Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (33): 7158-7164.doi: 10.12307/2025.808
Previous Articles Next Articles
Optimal rotational alignment of the tibial component during Oxford unicompartmental knee arthroplasty
Liu Ning, Sun Yingjin, Huang Long, Feng Shuo, Chen Xiangyang
- Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
-
Received:2024-04-22Accepted:2024-07-05Online:2025-11-28Published:2025-04-12 -
Contact:Chen Xiangyang, MD, Chief physician, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
About author:Liu Ning, Master candidate, Physician, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
Supported by:New Medical Technology Project of Affiliated Hospital of Xuzhou Medical University, No. 2023301010 (to CXY)
CLC Number:
Cite this article
Liu Ning, Sun Yingjin, Huang Long, Feng Shuo, Chen Xiangyang. Optimal rotational alignment of the tibial component during Oxford unicompartmental knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7158-7164.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
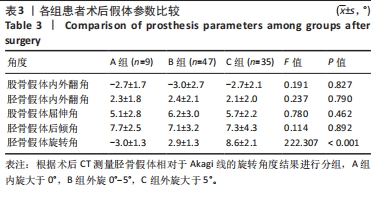
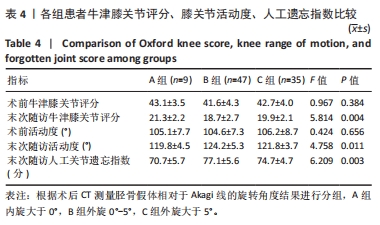
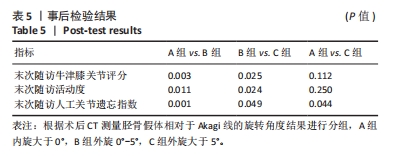
| [1] REN Y, HU J, TAN J, et al. Incidence and risk factors of symptomatic knee osteoarthritis among the Chinese population: analysis from a nationwide longitudinal study. BMC Public Health. 2020; 20(1):1491. [2] ROSSI SMP, SANGALETTI R, NESTA F, et al. A well performing medial fixed bearing UKA with promising survivorship at 15 years. Arch Orthop Trauma Surg. 2023;143(5):2693-2699. [3] PONGCHAROEN B, LIENGWATTANAKOL P, BOONTANAPIBUL K, et al. Comparison of functional recovery between unicompartmental and total knee arthroplasty: A randomized controlled trial. J Bone Joint Surg Am. 2023;105(3):191-201. [4] BANDI M, BENAZZO F, BATAILLER C, et al. A morphometric fixed-bearing unicompartmental knee arthroplasty can reproduce normal knee kinematics. Arthroplasty Today. 2022;16:151-157. [5] GHOMRAWI HM, EGGMAN AA, PEARLE AD, et al. Effect of age on cost-effectiveness of unicompartmental knee arthroplasty compared with total knee arthroplasty in the U.S. J Bone Joint Surg Am. 2015; 97(5):396-402. [6] CASPER DS, FLEISCHMAN AN, PAPAS PV, et al. Unicompartmental knee arthroplasty provides significantly greater improvement in function than total knee arthroplasty despite equivalent satisfaction for isolated medial compartment osteoarthritis. J Arthroplasty. 2019;34(8):1611-1616. [7] GUERREIRO JPF, SANTOS VKJD, MATZ LB, et al. Does partial medial knee arthroplaties have better results than total ones? Acta Ortop Bras. 2023;31(spe2):e262186. [8] KERENS B, LEENDERS AM, SCHOTANUS MGM, et al. Patient-specific instrumentation in Oxford unicompartmental knee arthroplasty is reliable and accurate except for the tibial rotation. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1823-1830. [9] ALETO TJ, BEREND ME, RITTER MA, et al. Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty. 2008;23(2):159-163. [10] KOH YG, PARK KM, KANG K, et al. Finite element analysis of the influence of the posterior tibial slope on mobile-bearing unicompartmental knee arthroplasty. Knee. 2021;29:116-125. [11] ALRUWAILI SH, PARK KK, YANG IH, et al. Difference between medial and lateral tibia plateau in the coronal plane: importance of preoperative evaluation for medial unicompartmental knee arthroplasty. BMC Musculoskeletal Disorder. 2022;23(1):342. [12] MARULLO M, RUSSO A, SPREAFICO A, et al. Mild valgus alignment after lateral unicompartmental knee arthroplasty led to lower functional results and survivorship at mean 8-year follow-up. J Arthroplasty. 2023;38(1):37-42. [13] DOUIRI A, BOUGUENNEC N, BISET A, et al. Functional scores and prosthetic implant placement are different for navigated medial UKA left in varus alignment. Knee Surg Sports Traumatol Arthrosc. 2023;31(9):3919-3926. [14] FAROOQ H, DECKARD ER, CARLSON J, et al. Coronal and sagittal component position in contemporary total knee arthroplasty: Targeting native alignment optimizes clinical outcomes. J Arthroplasty. 2023;38:S245-S251. [15] MALYAVKO A, COHEN JS, FULLER SI, et al. Reduced early revision surgery and medical complications in computer-assisted knee arthroplasty compared with non-computer-assisted arthroplasty. J Am Acad Orthop Surg. 2023; 31(2): 87-96. [16] ZHANG J, NDOU WS, NG N, et al. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(8):2677-2695. [17] ZHOU X, SUN C, XU R, et al. The effect of tibial component rotational alignment on clinical outcomes of mobile-bearing unicompartmental knee arthroplasty. J Orthop Surg Res. 2023; 18(1):217. [18] LIOW MHL, TSAI TY, DIMITRIOU D, et al. Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty. 2016; 31(10):2167-2172. [19] JANG KM, LIM HC, HAN SB, et al. Does new instrumentation improve radiologic alignment of the Oxford® medial unicompartmental knee arthroplasty? Knee. 2017;24(3):641-650. [20] HERNIGOU P, DESCHAMPS G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004;86(3):506-511. [21] 田文明,王光达. CT在膝关节Oxford单髁置换术后假体位置评价中的应用[J]. 世界最新医学信息文摘(连续型电子期刊),2018, 18(A2):31-33. [22] 李相伟,丁晶. Oxford单髁置换术的术后影像学评价及分析[J]. 中华关节外科杂志(电子版),2013,7(1):48-51. [23] CASPER DS, FLEISCHMAN AN, PAPAS PV, et al. Unicompartmental Knee Arthroplasty Provides Significantly Greater Improvement in Function than Total Knee Arthroplasty Despite Equivalent Satisfaction for Isolated Medial Compartment Osteoarthritis. J Arthroplasty.2019; 34(8):1611-1616. [24] 张江涛,尚延春,李启义,等.全膝关节置换术与单髁置换术治疗内侧间室膝骨关节炎疗效对比的meta分析[J].中华骨与关节外科杂志,2020,13(10):830-835+858 [25] LEE SY, CHAY S, LIM HC, et al. Tibial component rotation during the unicompartmental knee arthroplasty: is the anterior superior iliac spine an appropriate landmark? Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3723-3732 [26] TSAI TY, DIMITRIOU D, HOSSEINI A, et al. Assessment of accuracy and precision of 3D reconstruction of unicompartmental knee arthroplasty in upright position using biplanar radiography. Med Eng Phys. 2016; 38(7): 633-638. [27] SERVIEN E, FARY C, LUSTIG S, et al. Tibial component rotation assessment using CT scan in medial and lateral unicompartmental knee arthroplasty. Orthop Traumatol Surg Res. 2011;97(3):272-275. [28] IRIBERRI I, ARAGÓN JF. Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT scan: does it influence the outcome? Knee. 2014;21(6):1269-1274. [29] NG JP, FAN JCH, CHAU WW, et al. Does component axial rotational alignment affect clinical outcomes in Oxford unicompartmental knee arthroplasty? Knee. 2020;27(6):1953-1962. [30] IWAKI H, PINSKEROVA V, FREEMAN MA, et al. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82(8):1189-1195. [31] HERNÁNDEZ-HERMOSO JA, NESCOLARDE L, YAÑEZ-SILLER F, et al. Combined femoral and tibial component total knee arthroplasty device rotation measurement is reliable and predicts clinical outcome. J Orthop Traumatol. 2023;24(1):40. [32] RAJGOPAL A, SUDARSHANP, KUMAR S, et al. Failure modes in malrotated total knee replacement. Arch Orthop Trauma Surg. 2023; 143(5):2713-2720. [33] NICOLL D, ROWLEY DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br. 2010; 92(9):1238-1244. [34] BÉDARD M, VINCE KG, REDFERN J, et al. Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res. 2011;469(8):2346-2355. [35] KAMENAGA T, HIRANAKA T, TAKAYAMA K, et al. Adequate positioning of the tibial component is key to avoiding bearing impingement in oxford unicompartmental knee arthroplasty. J Arthroplasty. 2019;34(11): 2606-2613. [36] ESCUDIER IC, JACQUET C, FLECHER X, et al. Better Implant Positioning and Clinical Outcomes With a Morphometric Unicompartmental Knee Arthroplasty. Results of a Retrospective,Matched-Controlled Study. J Arthroplasty. 2019;34(12):2903-2908 [37] KAMENAGA T, HIRANAKA T, HIDA Y, et al. Rotational position of the tibial component can decrease bony coverage of the tibial component in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee. 2019;26(2):459-465. [38] CHAU R, GULATI A, PANDIT H, et al. Tibial component overhang following unicompartmental knee replacement--does it matter? Knee. 2009;16(5): 310-313. [39] GUDENA R, PILAMBARAEI MA, WERLE J, et al. A safe overhang limit for unicompartmental knee arthroplasties based on medial collateral ligament strains: an in vitro study. J Arthroplasty. 2013; 28(2):227-233. [40] XU K, CHEN Q, YAN Q, et al. Comparison of computer-assisted navigated technology and conventional technology in unicompartmental knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2022;17(1):123. [41] AHMED AG, TIAN Y, HASAN M, et al. Revisiting short-term outcomes of conventional and computer-assisted total knee arthroplasty: A population-based study. J Am Acad Orthop Surg Glob Res Rev. 2022; 6(6):e22 68000. [42] MALHOTRA R, GUPTA S, GUPTA V, et al. Navigated unicompartmental knee arthroplasty: A different perspective.Clin Orthop Surg. 2021;13(4):491-498 |
| [1] | Ma Chi, Wang Ning, Chen Yong, Wei Zhihan, Liu Fengji, Piao Chengzhe. Application of 3D-printing patient-specific instruments combined with customized locking plate in opening wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1863-1869. |
| [2] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [3] | Wang Peiguang, Zhang Xiaowen, Mai Meisi, Li Luqian, Huang Hao. Generalized equation estimation of the therapeutic effect of floating needle therapy combined with acupoint embedding on different stages of human knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1565-1571. |
| [4] | He Guanghui, Yuan Jie, Ke Yanqin, Qiu Xiaoting, Zhang Xiaoling. Hemin regulates mitochondrial pathway of oxidative stress in mouse chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1183-1191. |
| [5] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [6] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| [7] | Jiang Tao, Zhang Chuankai, Hao Liang, Liu Yong. MAKO robot- and navigation-assisted knee replacement: comparison of lower limb force alignment and prosthesis position accuracy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7150-7157. |
| [8] | Jiang Zehua, Du Wenjun, Ren Zhishuai, Cui Haojun, Zhu Rusen. Percutaneous vertebroplasty via Kambin's triangle for treatment of osteoporotic compression fractures: evaluation of safety and effectiveness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7181-7188. |
| [9] | Liu Mengfei, Chen Gang, Shi Yihan, Zeng Lin, Jiang Kan, Yilihamujiang•Wusiman. Finite element analysis of optimization of femoral prosthesis implantation position in unicompartmental knee arthroplasty in osteoporotic patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 464-470. |
| [10] | Shi Lei, Shi Song, Lu Yue, Tao Ran, Ma Hongdong. Comparison of unicondylar knee arthroplasty and high tibial osteotomy in treatment of medial knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 503-509. |
| [11] | Li Jia, Liu Qianru, Xing Mengnan, Chen Bo, Jiao Wei, Meng Zhaoxiang. A network meta-analysis on therapeutic effect of different types of exercise on knee osteoarthritis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 609-616. |
| [12] | Zhang Yunyi, Liu Songtao, Xie Shaodong, Zhu Haifeng, Qian Guifeng, Huo Ming, Zhou Jie, Deng Zixuan. Platelet rich plasma versus hyaluronic acid in treatment of knee osteoarthritis: an overview of systematic reviews [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 6138-6145. |
| [13] | Sun Yingjin, Liu Ning, Huang Long, Feng Shuo, Chen Xiangyang. Effect of patellar morphology on functional recovery and patellofemoral joint alignment after unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5826-5832. |
| [14] | Ding Yuan, Gong Jianbao, Zhang Jie, Qiao Yuan, Xu Wenlong. Characteristic analysis of isometric muscle strength of knee joint in patients after unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5833-5838. |
| [15] | Shaban Amiri Nzelekela, Yang Lianbo, Li Peng. Objective accuracy of six degree of freedom gait analysis system in evaluating the severity of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5890-5896. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||