Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (15): 3129-3137.doi: 10.12307/2025.198
Previous Articles Next Articles
Biomechanical characteristics of different orthopedic modalities for adolescent idiopathic scoliosis based on finite element simulation analysis
Yue Bo1, 2, Cao Zhenhua3, 4, Zhang Yunfeng5, Xu Yangyang6, Jin Feng7, Su Baoke8, Wang Lidong9, Wang Xing1, Tong Ling1, Liu Qinghua1, Fang Yuan1, Sha Lirong1, Wang Haiyan1, Li Xiaohe1, Li Zhijun1#br#
- 1Department of Human Anatomy, School of Basic Medicine, Inner Mongolia Medical University (Inner Mongolia Digital Transformation Medical Engineering Technology Research Center), Hohhot 010000, Inner Mongolia Autonomous Region, China
-
Received:2023-02-28Accepted:2024-06-07Online:2025-05-28Published:2024-11-04 -
Contact:Zhang Yunfeng, Associate chief physician, Department of Imaging, Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010000, Inner Mongolia Autonomous Region, China Co-corresponding author: Li Xiaohe, Professor, Doctoral supervisor, Department of Human Anatomy, School of Basic Medicine, Inner Mongolia Medical University (Inner Mongolia Digital Transformation Medical Engineering Technology Research Center), Hohhot 010000, Inner Mongolia Autonomous Region, China -
About author:Yue Bo, Master candidate, Department of Human Anatomy, School of Basic Medicine, Inner Mongolia Medical University (Inner Mongolia Digital Transformation Medical Engineering Technology Research Center), Hohhot 010000, Inner Mongolia Autonomous Region, China; Bayannur Hospital, Bayannur 015000, Inner Mongolia Autonomous Region, China Cao Zhenhua, MD, Associate chief physician, Postdoctoral Workstation of Chinese PLA General Hospital, Beijing 100000, China; Department of Orthopedics, Third Affiliated Hospital of Jinzhou Medical University, Jinzhou 121000, Liaoning Province, China Yue Bo and Cao Zhenhua contributed equally to this article. -
Supported by:Inner Mongolia Autonomous Region Natural Science Foundation Project, No. 2021MS08086 (to WHY); 2022 Inner Mongolia Autonomous Region Health Science and Technology Plan Project, No. 202201188 (to WHY); Inner Mongolia Medical University 2020 “Achievement Transformation” Project, No. YKD2020CGZH009 (to WHY); Inner Mongolia Natural Science Foundation, No. 2020MS08124 (to LXH); Inner Mongolia Autonomous Region “Grassland Talent” Project Youth Innovation and Entrepreneurship Talent Project, No. 2020 (to LXH); Inner Mongolian Medical University Follow-Up Scientific Research Project, No. 2020 (to LXH); Inner Mongolia Science and Technology Plan Project, No. 2019GG115 (to LZJ); 2021 Inner Mongolia Autonomous Region Mongolian Medicine Collaborative Innovation Center Scientific Research Project (to LXH); 2021 Inner Mongolia Medical University Zhiyuan Talent Project (to LXH); Inner Mongolia Medical University 2021 School-Level Key Scientific Research Project, No. YKD2021ZD001 (to LXH); Inner Mongolia Education Department Higher Education Innovation Team Development Plan, No. NMGIRT2227 (to LXH)
CLC Number:
Cite this article
Yue Bo, Cao Zhenhua, Zhang Yunfeng, Xu Yangyang, Jin Feng, Su Baoke, Wang Lidong, Wang Xing, Tong Ling, Liu Qinghua, Fang Yuan, Sha Lirong, Wang Haiyan, Li Xiaohe, Li Zhijun. Biomechanical characteristics of different orthopedic modalities for adolescent idiopathic scoliosis based on finite element simulation analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(15): 3129-3137.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

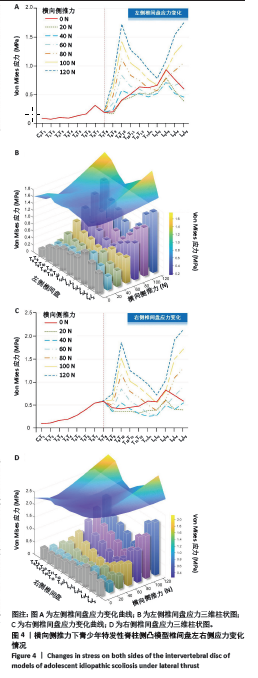
2.1 椎间盘应力 如图4A所示为横向侧推力下椎间盘左右侧的应力变化情况,C7T1-T7T8椎间盘在侧推矫正过程中应力无明显变化。红色实线表示的是模型在不加外力仅在跟随载荷下的应力,可以看出红色实线经历了向下摆动后升高的过程,20,40,60,80 N折线均存在小于红色实线的情况,节段靠上时,例如在T9T10节段,只有20 N线位于红色实线下,节段靠下时,例如在L2L3节段,应力值在20,40,60,80 N情况下均小于对照组。横向侧推力下,应力在T7T8-L4L5节段表现出一个起伏现象,如波峰位于T9T10节段(1.73 MPa,120 N),波谷位于L1L2节段(0.78 MPa,120 N)。图4B的三维柱状图和三维曲面也表现出了上述趋势,侧推力方向,三维曲面先是进行了一个短暂的下降后逐渐上升,节段方向三维曲面表现出两侧值高中间值低的“凹”形特征,与对照组状态下的柱状图趋势相比,“凹”状趋势随着侧推力变大越来越明显。 图4C,D表示了右侧椎间盘应力的变化情况,同样地,椎间盘应力在C7T1-T7T8节段无明显变化。侧推力为0 N时,T10T11-L4L5节段,右侧椎间盘应力T10T11:0.45 MPa;T11T12:0.47 MPa;T12L1:0.58 MPa;L1L2:0.57 MPa;L2L3:0.82 MPa;L3L4:0.71 MPa; L4L5:0.58 MPa;左侧椎间盘T10T11:0.51 MPa;T11T12:0.64 MPa;T12L1:0.62 MPa; L1L2:0.67 MPa;L2L3:0.94 MPa;L3L4:0.76 MPa;L4L5:0.60 MPa;侧推力为40 N时,T10T11-L4L5节段左右侧椎间盘应力均降低,其中右侧椎间盘应力T10T11:0.41 MPa; T11T12:0.31 MPa;T12L1:0.25 MPa;L1L2:0.27 MPa;L2L3:0.49 MPa;L3L4:0.40 MPa; L4L5:0.54 MPa;左侧椎间盘T10T11:0.50 MPa;T11T12:0.51 MPa;T12L1:0.46 MPa; L1L2:0.52 MPa;L2L3:0.72 MPa;L3L4:0.52 MPa;L4L5:0.46 MPa。"

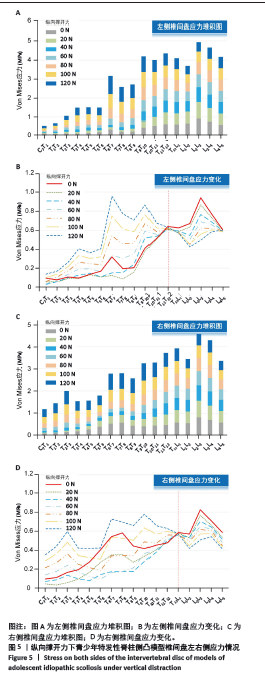
如图5所示为纵向撑开力下椎间盘左右侧应力情况,图5A中,C7T1-T5T6节段应力变化较其他节段较小,随着撑开力的增加,应力增长逐渐明显;T6T7-T9T10节段应力变化最明显,例如,T6T7节段的应力值为0.32,0.12,0.15,0.33,0.54,0.74,0.95 MPa(0,20,40,60,80,100,120 N);从图5B中可以看出,撑开力为20 N时,C7T1-T11T12节段应力线位于红色实线下,而T11T12-L4L5节段,应力线均位于红色实线下。图5C中,C7T1-T5T6节段应力变化明显且均大于左侧椎间盘应力,T9T10-L4L5节段右侧椎间盘应力小于左侧椎间盘应力,同样地,靠下的节段应力变化较为平均,靠上的节段应力变化较为明显。图5D中,在C7T1-T12L1节段,有较多的曲线位于红色实线下,而T12L1-L4L5节段,曲线均位于红色实线下,这与左侧椎间盘现象一致。"

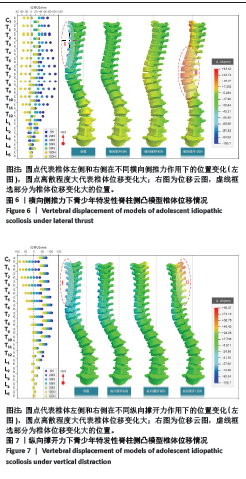
2.2 椎体位移 图6为横向侧推力下椎体的位移情况,左侧散点图表示椎体各节段左右侧的纵向位移,可以看出C7-T12椎体左侧位移点较分散,说明左侧位移变化较大,而右侧位移变化较为集中,可以理解为这些椎体发生了旋转,L1-L5椎体位移点集中,椎体发生的旋转小。脊柱只受跟随载荷时,椎体有很大的位移值,其中T7和T8的位移值最大,为-106.3 mm和-106.7 mm,随着力的增加,凸位移点大多向左移动,凹侧位移点多向右移动。脊柱的区域Ⅰ为位移变化最大的地方(-106.7 mm),方向为-U3;椎体的区域Ⅱ为正向位移最大的地方(45.42 mm)。由空载到120 N过程中,多个区域的位移由负向移动变为正向移动。 图7为纵向撑开力下椎体的位移情况,同样地,左侧散点图表示椎体各节段左右侧的纵向位移。与横向侧推力的情况相反,其椎体左侧位移变化值小,右侧位移变化值大,而且随着节段往下,椎体的位移变化越来越小,L3、L4、L5椎体位移几乎无变化。从各位移点的左右间距可以看出,每次位移变化较为一致,椎体右侧位移经历了负向位移到正向位移的变化。脊柱的Ⅰ区域为负向位移最大的地方(-106.7 mm),脊柱Ⅱ区域为正向位移最大的地方(89.47 mm),与横向侧推力不同的是,纵向撑开力下的脊柱最大位移发生在头部。"

2.3 Cobb角变化 如图8A所示,情况一中,椎体受到跟随载荷,其可分解为和,在脊柱变直的过程中,Cobb角减小,则横向分力减小;横向侧推力不变的情况下,侧推矫正的效果变好,但纵向分力变大;纵向撑开力不变的情况下,撑开矫正的效果减弱。情况二中,椎体未倾斜,横向侧推和纵向撑开的矫正效果不变。情况三中,椎体倾斜与情况一相反,此时Cobb角减小,横向侧推力减小;横向侧推力不变的情况下,侧推矫正的效果变弱,纵向分力变大;纵向撑开力不变的情况下,撑开矫正的效果减弱。 如图8B所示,胸椎Cobb角的矫正效果优于腰椎Cobb角的矫正效果,纵向撑开力下胸椎Cobb角的曲线斜率逐渐减小,而横向侧推力下胸椎Cobb角的曲线斜率是逐渐增加的,两种矫形力均在80 N时达到了正向的矫正效果。"

| [1] ROYE BD, SIMHON ME, MATSUMOTO H, et al. Establishing consensus on the best practice guidelines for the use of bracing in adolescent idiopathic scoliosis. Spine Deform. 2020;8:597-604. [2] GANJAVIAN MS, PARNIANPOUR M, GOHARI E, et al. Numerical analysis (finite element method) of brace effects on the adolescent idiopatic scolosis during 24 hours. Biomed Eng. 2014;26(3):1450046. [3] LI QY, ZHONG GB, LIU ZD, et al. Effect of asymmetric tension on biomechanics and metabolism of vertebral epiphyseal plate in a rodent model of scoliosis. Orthop Surg. 2017;9(3):311-318. [4] AROEIRA R, PERTENCE A, KEMMOKU DT, et al. The effect of hypokyphosis on the biomechanical behavior of the adolescent thoracic spine. J Braz Soc Mech Sci. 2018;40(3):1-10. [5] DUPUIS S, FORTIN C, CAOUETTE C, et al. Global postural re-education in pediatric idiopathic scoliosis: a biomechanical modeling and analysis of curve reduction during active and assisted self-correction. BMC Musculoskelet Disord. 2018;19(1):200. [6] BIDARI S, KAMYAB M, GHANDHARI H, et al. Effcacy of computer-aided design and manufacturing versus computer-aided design and fnite element modeling technologies in brace management of idiopathic scoliosis: a narrative review. Asian Spine J. 2021;15(2):271-282. [7] KONIECZNY MR, SENYURT H, KRAUSPE R. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2013;7(1):3-9. [8] WEINSTEIN SL, DOLAN LA, CHENG JC, et al. Adolescent idiopathic scoliosis. Lancet. 2008;371(9623):1527-1537. [9] GOLDBERG CJ, MOORE DP, FOGARTY EE, et al. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine. 2001;26(1):42-47. [10] HARRINGTON PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. JBJS. 1962;44(4):591-634. [11] MAJDOULINE Y, AUBIN CE, ROBITAILLE M, et al. Scoliosis correction objectives in adolescent idiopathic scoliosis. J Pediatr Orthop. 2007; 27(7):775-781. [12] MEHLMAN CT, ARAGHI A, ROY DR. Hyphenated history: the hueter- volkmann law. Am J Orthop. 1997;26(11):798-800. [13] BREKELMANS WA, POORT HW, SLOOFF TJ. A new method to analyse the mechanical behaviour of skeletal parts. Acta Orthop Scand. 1972; 43(5):301-317. [14] 张宏其, 王永福, 唐明星, 等. Lenke5型青少年特发性脊柱侧凸手术矫形的有限元研究[J]. 脊柱外科杂志,2011,9(2):112-116. [15] 邬超, 高明杰, 王建忠, 等. 有限元法分析Lenke 3型青少年特发性脊柱侧凸胸-腰椎的应力及位移变化[J]. 中国组织工程研究,2021, 25(33):5273-5280. [16] FINLEY SM, BRODKE DS, SPINA NT, et al. FEBio finite element models of the human lumbar spine. Comput Methods Biomech Biomed Eng. 2018;21(6):444-452. [17] 海涌, 潘爱星, 李永刚. 早发性脊柱侧凸不同生长棒固定方式对邻近节段生物力学的影响[J]. 中华医学杂志,2017,97(48):3768-3773. [18] CAHILL PJ, WANG W, ASGHAR J, et al. The use of a transition rod may prevent proximal junctional kyphosis in the thoracic spine following scoliosis surgery: a finite element analysis. Spine (Phila Pa 1976). 2012; 37(12):687-695. [19] WHITE AA, PANJABI MM. Clinical Biomechanics of the Spine. Philadelphia: Lippincott, 1992. [20] CAI XY, SANG DC, YUCHI CX, et al. Using finite element analysis to determine effects of the motion loading method on facet joint forces after cervical disc degeneration. Comput Biol Med. 2020;116:103519. [21] PASHA S, AUBIN CE, PARENT S, et al. Biomechanical loading of the sacrum in adolescent idiopathic scoliosis. Clin Biomech. 2014;29(3): 296-303. [22] AAKASH A, ANAND KA, ARVIND J, et al. Distraction magnitude and frequency affects the outcome in juvenile idiopathic patients with growing rods: Finite element study using a representative scoliotic spine model. Spine J. 2015;15(8):1848-1855. [23] VILLEMURE I, AUBIN CE, DANSEREAU J, et al. Simulation of progressive deformities in adolescent idiopathic scoliosis using a biomechanical model integrating vertebral growth modulation. J Biomech Eng. 2002; 124(6):784-790. [24] YE QB, WANG YP, ZHANG J, et al. A new instrumentation without fusion for the treatment of progressive idiopathic scoliosis in growing children. J Musculoskeletal Res. 2003;7(3n04):201-209. [25] 叶启彬, 邱贵兴, 王以朋, 等. 板一棍系统(PRSS)对生长中儿童和成人脊柱侧弯矫治的早期结果[J]. 中国矫形外科杂志,2001,8(1): 22-26. [26] VILLEMURE I, AUBIN CE, DANSEREAU J, et al. Biomechanical simulations of the spine deformation process in adolescent idiopathic scoliosis from different pathogenesis hypotheses. Eur Spine J. 2004;13(1):83-90. [27] STOKES IA. Analysis and simulation of progressive adolescent scoliosis by biomechanical growth modulation. Eur Spine J. 2007;16:1621-1628. [28] STOKES IA, ARONSSON DD, DIMOCK AN, et al. Endochondral growth in growth plates of three species at two anatomical locations modulated by mechanical compression and tension. J Orthop Res. 2006;24: 1327-1334. [29] CLIN J, AUBIN CÉ, SANGOLE A, et al. Correlation between immediate in-brace correction and biomechanical effectiveness of brace treatment in adolescent idiopathic scoliosis. Spine. 2010;35(18): 1706-1713. [30] MAHAR AT, BAGHERI R, OKA R, et al. Biomechanical comparison of different anchors (foundations) for the pediatric dual growing rod technique. Spine J. 2008;8(6):933-939. [31] AGARWAL A, AGARWAL AK, JAYASWAL A, et al. Effect of distraction force on growth and biomechanics of the spine: a finite element study on normal juvenile spine with dual growth rod instrumentation. Spine Deform. 2014;2:260-269. [32] 海涌, 潘爱星, 李永刚, 等. 早发性脊柱侧弯不同生长棒固定方式对邻近节段生物力学的影响[J]. 中华医学杂志,2017,97(48): 3768-3773. [33] ABOLAEHA OA, WEBER J, ROSS LT. Finite element simulation of a scoliotic spine with periodic adjustments of an attached growing rod. Conf Proc IEEE Eng Med Biol Soc. 2012;(12):5781-5785. [34] PAN A, DING H, WANG J, et al. The application of finite element analysis to determine the optimal UIV of growing-rod treatment in early-onset scoliosis. Front Bioeng Biotechnol. 2022;10:978554. [35] AKBARNIA BA, CAMPBELL RM, DIMEGLIO A, et al. Fusionless procedures for the management of early-onset spine deformities in 2011: what do we know? J Child Orthop. 2011;5(3):159-172. [36] KARAM JA, EID R, KREICHATI G, et al. Optimizing the vertical position of the brace thoracic pad: Apical rib or apical vertebra. Orthop Traumatol Surg Res. 2019;105(4):727-731. [37] GUAN T, ZHANG Y, ANWAR A, et al. Determination of three-dimensional corrective force in adolescent idiopathic scoliosis and biomechanical finite element analysis. Front Bioeng Biotechnol. 2020;8:963. [38] PEI B, LU D, WU X, et al. and Wu S. Kinematic and biomechanical responses of the spine to distraction surgery in children with early onset scoliosis: A 3-D finite element analysis. Front. Bioeng. Biotechnol. 2022;10:933341. [39] 刘小丹. 脊柱的简化模型及其在侧弯矫正中的应用[D]. 上海: 上海交通大学,2009. |
| [1] | Ye Xiaolong, Zhang Yuxuan, Fu Rongchang, Liu Yun, Yusanjiang·Wuhuer, Escar·Aimer, Ma Yuan. A three-dimensional finite element modal analysis on adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7072-7079. |
| [2] | Zheng Xiaodong, Gao Shan, Han Wenjin, Liu Lijun, Jia Menglong, Yu Longtan. Visual analysis of treatment of adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 645-653. |
| [3] | Zhang Juanjuan, Jiang Nannan, Wu Yajun, Gu Qian, He Linfei, Ji Yongxin, Liu Su. Schroth therapy combined with core strength training improves scoliosis angle in patients with mild adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5876-5882. |
| [4] | Liu Jing, Xu Chunxin, Lu Yangyang, Qu Qinquan, Zhu Qi, Guo Yulan, Shen Min. Correlation of gait parameters and muscle parameters with imaging in adolescent idiopathic scoliosis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4477-4485. |
| [5] | Wu Maodong, Su Qinglun, Huang Yiming, Shen Longying, Lu Yu, Zhao Qin. Correlation between coronal pressure variation and coronal imbalance in adolescent idiopathic scoliosis patients [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 852-856. |
| [6] | Hou Yutong, Huang Chenglan, Yang Yunxiao, Li Ya, Guo Peiwu, Yu Wenqiang, Zhao Yu, Wang Zanbo, Zeng Hong, Ma Zhenjiang, Lu Dezhi, Wang Jinwu. Correlation between lumbar spine and pelvic parameters in Lenke type 5 adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5753-5758. |
| [7] | Chang Ying, Xia Yuan, Sun Yundi, Cheng Lulu, Xiong Wenjuan, Zhao Xianghu. Effectiveness of different specific exercise therapies in treatment of adolescent idiopathic scoliosis: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5899-5904. |
| [8] | Hou Zhaomeng, Su Shaoting, Chen Longhao, Wei Guikang, Zhou Honghai. Visualization analysis of research hotspots and trends in adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3424-3430. |
| [9] | Xin Xiaoming, Gao Mingxuan, Zhang Fan, Chi Fei, Feng Junchao, Luo Wenyuan. Application of orthopedic robot-assisted screw placement in the correction of adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(36): 5790-5794. |
| [10] | Peng Lu, Duan Zhili, Li Zhenyu, Li Junhui, Li Yunhong, Wang Song, Liu Weiqiang. Research status and progress of establishment and validation of finite element model of adolescent idiopathic scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(27): 4393-4400. |
| [11] | Wang Shuai, Wang Liancheng, Zhang Shuhao, Li Fuli, Dong Jiaxing, Zhang Yajie. Correlation of the electromyography ratio of the paraspinal muscles on the convex and concave sides with Cobb angle, apical vertebra translation, and coronal balance distance in adolescent idiopathic scoliosis patients [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1402-1406. |
| [12] | Lu Yangyang, Xu Chunxin, Chen Cen, Ren Jie, Zhai Xinyi, Zhu Shenyu, Shen Min. Establishment of thoracic and abdominal volume models of adolescent idiopathic scoliosis based on three-dimensional motion capture system [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5807-5811. |
| [13] | Zhu Feilong, Zhang Ming, Wu Yu, Wang Bin, Guo Xiaoqi, Cao Jiangang, Zhu Qian, Chen Wei. Foot posture and gait in adolescent idiopathic scoliosis patients: three-dimensional morphological analysis and biomechanics evaluation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(33): 5294-5300. |
| [14] | Zhang Yufang, Guan Tianmin, Guo Qiaoge, Zhang Yufen, Guo Yanli. Digital design of personalized scoliosis orthopedic braces based on 3D printing technology [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(36): 5824-5829. |
| [15] | Fu Yu, Zhang Yunfeng, Su Baoke, Zhao Yan, Xin Daqi, Wang Haiyan, Xu Yangyang, Zhang Cong, Wang Yidan, Wang Xing, Gao Shang, En He, Cai Yongqiang, Wang Jianzhong, Wang Zhiqiang, Gao Mingjie, Li Zhijun, Ma Jierong, Li Xiaohe. Application of three-dimensional digital operation planning to individualized adolescent idiopathic scoliosis surgery [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(32): 5158-5163. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||