheng, Kang Hui. Precise application of O-arm navigation system in thoracolumbar fractures with developmental pedicle stenosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1855-1862. |
| [3] | Gao Zhenyang, Zeng Xiuan, Yang Qibing, Kou Xianshuai, Wang Kejing, Li Meng. Computer-simulated repositioning combined with pelvic reduction frame for treatment of anteroposterior compression-III pelvic fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1870-1875. |
| [4] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [5] | Huang Haobo, Liang Xinyuan, Ye Guozhong, Xie Qingxiang, Su Boyuan. Suture tape and headless compression screws in treatment of Lisfranc injury with comminuted fractures of the first and second proximal metatarsal bones [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1803-1809. |
| [6] | Yu Ming, Wang Wen. Posterior cruciate ligament tibial attachment point avulsion fracture: materials, implants, and internal fixation techniques in arthroscopic treatment [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 872-880. |
| [7] | Sheng Wenbo, Liu Bingli, Li Sibo, Ao Rongguang, Yu Baoqing. Cement-augmented short-segment percutaneous pedicle screw fixation for the stage II Kümmell’s disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7286-7292. |
| [8] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| [9] | Xu Xin, Wurikaixi·Aiyiti, Lyu Gang, Maimaiaili·Yushan, Ma Zhiqiang, Ma Chao. Finite element analysis of four different internal fixation methods for complex acetabular double-column fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7063-7071. |
| [10] | Hu Chaoran, Cen Chaode, Yang Yang, Zhou Cheng, Huang Huaxian, Yuan Honghao, Luo Qin, Cao Yongfei. 3D printing assisted minimal invasive plate osteosynthesis versus intramedullary nail for treatment of AO12-C middle-proximal humeral fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7116-7122. |
| [11] | Yan Jinlian, Xu Zhengquan, Wei Renjie, Wang Yehua. Hip joint function recovery and prediction model construction after proximal femoral nail antirotation for intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7189-7195. |
| [12] | Cao Yong, Li Xin, Chen Zhigang, Gu Honglin, Lyu Shujun. Compensatory alignment changes of cervical and thoracic spine after correction of lumbar degenerative scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7196-7202. |
| [13] | Hu Liuchao, Luo Yiwen, Wu Zhifang. Fracture line map characteristics of distal radius fractures involving dorsal articular surface: effective fixation with screws for postoperative displacement [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 524-530. |
| [14] | Liu Xiaoyin, Zhang Jianqun, Chen Zhen, Liang Simin, Wang Zhiqiang, Ma Zongjun, Ma Rong, Ge Zhaohui. Short-term efficacy of oblique lateral interbody fusion combined with lateral plate fixation in treatment of single-level lumbar degenerative disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 531-537. |
| [15] | Li Zhenggang, Shang Xuehong, Wu Zhang, Li Hong, Sun Chaojun, Chen Huadong, Sun Zhe, Yang Yi. Finite element analysis of three internal fixation modalities for treatment of Pauwels type III femoral neck fractures under different loading conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 455-463. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||