Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (21): 4612-4620.doi: 10.12307/2025.828
Research and development trends and hot spots of spinal surgical robots for treatment of spinal diseases
Niu Yanyan1, Zhang Qi2, Fan Mingxing2
- 1Medical Journal Center, 2Department of Spine Surgery, Beijing Jishuitan Hospital Affiliated to Capital Medical University, Beijing 100035, China
-
Received:2024-08-21Accepted:2024-08-31Online:2025-07-28Published:2024-12-07 -
Contact:Fan Mingxing, MD, Associate chief physician, Department of Spine Surgery, Beijing Jishuitan Hospital Affiliated to Capital Medical University, Beijing 100035, China -
About author:Niu Yanyan, Assistant researcher, Medical Journal Center, Beijing Jishuitan Hospital Affiliated to Capital Medical University, Beijing 100035, China -
Supported by:National Natural Science Foundation of China, No. 82302353 (to FMX)
CLC Number:
Cite this article
Niu Yanyan, Zhang Qi, Fan Mingxing. Research and development trends and hot spots of spinal surgical robots for treatment of spinal diseases[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4612-4620.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
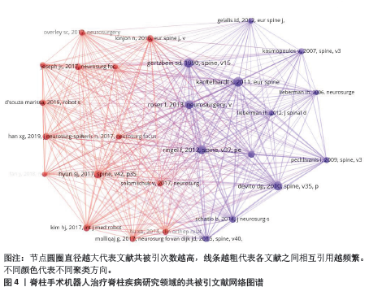
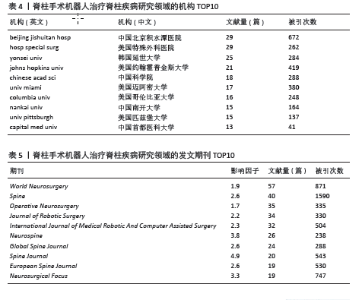
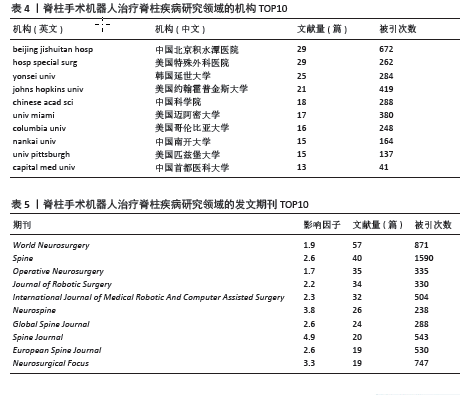
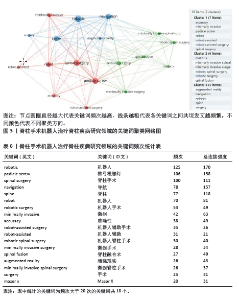
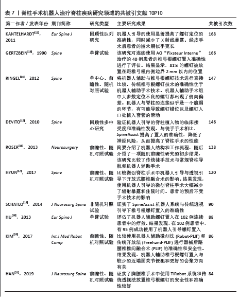
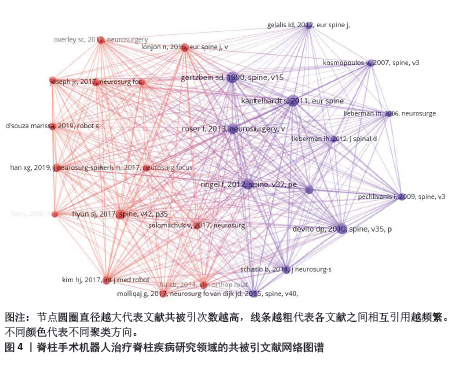
2.7 文献共被引分析 2.7.1 共被引文献热点分析 在该领域的共被引文献的网络图谱见图4。文章总结了发文量排名前10位的经典共被引文献[12-21],见表7。 KANTELHARDT等[12] (2011)开展了一项回顾性队列研究(被引168次),观察了机器人引导在提高螺钉定位准确性和减少X射线暴露方面的作用。尽管机器人辅助提高了操作精确度,但患者的围术期似乎更长,这可能对临床应用提出了额外考虑。这项研究是最高被引的文献,显示了其在专业领域的广泛影响力。 GERTZBEIN等[13] (1990)在一项单臂试验(被引166次)中,评估了AO “Fixateur Interne”治疗椎弓根螺钉置入的准确性。该研究显示了较高的置钉准确率,这是早期机器人辅助脊柱手术技术的研究之一。 RINGEL等[14] (2012)在一项单中心、前瞻性、随机对照试验(被引147次)中,将机器人辅助技术与传统椎弓根螺钉技术进行了直接比较发现,传统技术在准确性上优于机器人辅助技术,尤其是在螺钉定位的侧向偏差方面,这提示在某些情况下,传统技术可能仍然更具优势。 DEVITO等[15] (2010)在一项回顾性多中心研究(被引146次)中,验证了机器人引导的脊柱植入物的临床接受度和准确性。研究发现在准确性以及降低神经风险方面,机器人引导的SpineAssist优于徒手操作,凸显了其对临床实践的重要意义。 ROSER等[16] (2013)在一项前瞻性、随机对照试验(被引138次)中,比较了传统徒手技术与常规脊柱导航和机器人辅助手术,提供了机器人结构和工作流程的初步结果,反映了其对脊柱手术技术发展的贡献。 HYUN等[17] (2017) 在一项前瞻性、随机对照试验(被引120次)中,比较了微创脊柱手术中机器人引导与透视引导下开放式腰椎融合术的影响发现,机器人引导的MIS可以大幅减少辐射暴露和住院时间,而不影响患者的预后。 SCHATLO等[18] (2014)在一项非随机对照试验(被引90次)中,证实了SpineAssist机器人系统在椎弓根螺钉置入过程中的准确性,与传统透视引导技术相当。 HU等[19] (2013) 在一项单臂试验(被引88次)中,评估了102例患者中连续使用机器人引导螺钉置入的疗效发现,在大多数患者中,机器人引导技术得以成功应用。 KIM等[20] (2017)在一项前瞻性、随机对照试验(被引86次)中,比较了机器人辅助微创法(Robot-PLIF)和传统开放法(Freehand-PLIF)进行器械后路腰椎椎间融合术的准确性和安全性,发现机器人辅助技术与较少的近端关节面侵犯和更好的聚焦方向有关。 HAN等[21] (2019) 在一项前瞻性、随机对照试验(被引84次)中,对胸腰椎手术中使用TiRobot系统和传统透视法放置椎弓根螺钉的安全性和准确性进行了比较发现,两种方法在安全性和准确性上都表现良好。 2.7.2 脊柱手术机器人领域的高被引的里程碑研究分析 文章进一步分析共被引文献的研究历程发现,从2012-2020年期间,在脊柱手术机器人领域中,多项里程碑研究得以开展并取得了显著成果,这些研究涵盖了手术机器人的应用、准确性评估、优势以及潜在的挑战等方面。文章整理了高被引研究中的具体有代表性的里程碑研究。 (1) 在2012年,脊柱手术机器人应用于临床取得了一定成果,诞生了3项在脊柱手术机器人领域的里程碑研究。SCHIZAS等[22]推出了用于椎弓根螺钉置入的骨安装机器人引导技术,旨在提高精确度,这项前瞻性研究的目的是将这种新方法与传统的透视辅助徒手技术(非二维或三维透视导航)进行比较。目前的研究并不能说明机器人辅助螺钉置入取代了传统的透视辅助技术,尽管文献对前者更为乐观(共被引47次)。RINGEL等[14]进行了一项单中心前瞻性随机对照研究(共被引53次),评估了机器人辅助(RO)植入腰椎/骶椎椎弓根螺钉与徒手置钉传统技术相比的准确性。在这项研究中,传统徒手置钉技术的准确性优于 RO 技术,RO组中大多数定位不良的螺钉都出现了侧向偏差。机器人与脊柱的连接似乎是一个脆弱的环节,有可能导致螺钉错位以及螺钉入口处植入套管的滑动。一项对照尸体植入试验(共被引147次)显示,机器人引导系统的相关优势可能会让外科医生更放心地为患者提供微创或经皮手术选择[23],并让他们在实施基于椎弓根的固定时更加得心应手。这种先进的技术还可以将具有复杂解剖畸形的患者纳入手术范围,而这些患者常被排除在椎弓根螺钉手术方案之外。 (2)在2013年,诞生了2项里程碑研究,出现了脊柱手术机器人的结构和工作流程,并报道了机器人辅助螺钉置入失败的诱因。ROSER等[16]简要介绍了脊柱手术机器人的结构和工作流程(共被引138次),并介绍了一项随机前瞻性研究的初步结果,该研究比较了传统徒手技术与常规脊柱导航和机器人辅助手术,发现与标准手术相比,机器人辅助手术提高了准确性,减少了患者和外科医生的辐射暴露。现有设备的第二代硬件和软件升级将改进工作流程和术中设置。随着该领域更多研究的发表,机器人辅助疗法将在不久的将来获得更广泛的认可。HU等[19]评估了机器人辅助螺钉置入在102例连续患者中的疗效(共被引88次)。在使用机器人植入的960枚螺钉中,有949枚(98.9%)成功准确地植入,11枚(1.1%)定位不当,尽管大多数患者都有严重的脊柱畸形和/或曾接受过脊柱手术。工具滑脱被认为是螺钉错位的诱因。 (3) 在2014年,HU等[24]进一步研究(共被引70次)发现,成功放置椎弓根螺钉的比例随着经验的增加而提高,随着经验的增加,转为手动置入的螺钉率有所下降,在学习曲线中,螺钉错位的频率相似,从0%-1.4%。SCHATLO等[18]研究(共被引90次)认为,机器人引导下的椎弓根螺钉置入是协助脊柱外科医生处理退行性脊柱病例的一种安全、有用的工具。尽管如此,技术上的困难依然存在,建议使用透视后备技术。 (4) 在2015年,KIM等[25]进行了一项前瞻性随机对照试验(共被引48次),目的是在机器人辅助椎弓根螺钉固定应用的初始阶段,通过累积总和(CUSUM)测试来监控机器人辅助椎弓根螺钉固定准确性的质量控制。文章根据CUSUM分析证明,即使在应用初期,机器人辅助椎弓根螺钉固定术的质量控制也是充分的。其次,CUSUM 检验是监控脊柱手术相关程序质量的有效工具。SCHATLO等[26]回顾性研究(共被引46次)旨在评估经验和时间是否会影响借助 SpineAssist?机器人系统放置螺钉的准确性。结果发现,螺钉错置率的一个主要高峰出现在10-20 例手术,第二个较小的高峰出现在40例手术左右。一种可能的解释是,外科医生在掌握新技术(熟练掌握)之前,从监管减少(不熟练但了解)到信心增强(不熟练但不了解)的过渡。因此,该研究主张至少在机器人脊柱手术的前25例手术中确保对新外科医生进行合格的指导,以优化机器人辅助椎弓根螺钉的精确度。 (5) 在2016年,LONJON等[27]研究(共被引84次)发现,与传统技术相比,机器人技术的精确率更高。采用图像引导工具通过长期监控患者的运动来提供辅助,有助于更准确地定位椎弓根进入点并控制轨迹。LEFRANC等[28]报道了一种新型ROSA? 机器人(法国蒙彼利埃 Medtech 公司)(共被引38次),是一种新型医疗设备,旨在协助外科医生进行微创脊柱手术。ROSA? Spine 机器人可实现精确的椎弓根螺钉置放。凭借其机械臂和导航能力,该机器人可在整个手术过程中监控脊柱的运动,从而完全按照外科医生的计划,准确、安全地进行关节置换术,治疗腰椎间盘退行性疾病。 (6) 在2017年,OVERLEY等[29]的一篇综述(共被引72次)证实,脊柱手术可能是整合导航和机器人辅助手术的理想选择,文章还探讨了术中导航和机器人辅助脊柱手术的可选方案。HYUN等[17]进行了一项前瞻性随机临床试验(共被引120次),比较机器人引导的微创脊柱手术与透视引导的开放式腰椎融合术的影响发现,使用机器人引导的微创脊柱手术 大幅减少了辐射暴露和住院时间。患者的预后不受手术技术的影响。 (7) 在2018年,GAO等[30]的一项基于随机对照试验的荟萃分析表明(共被引48次),与徒手技术相比,机器人辅助技术具有相同的椎弓根螺钉植入准确率、更少的近端面关节侵犯、更少的术中辐射暴露,但手术时间更长。LAUDATO等[31]的一项回顾性放射学研究(共被引39次)评估使用 O-Arm 导航、机器人辅助或徒手透视技术插入椎弓根螺钉的准确性,结果发现新技术的出现似乎并未改变螺钉置入的准确性。在指导下,脊柱外科医生在使用新工具时可能与经验丰富的外科医生表现相当。准确性上的差异并不意味着上述技术没有额外的优势。MENGER等[32]调查了在活跃的神经外科实践中增加脊柱手术机器人技术的成本效益(共被引44次),结果发现,应用机器人脊柱手术具有成本效益,可减少翻修手术、降低感染率、缩短住院时间和手术时间。有必要开展进一步研究,评估机器人脊柱手术的经济效益。GHASEM等[33]的一项系统综述(共被引61次)表明,采用机器人技术进行椎弓根螺钉置入可在高度一致的基础上获得可接受的精确度。外科医生应该对机器人辅助螺钉轨迹的确认保持警惕,因为钻孔路径已被证明会因软组织压力、强力手术应用和骨表面滑动而改变。然而,机器人辅助对辐射暴露、住院时间和手术时间的有效影响仍不清楚,需要在未来的研究中不断完善。 (8) 在2019年,KHAN等[34]进行了一项回顾性病历审查(共被引58次),获取了20例患者的数据,这些患者因伴有或不伴有脊柱滑脱的退行性椎间盘疾病接受椎间融合术以稳定腰椎后,在机器人引导下接受了腰椎椎弓根螺钉置入。手术使用了最新一代的 Mazor X(Mazor Robotics Ltd,以色列凯撒利亚),结果显示Mazor X机器人脊柱手术安全可行,精确可靠,学习曲线最小。KOCHANSKI等[35]的综述(共被引42次)认为,图像引导(IG)和机器人系统的应用越来越广泛,是脊柱手术中不可多得的术中辅助工具,两者都高度依赖于立体定向和术前或术中放射成像,这两种技术还能为手术室工作人员、外科医生和患者带来减少电离辐射职业暴露的潜在好处。 (9) 在2020年,LI等[36]的一项荟萃分析(共被引46次)显示,机器人辅助技术在椎弓根螺钉置入方面比徒手技术更精确。TINAVI机器人辅助椎弓根螺钉置入比传统技术和复兴时期的机器人辅助手术更加精确。"
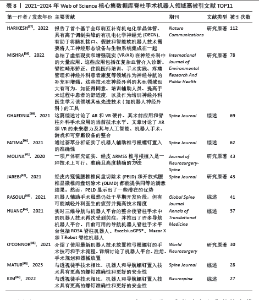
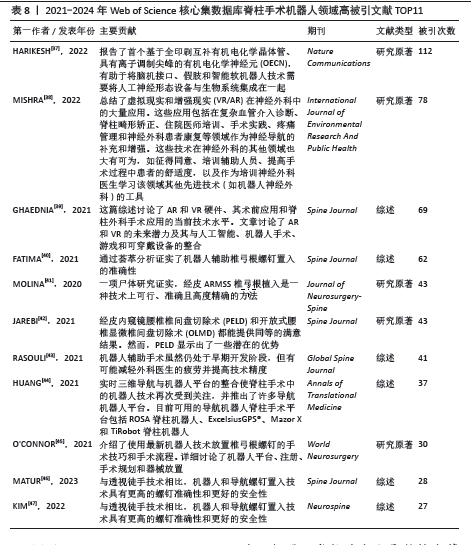
2.8 最新发表的高被引文献热点汇总 文章进一步检索了2021-2024年Web of Science核心集数据库发表的该领域最新高被引文献11篇[37-47],见表8,剖析近年来的研究热点发现,脊柱手术机器人领域的研究热点主要集中在以下几个方面:①技术进步与创新:研究人员报告了基于全印刷互补有机电化学晶体管的有机电化学神经元(OECN),为脑机接口、假肢和智能软机器人技术提供了新的集成方案。②虚拟现实(VR)和增强现实(AR)技术在神经外科中的应用:文献中总结了VR/AR技术在复杂血管介入诊断、脊柱畸形矫正、住院医师培训、手术实践、疼痛管理和神经外科患者康复等领域的广泛应用。③机器人辅助椎弓根螺钉置入的准确性:通过荟萃分析和尸体研究,证实了机器人辅助椎弓根螺钉置入的准确性,并与透视徒手技术进行了比较,结果显示机器人辅助技术具有更高的螺钉准确性和更好的安全性。④导航机器人脊柱手术平台的进展:介绍了实时三维导航与机器人平台的整合,以及当前可用的导航机器人脊柱手术平台,包括ROSA脊柱机器人、ExcelsiusGPS、Mazor X脊柱机器人和TiRobot。⑤手术技巧和流程:文献中详细介绍了使用最新机器人技术放置椎弓根螺钉的手术技巧和流程,包括机器人平台的注册、手术规划和器械放置。⑥机器人辅助手术的潜力:尽管机器人辅助手术仍处于早期开发阶段,但它有可能减轻外科医生的疲劳并提高技术精度。 因此,脊柱手术机器人领域的研究热点集中在技术进步、精确度和安全性、手术技巧和流程、以及未来潜力的探索上。随着技术的不断进步和临床应用的扩展,机器人辅助脊柱手术有望成为未来脊柱外科手术的主流技术。"
| [1] YUH WT, KIM JH, HAN J, et al. The iterative implementation of a comprehensive enhanced recovery after surgery protocol in all spinal surgery in Korea: a comparative analysis of clinical outcomes and medical costs between primary spinal tumors and degenerative spinal diseases. J Neurosurg Spine. 2023;40(3):301-311. [2] HAIM O, AGUR A, GABAY S, et al. Differentiating spinal pathologies by deep learning approach. Spine J. 2024;24(2):297-303. [3] LENGA P, TRONG PD, PAPAKONSTANTINOU V, et al. Adverse events in spine surgery: a prospective analysis at a large tertiary center in Germany. Acta Neurochir (Wien). 2023;165(9):2689-2697. [4] 张世民.稳妥开展腰椎微创融合技术以减少手术并发症[J].中国骨伤,2023,36(5):399-402. [5] GIORGI PD, LEGRENZI S, SACCHI L, et al. Implementation of robotic exoscope in minimally invasive corpectomy at thoracolumbar junction for the treatment of traumatic spinal cord compression. World Neurosurg. 2024;184:23-28. [6] KOVACIC J, CANAGASINGHAM A, GOOLAM A, et al. A robot-assisted laparoscopic revision of an artificial urinary sphincter in a patient with spinal cord injury. BJU Int. 2024;133 Suppl 3:68-71. [7] SPETZGER U, VON SCHILLING A, WINKLER G, et al. The past, present and future of minimally invasive spine surgery: a review and speculative outlook. Minim Invasive Ther Allied Technol. 2013;22(4):227-241. [8] KURIS EO, ANDERSON GM, OSORIO C, et al. Development of a robotic spine surgery program: rationale, strategy, challenges, and monitoring of outcomes after implementation. J Bone Joint Surg Am. 2022;104(19):e83. [9] ZAWAR A, CHHABRA HS, MUNDRA A, et al. Robotics and navigation in spine surgery: a narrative review. J Orthop. 2023;44:36-46. [10] 杨帆,安晓龙,周程沛,等. 胸椎管狭窄症的微创手术治疗新进展[J].中华全科医学,2024, 22(2):292-295, 300. [11] ARRUDA H, SILVA ER, LESSA M, et al. VOSviewer and Bibliometrix. J Med Libr Assoc. 2022;110(3): 392-395. [12] KANTELHARDT SR, MARTINEZ R, BAERWINKEL S, et al. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J. 2011;20(6):860-868. [13] GERTZBEIN SD, ROBBINS SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15(1):11-14. [14] RINGEL F, STÜER C, REINKE A, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976). 2012;37(8): E496-E501. [15] DEVITO DP, KAPLAN L, DIETL R, et al. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila Pa 1976). 2010; 35(24):2109-2115. [16] ROSER F, TATAGIBA M, MAIER G. Spinal robotics: current applications and future perspectives. Neurosurgery. 2013;72 Suppl 1:12-18. [17] HYUN SJ, KIM KJ, JAHNG TA, et al. Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine (Phila Pa 1976). 2017;42(6): 353-358. [18] SCHATLO B, MOLLIQAJ G, CUVINCIUC V, et al. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine. 2014;20(6):636-643. [19] HU X, OHNMEISS DD, LIEBERMAN IH. Robotic-assisted pedicle screw placement: lessons learned from the first 102 patients. Eur Spine J. 2013;22(3):661-666. [20] KIM HJ, JUNG WI, CHANG BS, et al. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot. 2017. doi: 10.1002/rcs.1779. [21] HAN X, TIAN W, LIU Y, et al. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. 2019;30(5):615-622. [22] SCHIZAS C, THEIN E, KWIATKOWSKI B, et al. Pedicle screw insertion: robotic assistance versus conventional C-arm fluoroscopy. Acta Orthop Belg. 2012;78(2):240-245. [23] LIEBERMAN IH, HARDENBROOK MA, WANG JC, et al. Assessment of pedicle screw placement accuracy, procedure time, and radiation exposure using a miniature robotic guidance system. J Spinal Disord Tech. 2012;25(5):241-248. [24] HU X, LIEBERMAN IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. 2014; 472(6):1839-1844. [25] KIM HJ, LEE SH, CHANG BS, et al. Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976). 2015;40(2):87-94. [26] SCHATLO B, MARTINEZ R, ALAID A, et al. Unskilled unawareness and the learning curve in robotic spine surgery. Acta Neurochir (Wien). 2015;157(10):1819-1823; discussion 1823. [27] LONJON N, CHAN-SENG E, COSTALAT V, et al. Robot-assisted spine surgery: feasibility study through a prospective case-matched analysis. Eur Spine J. 2016;25(3):947-955. [28] LEFRANC M, PELTIER J. Evaluation of the ROSA™ Spine robot for minimally invasive surgical procedures. Expert Rev Med Devices. 2016; 13(10):899-906. [29] OVERLEY SC, CHO SK, MEHTA AI, Arnold PM. Navigation and robotics in spinal surgery: where are we now? Neurosurgery. 2017;80(3S):S86-S99. [30] GAO S, LV Z, FANG H. Answer to the Letter to the Editor of Qi Sun et al. concerning “Robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis of randomized controlled trials” by Gao ST, et al. (Eur Spine J; 2017: doi 10.1007/s00586-017-5333-y). Eur Spine J. 2018;27(4):933-934. [31] LAUDATO PA, PIERZCHALA K, SCHIZAS C. Pedicle screw insertion accuracy using o-arm, robotic guidance, or freehand technique: a comparative study. Spine (Phila Pa 1976). 2018; 43(6):E373-E378. [32] MENGER RP, SAVARDEKAR AR, FAROKHI F, et al. A cost-effectiveness analysis of the integration of robotic spine technology in spine surgery. Neurospine. 2018;15(3):216-224. [33] GHASEM A, SHARMA A, GREIF DN, et al. The arrival of robotics in spine surgery: a review of the literature. Spine (Phila Pa 1976). 2018; 43(23):1670-1677. [34] KHAN A, MEYERS JE, SIASIOS I, et al. Next-generation robotic spine surgery: first report on feasibility, safety, and learning curve. Oper Neurosurg (Hagerstown). 2019;17(1):61-69. [35] KOCHANSKI RB, LOMBARDI JM, LARATTA JL, et al. Image-guided navigation and robotics in spine surgery. Neurosurgery. 2019;84(6):1179-1189. [36] LI HM, ZHANG RJ, SHEN CL. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: A Meta-analysis. Spine (Phila Pa 1976). 2020;45(2):E111-E119. [37] HARIKESH PC, YANG CY, TU D, et al. Organic electrochemical neurons and synapses with ion mediated spiking. Nat Commun. 2022;13(1):901. [38] MISHRA R, NARAYANAN MDK, UMANA GE, et al. Virtual reality in neurosurgery: beyond neurosurgical planning. Int J Environ Res Public Health. 2022;19(3):1719. [39] GHAEDNIA H, FOURMAN MS, LANS A, et al. Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J. 2021;21(10):1617-1625. [40] FATIMA N, MASSAAD E, HADZIPASIC M, et al. Safety and accuracy of robot-assisted placement of pedicle screws compared to conventional free-hand technique: a systematic review and meta-analysis. Spine J. 2021;21(2):181-192. [41] MOLINA CA, PHILLIPS FM, COLMAN MW, et al. A cadaveric precision and accuracy analysis of augmented reality-mediated percutaneous pedicle implant insertion. J Neurosurg Spine. 2020;34(2):316-324. [42] JAREBI M, AWAF A, LEFRANC M, et al. A matched comparison of outcomes between percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for the treatment of lumbar disc herniation: a 2-year retrospective cohort study. Spine J. 2021;21(1):114-121. [43] RASOULI JJ, SHAO J, NEIFERT S, et al. Artificial intelligence and robotics in spine surgery. Global Spine J. 2021;11(4):556-564. [44] HUANG M, TETREAULT TA, VAISHNAV A, et al. The current state of navigation in robotic spine surgery. Ann Transl Med. 2021;9(1):86. [45] O’CONNOR TE, O’HEHIR MM, KHAN A, et al. Mazor X stealth robotic technology: a technical note. World Neurosurg. 2021;145:435-442. [46] MATUR AV, PALMISCIANO P, DUAH HO, et al. Robotic and navigated pedicle screws are safer and more accurate than fluoroscopic freehand screws: a systematic review and meta-analysis. Spine J. 2023;23(2):197-208. [47] KIM H, CHANG BS, CHANG SY. Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine. 2022;19(1):163-176. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Li Zikai, Zhang Chengcheng, Xiong Jiaying, Yang Xirui, Yang Jing, Shi Haishan. Potential effects of ornidazole on intracanal vascularization in endodontic regeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-7. |
| [3] | Lai Pengyu, Liang Ran, Shen Shan. Tissue engineering technology for repairing temporomandibular joint: problems and challenges [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [4] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [5] | Su Lintao, Jiang Jianfeng, Ma Jun, Huang Liangliang, Lei Changyu, Han Yaozheng, Kang Hui. Precise application of O-arm navigation system in thoracolumbar fractures with developmental pedicle stenosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1855-1862. |
| [6] | Liu Lin, Liu Shixuan, Lu Xinyue, Wang Kan. Metabolomic analysis of urine in a rat model of chronic myofascial trigger points [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1585-1592. |
| [7] | Su Xiaoyang, Chen Wenting, Fu Yidan, Zhao Yan, Lan Danfeng, Yang Qiuping. Correlation between Mer receptor tyrosine kinase and diabetic peripheral neuropathy in Sprague-Dawley rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1593-1599. |
| [8] | Li Kaiying, Wei Xiaoge, Song Fei, Yang Nan, Zhao Zhenning, Wang Yan, Mu Jing, Ma Huisheng. Mechanism of Lijin manipulation regulating scar formation in skeletal muscle injury repair in rabbits [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1600-1608. |
| [9] | Li Jun, Gong Jingjing, Sun Guobin, Guo Rui, Ding Yang, Qiang Lijuan, Zhang Xiaoli, Fang Zhanhai . miR-27a-3p promotes the proliferation of human hypertrophic scar fibroblasts by regulating mitogen-activated protein kinase signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1609-1617. |
| [10] | Li Huayuan, Li Chun, Liu Junwei, Wang Ting, Li Long, Wu Yongli. Effect of warm acupuncture on PINK1/Parkin pathway in the skeletal muscle of rats with chronic fatigue syndrome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1618-1625. |
| [11] | Jing Ruyi, Chen Yingxin, Cao Lei . Prognosis of deep lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1626-1633. |
| [12] | Wang Xuanqiang, Zhang Wenyang, Li Yang, Kong Weiqian, Li Wei, Wang Le, Li Zhongshan, Bai Shi. Effects of chronic exposure to low-frequency pulsed magnetic fields on contractility and morphology of the quadriceps muscle in healthy adults [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1634-1642. |
| [13] | Zhang Yuxin, Yu Cong, Zhang Cui, Ding Jianjun, Chen Yan. Differences in postural control ability between older adults with mild cognitive impairment and those with normal cognition under different single-task and dual-task conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1643-1649. |
| [14] | Zhou Panpan, Cui Yinglin, Zhang Wentao, Wang Shurui, Chen Jiahui, Yang Tong . Role of cellular autophagy in cerebral ischemic injury and the regulatory mechanism of traditional Chinese medicine [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1650-1658. |
| [15] | Yu Jingbang, Wu Yayun. Regulatory effect of non-coding RNA in pulmonary fibrosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1659-1666. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||