Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1810-1819.doi: 10.12307/2025.172
Previous Articles Next Articles
Decompression mechanism of symmetrically adduction of lumbar decompression induced resorption of herniated nucleus pulpous
Zhang Chunlin, Hou Zhaohua, Yan Xu, Jiang Yan, Fu Su, Ning Yongming, Li Dongzhe, Dong Chao, Liu Xiaokang, Wang Yongkui, Cao Zhengming, Yang Tengyue
- Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China
-
Received:2023-10-19Accepted:2024-01-25Online:2025-03-28Published:2024-10-09 -
Contact:Zhang Chunlin, MD, Chief physician, Professor, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China -
About author:Zhang Chunlin, MD, Chief physician, Professor, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China
CLC Number:
Cite this article
Zhang Chunlin, Hou Zhaohua, Yan Xu, Jiang Yan, Fu Su, Ning Yongming, Li Dongzhe, Dong Chao, Liu Xiaokang, Wang Yongkui, Cao Zhengming, Yang Tengyue. Decompression mechanism of symmetrically adduction of lumbar decompression induced resorption of herniated nucleus pulpous[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1810-1819.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
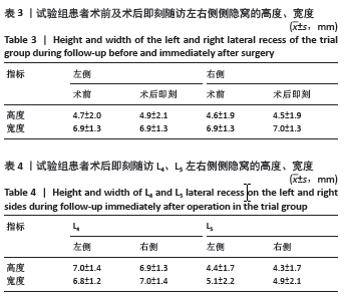
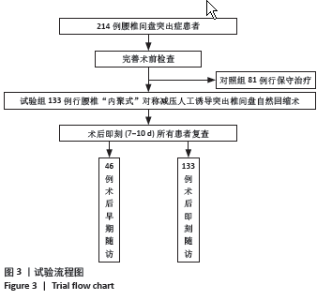
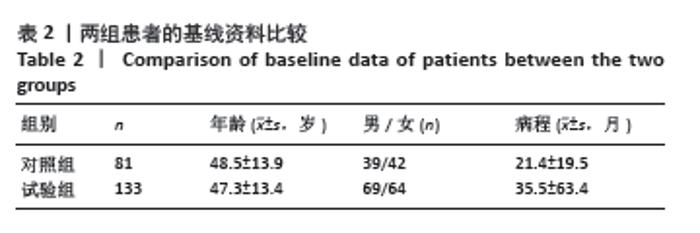
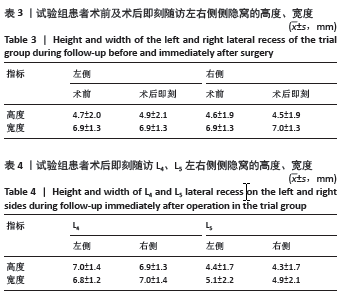
2.4 随访时临床疗效 对照组:81例腰椎间盘突出症患者就诊时及末次随访的JOA评分分别为(17.1±2.4)分和(13.3±2.1)分,差异有显著性意义(P < 0.05),患者有症状逐渐加重趋势。 试验组:133例患者的腰椎JOA评分,由术前(10.1±3.4)分提升至术后即刻(17.0±4.8)分,差异有显著性意义(P < 0.001),术后即刻有效率为91.7%。其中46例患者获术后早期随访,腰椎JOA评分由术前(9.3±5.1)分改善至(23.5±4.0)分,差异有显著性意义(P < 0.001)。46例患者中优18例,良25例,好转3例,无效0例,优良率达93.4%,优和良分别占39.1%(18/46)和54.3%(25/46)。该组有2例患者发生切口渗液,延迟愈合,经换药等保守治疗切口愈合。未发生神经损伤及死亡等并发症,也未见二次手术患者。 2.5 突出腰椎间盘的吸收情况 2.5.1 对照组 81例腰椎间盘突出症保守治疗患者171个突出腰椎间盘进行随访,就诊时及末次随访MRI分别显示突出腰椎间盘体积为(551.6±257.9) mm3和(792.2±330.4) mm3,平均体积改变率增大(53.2±44.4)%,突出腰椎间盘体积呈现增大趋势,差异有显著性意义(P < 0.001)。171个突出腰椎间盘中有4个发生了自然回缩现象,吸收比为2.3%(4/171),平均吸收率为(24.5±9.9)%。 2.5.2 试验组 133例腰椎间盘突出患者共285个突出腰椎间盘,依据突出位置:中央型126个、旁侧型153个、极外侧型6个;依据突出类型:包容型和破裂型分别为42,91例。 (1)术后即刻:①285个突出腰椎间盘中有229个发生回缩,吸收比为80.3%(229/285),平均吸收率为(21.5±20.9)%,最大吸收率为86.6%;其中轻度吸收占36.5%(104/285),中度吸收占37.5%(107/285),显著吸收占5.2%(15/285),完全吸收占1.2%(3/285);②有27个突出腰椎间盘体积不变,体积不变率为9.47%(27/285); ③有29个突出腰椎间盘体积增大,体积增大率为10.2% (29/285),最大体积增大率为32.9%;④L1-3共70个突出腰椎间盘,其中60个发生回缩,吸收比为85.7%(60/70),平均吸收率为(23.1±19.5)%,最大吸收率为86.6%;轻度吸收占42.9%(30/70),中度吸收占37.1%(26/70),显著吸收占4.3%(3/70),完全吸收占1.4%(1/70);⑤L4-5共215个突出腰椎间盘,其中169个发生回缩,吸收比为78.6%(169/215),平均吸收率为(21.0±21.3)%,最大吸收率为83.2%;轻度吸收占25.9%(74/215),中度吸收占28.4%(81/215),显著吸收占4.5%(13/215),完全吸收占1.2%(1/215);⑥285个突出腰椎间盘中显著及完全吸收占6.3%,其中上腰椎与下腰椎分别为5.7%和6.5%,二者无统计学差异(P > 0.05)。 (2)术后早期:133例腰椎间盘突出患者中有46例共101个突出腰椎间盘获术后早期随访,术前与术后早期的平均体积分别为(658±395) mm3和(392±273) mm3,差异有显著性意义(P < 0.001)。101个突出腰椎间盘中有95个发生回缩,轻度吸收占29.7%(30/101),中度吸收占 33.7%(34/101),显著吸收占23.7%(24/101),完全吸收占6.9%(7/101),吸收比为94%(95/101),平均吸收率为(36.9±23.7)%,最大吸收率为100%,显著及完全吸收30.6%。101个突出腰椎间盘中有3个体积未发生变化,突出腰椎间盘体积不变率为2.97%(3/101);还有3个突出腰椎间盘体积增大,体积增大比为2.97%(3/101),体积增大率分别为6.7%,8.7%和30.9%(该突出腰椎间盘术前与术后早期体积分别是97 mm3 和127 mm3)。 2.6 侧隐窝测量结果 如表3所示,试验组左右两侧侧隐窝的高度、宽度术前术后对比均无统计学差异(P > 0.05)。如表4所示,试验组患者术后即刻随访L4、L5左右侧侧隐窝的高度、宽度对比均无统计学差异(P > 0.05)。"
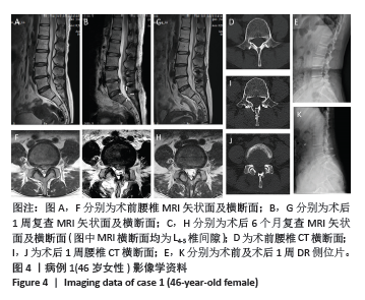
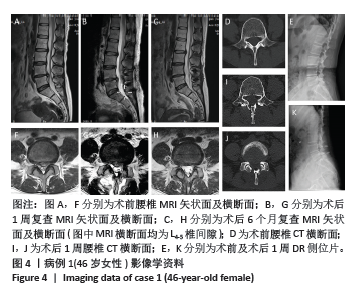
2.7 棘突韧带复合体后移距离结果 术前椎体后缘-棘突韧带复合体正中内表面的平均距离为(16.3±2.6) mm,术后即刻为(21.5±3.4) mm,差异有显著性意义(P < 0.001)。棘突韧带复合体平均后移距离为(5.2±2.8) mm,其中L4的棘突韧带复合体平均后移距离为(5.4±2.9) mm,L5的棘突韧带复合体平均后移距离为(4.9±2.6) mm,两者无统计学差异(P > 0.05)。 2.8 典型病例 病例1:女性患者,46岁。主诉:左下肢疼痛、麻木、无力1个月;查体:左下肢直腿抬高试验阳性(+),肌力IV级;诊断为L4-5、L2-3腰椎间盘突出症,见图4。术前MRI T2图像(图4A,F)显示L4-5巨大椎间盘突出及L2-3椎间盘突出,导致相应部位神经受压,考虑责任椎间盘的因素,仅行L4-5节段 SALD-iRHNP减压。术后1周MRI T2图像(图4B,G)显示局部神经减压状态,L4-5 突出腰椎间盘仍然存在并与硬膜囊接触,但术后患者左下肢疼痛明显减轻;CT图像(图4D)显示术前侧隐窝形态,侧隐窝高度为7.19 mm(左)及8.95 mm(右),宽度为8.82 mm (左)及9.04 mm(右),术后1周时棘突韧带复合体向后移位了4.42 mm(图4I)。图4J显示 SALD-iRHNP手术未涉及侧隐窝后方骨质也未损伤关节突关节解剖结构。术后6个月复查MRI T2图像(图4C,H)显示L4-5腰椎间盘突出发生了完全回缩,但L2-3突出腰椎间盘未行手术仍然存在。突出L4-5的突出椎间盘体积术前为801 mm3,术后1周为680 mm3,术后6个月为110 mm3,对应的回缩率分别为15.1%和86.2%,6个月时完全吸收。未行手术治疗的突出L2-3的突出椎间盘体积对应L4-5治疗时间阶段的体积分别为315,362,337 mm3,无明显变化。X射线侧位片(图4E,K)显示患者术前腰椎及术后微型钛钢板内固定位置良好。术后6个月JOA评分由术前15分提升至26分,改善率为78.5%,疗效为优。患者左下肢疼痛及麻木症状基本消失,肌力恢复正常至V级,患者满意。该病例表明SALD-iRHNP对突出腰椎间盘(L4-5)有良好诱导发生iRHNP的作用,未行该手术者(L2-3)则不发生回缩。"

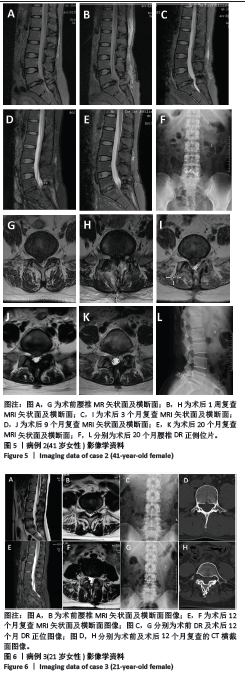
病例2:女性患者,41岁。主诉:右下肢疼痛、麻木半个月;查体:右下肢直腿抬高试验阳性(+),肌力V级;诊断为L5-S1腰椎间盘突出症(破裂型),见图5。术前MRI T2图中L5-S1巨大椎间盘右侧突出,相应部位神经受压,突出腰椎间盘体积为851 mm3(图5A,F)。MRI T2图像显示该患者行L4-5节段 SALD-iRHNP减压术后即刻突出腰椎间盘仍与硬膜囊接触(图5B,G),但术后即刻患者即感右下肢疼痛及麻木感减轻,突出腰椎间盘体积为872 mm3。MRI T2图像显示术后3个月突出腰椎间盘缩小(图5C,H),体积减少至539 mm3,回缩率为36.3%。MRI T2图像显示术后9个月突出腰椎间盘进一步缩小至112 mm3,发生了完全回缩(图4D,I),回缩率为86.8%。MRI T2图像显示术后20个月仍然保持iRHNP完全回缩现象(图5E,J),回缩率为87.8%,突出腰椎间盘体积为103 mm3。患者腰椎JOA评分由术前23分提升至术后20个月28分,改善率为83.3%,疗效为优。 病例3:女性患者,21岁。主诉:双下肢疼痛、麻木1个月;查体:双下肢直腿抬高试验阳性(+),肌力正常;诊断为腰椎间盘突出症(L4-5包容型及L5-S1脱垂型),见图6。术前MRI T2图像(图6A,B)显示L4-5及L5-S1巨大脱垂型椎间盘突出,相应部位神经受压。患者行2节段 SALD-iRHNP减压,术后即感双下肢疼痛及麻木减轻。术后12个月MRI T2图像(图6E,F)显示突出腰椎间盘体积显著减小,L4-5及L5-S1突出椎间盘体积分别从术前302 mm3和561 mm3,减小至术后早期219 mm3和104 mm3,回缩率分别为27.4%和81.5%,L5-S1椎间盘完全回缩。术前及术后X射线图像(图6C,G)显示微型钛钢板位置良好。术前CT横截面如图6D所示,术后12个月复查CT时,双侧椎板减压槽已经发生了良好骨性愈合(图6H),腰椎管接近正常解剖形态。患者术后早期随访,JOA评分从术前21分提高至术后早期27分,改善率为75%,疗效为优。患者感双下肢疼痛及麻木基本消失,疗效满意。 2.9 不良事件 试验组2例患者术后出现切口渗液,经换药愈合后延迟拆线。试验组患者均未出现死亡、神经损伤、脊柱不稳定等不良事件。 2.10 植入物与宿主的生物相容性 腰椎内固定接骨板植入物生物相容性良好,所有患者目前尚未观察到植入物周围感染、过敏反应、免疫反应及排斥反应等。"
| [1] BENZAKOUR T, IGOUMENOU V, MAVROGENIS AF, et al. Current concepts for lumbar disc herniation. Int Orthop. 2019;43(4):841-851. [2] AMIN RM, ANDRADE NS, NEUMAN BJ. Lumbar disc herniation. Curr Rev Musculoskelet Med. 2017;10:507-516. [3] SHEPARD N, CHO W. Recurrent Lumbar Disc Herniation: A Review. Global Spine J. 2019;9(2):202-209. [4] ZHANG C, LI D, WANG C, et al. Cervical Endoscopic Laminoplasty for Cervical Myelopathy. Spine (Phila Pa 1976). 2016;41 Suppl 19:B44-B51. [5] FU S, ZHANG C, YAN X, et al. Volumetric Changes in Cervical Disc Herniation: Comparison of Cervical Expansive Open-door Laminoplasty and Cervical Microendoscopic Laminoplasty. Spine (Phila Pa 1976). 2022;47(7):E296-E303. [6] FU S, ZHANG C, YAN X, et al. A New Automated AI-Assisted System to Assess Cervical Disc Herniation. Spine (Phila Pa 1976). 2022;47(16): E536-E44. [7] ZHANG C, FU S, YAN X, et al. Cervical microendoscopic laminoplasty-induced clinical resolution of disc herniation in patients with single- to three-level myelopathy. Sci Rep. 2022;12(1):18854. [8] 朱安迪, 张春霖, 严旭, 等. 对称、非对称减压与保守治疗后脊髓型颈椎病突出椎间盘体积变化的中长期对比观察[J]. 中华外科杂志,2023,61(8):666-674. [9] 牛策号, 张春霖, 严旭, 等. 椎体后方结构及对突出椎间盘体积测量的影响[J]. 中国组织工程研究,2023,27(18):2897-2902. [10] 李莹, 李龙, 严旭, 等. 内镜下微创颈椎管成形术“诱导”突出颈椎间盘自然吸收的初步观察[J]. 中国实用医刊,2020,47(10): 15-19. [11] 王志强, 龙农. 腰椎侧隐窝狭窄的CT诊断[J]. 郴州医学高等专科学校学报,2002,4(3):16-17. [12] BOGDUK N. Functional anatomy of the spine. Handb Clin Neurol. 2016; 136:675-688. [13] KARIMI A, SHOJAEI A, TEHRANI P. Mechanical properties of the human spinal cord under the compressive loading. J Chem Neuroanat. 2017;86:15-18. [14] SINGH A, LU Y, CHEN C, et al. Mechanical properties of spinal nerve roots subjected to tension at different strain rates. J Biomech. 2006; 39(9):1669-1676. [15] DOBRAN M, MANCINI F, PARACINO R, et al. Laminectomy versus open-door laminoplasty for cervical spondylotic myelopathy: A clinical outcome analysis. Surg Neurol Int. 2020;11:73. [16] ZHANG Z, WANG LN, SONG YM, et al. Comparison of long-term clinical and radiographic outcomes between alternative-level and all-level fixation unilateral open-door laminoplasty. Spine J. 2020;20(11): 1761-1769. [17] TOPP KS, BOYD BS. Structure and Biomechanics of Peripheral Nerves: Nerve Responses to Physical Stresses and Implications for Physical Therapist Practice. Phys Ther. 2006;86(1):92-109. [18] YU P, MAO F, CHEN J, et al. Characteristics and mechanisms of resorption in lumbar disc herniation. Arthritis Res Ther. 2022;24(1): 205. [19] ZHONG M, LIU JT, JIANG H, et al. Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain Physician. 2017;20(1): E45-E52. [20] KARABEKIR HS, YILDIZHAN A, BALCI C, et al. Spontaneous regression of lumbar disc herniation. Neurosciences (Riyadh). 2007;12(1): 76-78. [21] DELGADO-LÓPEZ PD, RODRíGUEZ-SALAZAR A, MARTíN-ALONSO J, et al. [Lumbar disc herniation: Natural history, role of physical examination, timing of surgery, treatment options and conflicts of interests]. Neurocirugia (Astur). 2017;28(3):124-134. |
| [1] | Lu Qi, Sun Maji, Wang Xuezhi, Song Ting, Ma Yiming, Yuan Feng, Chen Hongliang. Two visual arthroplasty techniques for L5-S1 disc herniation: a half-year follow-up evaluation of clinical outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1841-1847. |
| [2] | Feng Zhimeng, Sun Ning, Sun Zhaozhong, Li Yuefei, Liu Changzhen, Li Sa. Three-dimensional image reconstruction can safely assist one-hole split endoscope in treatment of #br# L5/S1 far lateral lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1876-1882. |
| [3] | Zhi Fang, Zhu Manhua, Xiong Wei, Lin Xingzhen. Analgesic effect of acupuncture in a rat model of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 936-941. |
| [4] | Yang Yu, Li Yinghao, Duo Zhuangzhi, Zhou Dingrong. Effect of overall functional physical exercise on lumbar biomechanics in patients with lumbar disc herniation after surgery [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7096-7101. |
| [5] | Zhang Ziyu, Chen Longhao, Sheng Wei, Lyu Hanzhe, Shen Ying, Wang Binghao, Lyu Zhizhen, Lyu Lijiang. Application of artificial intelligence in the diagnosis and treatment of lumbar disc herniation: evolution towards standardization, efficiency, and precision of diagnosis and treatment methods [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6269-6276. |
| [6] | Bai Liang, Fu Su, Yan Xu, Zhang Chunlin, Li Ying . Measurement of intervertebral disc height and analysis of strength after induced resorption of herniated nucleus pulpous [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5785-5794. |
| [7] |
Wang Qianliang, Zhang Qianzhongyi, Peng Yujian, Yan Jun.
Effects of unilateral biportal endoscopic transforaminal lumbar interbody fusion on paraspinal muscles
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5862-5868.
|
| [8] | Zhang Ruofan, Guan Huanhuan, He Zhuoqun, Zhang Yunfeng, Jin Feng, Wang Zhiqiang, Wang Jianzhong, Li Xiaohe, Zhu Yong, Wang Haiyan, Zhang Kai. Effect of minimally invasive interbody fusion device height on lumbar biomechanics in patients with adolescent lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4421-4429. |
| [9] | Gu Jiangpeng, Chen Xujing, Liu Yikang, Guo Wei, Liu Xiaomin, Wang Fei, Feng Wei. Short-term effect of manipulation therapy for lumbar disc herniation quantitatively evaluated by three-dimensional scoliosis angle [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4552-4559. |
| [10] | Wang Qianliang, Chen Jianpeng, Wang Yuanbin, Yan Jun. Mechanism of circ05188 targeting miR-199a-5p involved in nociceptive hypersensitivity in a rat model of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4230-4238. |
| [11] | Gao Haoran, Zhang Heling, Jia Fanglin, Guo Di, Jing Li, Shi Yaozhou, Song Hanlin, Gao Xiao, Feng Hu. Risk factors related to intradural lumbar disc herniation analyzed by propensity score matching [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(15): 3199-3205. |
| [12] | Yin Hao, Ji Meiqi, Hu Zhixiang, Wu Han, Lyu Heng, Li Shengyun, Li Lei, Zhai Chuntao, Lyu Yue. Comparison and evaluation of three different methods for preparing rat models of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 2930-2936. |
| [13] | Cao Zhengpei, Lu Shengsheng, Zhang Jiahuan, Wang Xiaoying. Effects of silver needle comprehensive therapy on the ultrasonographic morphology of multifidus muscles in patients with lumbar disc herniation: an ultrasound morphologic assessment [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2261-2267. |
| [14] | Yu Weijie, Liu Aifeng, Chen Jixin, Guo Tianci, Jia Yizhen, Feng Huichuan, Yang Jialin. Advantages and application strategies of machine learning in diagnosis and treatment of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1426-1435. |
| [15] | He Xinyu, Zhou Honghai, Jiang Hong, Ma Zhijia, Su Shaoting, Lin Zehong, Tian Junming, Chen Longhao, Liu Baijie. Changes in lumbosacral sagittal plane parameters of L5/S1 disc herniation reabsorption [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1330-1335. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||