Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1783-1788.doi: 10.12307/2025.105
Previous Articles Next Articles
Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems
Chen Xi1, 2, Tang Tao1, 2, Chen Tongbing1, 2, Li Qing1, 2, Zhang Wen3
- 1Changzhou First People’s Hospital, Changzhou 213003, Jiangsu Province, China; 2Third Affiliated Hospital of Soochow University, Changzhou 213003, Jiangsu Province, China; 3Orthopedic Institute, Suzhou Medical College, Soochow University, Suzhou 215006, Jiangsu Province, China
-
Received:2023-10-07Accepted:2023-12-14Online:2025-03-28Published:2024-10-09 -
Contact:Zhang Wen, Master, Senior experimentalist, Orthopedic Institute, Suzhou Medical College, Soochow University, Suzhou 215006, Jiangsu Province, China -
About author:Chen Xi, MD, Associate researcher, Changzhou First People’s Hospital, Changzhou 213003, Jiangsu Province, China; Third Affiliated Hospital of Soochow University, Changzhou 213003, Jiangsu Province, China -
Supported by:National Natural Science Foundation of China (General Program), No. 82072410 (to CX)
CLC Number:
Cite this article
Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

2.1 模型上的变形量分布分析 所有模型在各载荷作用下的最大变形量都发生在股骨头,这与加载载荷的位置相符合。因皮质骨、松质骨和内固定系统的材料属性为各项同性,所以结果显示随着载荷增大,模型上的变形量随着增大,基本呈线性。在同种载荷作用下,所有固定组模型的变形量都高于生理组,见图3。其中PFNA组的变形在术后组中是最小的,DHS+DS组最大;2 100 N载荷作用时,各组模型上的最大变形量分布:Intact组为2.15 mm,PFNA组为2.90 mm,PFLP组为3.30 mm,PCCP组为3.40 mm,DHS+DS组为4.22 mm。700 N和1 400 N的变形量分布趋势与2 100 N载荷保持一致。为了便于比较各组之间的差异,同时与经典的验证文献做比较[7],将变形量换算成压缩刚度来呈现更为直观,压缩刚度的(计算公式是载荷/变形量,单位N/mm)结果为:Intact组(979.02 N/mm) > PFNA组(724.14 N/mm) > PFLP组(630.63 N/mm) > PCCP组(617.656 N/mm) > DHS+DS组(532.99 N/mm),完整的生理组模型的压缩刚度明显高于所有的手术组模型,该结果提示患者骨折后,经内固定系统能起到有效的复位和固定作用,但模型上的力学稳定性均有不同程度的下降。"


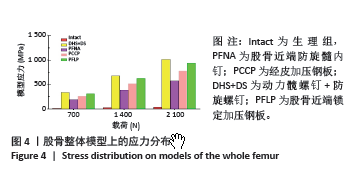
2.2 模型上最大等效应力分布分析 随着压缩载荷的增加,模型上的应力峰值也随着增大,各种载荷作用下,术后各模型上的应力峰值远高于Intact组(图4,5),应力峰值均集中分布于内固定上(图6),说明随着内固定的置入,术后模型呈现应力遮挡效应。当700 N作用时,PFNA组应力峰值为191.96 MPa,PCCP组为258.83 MPa,PFLP组为312.66 MPa,DHS+DS组为338.849 MPa,PFNA组最大应力峰值分布于防旋螺钉和髓内钉连接的位置,其他内固定组上的最高应力均分布于骨折线处,表明因骨折造成模型上的剪切力增加。当载荷增加到3倍体质量2 100 N时,DHS+DS组的应力峰值高达1 015.47 MPa,PFLP组为937.98 MPa,该数值均超过钛合金的屈服强度[24],提示在高载荷的持续作用下,内固定上可能会出现断钉的风险。在各级载荷作用下通过查看整体模型的Von Mises应力分布,可得到各组模型的分布趋势:Intact组< PFNA组< PCCP组< PFLP组< DHS+DS组。"
| [1] RAAS C, HOFMANN-FLIRI L, HÖRMANN R, et al. Prophylactic augmentation of the proximal femur: an investigation of two techniques. Arch Orthop Trauma Surg. 2016;136(3):345-351. [2] CHO HM, CHOI SM, PARK JY, et al. A finite element analysis and cyclic load experiment on an additional transcortical-type hole formed around the proximal femoral nail system’s distal locking screw. BMC Musculoskelet Disord. 2022;23(1):92. [3] KOVALAK E, ERMUTLU C, ATAY T, et al. Management of unstable pertrochanteric fractures with proximal femoral locking compression plates and affect of neck-shaft angle on functional outcomes. J Clin Orthop Trauma. 2017;8(3):209-214. [4] LI S, SU Z, ZHU J, et al. The importance of the thickness of femoral lateral wall for treating intertrochanteric fractures: a finite elements analysis. Sci Rep. 2023;13(1):12679. [5] SHEEHAN KJ, SOBOLEV B, GUY P. Mortality by Timing of Hip Fracture Surgery: Factors and Relationships at Play. J Bone Joint Surg Am. 2017;99(20):e106. [6] KIM J, OH C, KIM B, et al. Structure-mechanical analysis of various fixation constructs for basicervical fractures of the proximal femur and clinical implications; finite element analysis. Injury. 2023;54(2): 370-378. [7] GOMEZ-VALLEJO J, BLANCO-RUBIO N, LORENZO-LOPEZ R, et al. Outcomes of basicervical femoral neck fracture treated with percutaneous compression plate (PCCP). Injury. 2021;52S42-S46. [8] CHEN Y, LI H, DAI L, et al. Imaging observation of percutaneous compression plate use in promoting femoral neck fracture healing. J Int Med Res. 2021;49(8):030006052110335. [9] ZHU J, LI Y, ZHANG Y, et al. Clinical Outcome and Biomechanical Analysis of Dynamic Hip Screw Combined with Derotation Screw in Treating Displaced Femoral Neck Fractures Based on Different Reduction Qualities in Young Patients (≤65 Years of Age). Biomed Res Int. 2022; 2022:9505667. [10] DING K, ZHU Y, WANG H, et al. A comparative Study of Novel Extramedullary Fixation and Dynamic Hip Screw in the Fixation of Intertrochanteric Fracture: A Finite-Element Analysis. Front Surg. 2022;9:911141. [11] 恽常军, 钱文杰, 张杰, 等. 肱骨近端锁定接骨板固定治疗Vancouver B1型股骨假体周围骨折生物力学特性的有限元分析[J]. 中华创伤骨科杂志,2021,23(9):798-803. [12] 艾克白尔·吐逊, 阿吉木·克热木, 谢增如, 等. 两种内固定方式固定青壮年不稳定型股骨颈骨折生物力学特性的有限元分析[J]. 中华创伤骨科杂志,2020,22(9):793-798. [13] SUN H, ZHANG H, WANG T, et al. Biomechanical and Finite-Element Analysis of Femoral Pin-Site Fractures Following Navigation-Assisted Total Knee Arthroplasty. J Bone Joint Surg Am. 2022;104(19):1738-1749. [14] LI J, WANG M, LI L, et al. Finite element analysis of different configurations of fully threaded cannulated screw in the treatment of unstable femoral neck fractures. J Orthop Surg Res. 2018;13(1):272. [15] GARDNER MP, CHONG ACM, POLLOCK AG, et al. Mechanical evaluation of large-size fourth-generation composite femur and tibia models. Ann Biomed Eng. 2010;38(3):613-620. [16] HEINER AD. Structural properties of fourth-generation composite femurs and tibias. J Biomech. 2008;41(15):3282-3284. [17] MA L, ZHOU Y, ZHANG Y, et al. Biomechanical evaluation with finite element analysis of the reconstruction of femoral tumor defects by using a double-barrel free vascularized fibular graft combined with a locking plate. Int J Clin Exp Med. 2014;7(9):2425-2434. [18] CHANG C, CHEN Y, LI C, et al. Role of the compression screw in the dynamic hip–screw system: A finite-element study. Medical Engineering & Physics. 2015;37(12):1174-1179. [19] ME T, KE T, MAR F, et al. Stress and strain distribution within the intact femur: compression or bending? Med Eng Phys. 1996;18(2):122-131. [20] CUI Y, XING W, PAN Z, et al. Characterization of novel intramedullary nailing method for treating femoral shaft fracture through finite element analysis. Exp Ther Med. 2020;20(2):748-753. [21] WANG J, MA J, LU B, et al. Comparative finite element analysis of three implants fixing stable and unstable subtrochanteric femoral fractures: Proximal Femoral Nail Antirotation (PFNA), Proximal Femoral Locking Plate (PFLP), and Reverse Less Invasive Stabilization System (LISS). Orthop Traumatol Surg Res. 2020;106(1):95-101. [22] 张睿, 罗鹏, 胡炜, 等. 新型股骨近端内侧支撑钢板治疗股骨反转子间骨折的生物力学研究[J]. 中国修复重建外科杂志,2017,31(2): 165-170. [23] WANG Y, CHEN W, ZHANG L, et al. Finite Element Analysis of Proximal Femur Bionic Nail (PFBN) Compared with Proximal Femoral Nail Antirotation and InterTan in Treatment of Intertrochanteric Fractures. Orthop Surg. 2022;14(9):2245-2255. [24] NAVARRO M, MICHIARDI A, CASTA OO, et al. Biomaterials in orthopaedics. J R Soc Interface. 2008;5(27):1137-1158. [25] CHEUNG CL, ANG SB, CHADHA M, et al. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia. 2018;4(1):16-21. [26] HELWIG P, FAUST G, HINDENLANG U, et al. Finite element analysis of four different implants inserted in different positions to stabilize an idealized trochanteric femoral fracture. Injury. 2009;40(3):288-295. [27] KWAK DK, KIM WH, LEE SJ, et al. Biomechanical Comparison of Three Different Intramedullary Nails for Fixation of Unstable Basicervical Intertrochanteric Fractures of the Proximal Femur: Experimental Studies. Biomed Res Int. 2018;2018:7618079. [28] PAPINI M, ZDERO R, SCHEMITSCH EH, et al. The biomechanics of human femurs in axial and torsional loading: comparison of finite element analysis, human cadaveric femurs, and synthetic femurs. J Biomech Eng. 2007;129(1):12-19. [29] HEINER AD, BROWN TD. Structural properties of a new design of composite replicate femurs and tibias. J Biomech. 2001;34:773-781. [30] CRISTOFOLINI L, VICECONTI M, CAPPELLO A, et al. Mechanical validation of whole bone composite femur model. J Biomech. 1996; 29(4):525-535. [31] WANG H, YANG W, DING K, et al. Biomechanical study on the stability and strain conduction of intertrochanteric fracture fixed with proximal femoral nail antirotation versus triangular supporting intramedullary nail. Int Orthop. 2021;46(2):341-350. [32] BRANDT SE, LEFEVER S, JANZING HMJ, et al. Percutaneous compression plating (PCCP) versus the dynamic hip screw for pertrochanteric hip fractures: preliminary results. Injury. 2002;33:413-428. [33] KRISCHAK GD, AUGAT P, BECK A, et al. Biomechanical comparison of two side plate fixation techniques in an unstable intertrochanteric osteotomy model: Sliding Hip Screw and Percutaneous Compression Plate. Clin Biomech. 2007;22(10):1112-1118. [34] 张凯瑞. 动力髋螺钉与经皮加压钢板固定股骨转子间骨折的三维有限元分析[D]. 广州:南方医科大学,2009. [35] SOYLEMEZ M, OZKAN K, T RKMEN I, et al. A biomechanical comparison of proximal femoral nails and locking proximal anatomic femoral plates in femoral fracture fixation A study on synthetic bones. Indian J Orthop. 2015;49(3):347. [36] IBRAHIM S, MELEPPURAM JJ. A retrospective analysis of surgically-treated complex proximal femur fractures with proximal femoral locking compression plate. Rev Bras Ortop. 2017;52(6):644-650. [37] GAO Z, WANG M, SHEN B, et al. Treatment of Pauwels type III femoral neck fracture with medial femoral neck support screw: a biomechanical and clinical study. Sci Rep. 2021;11(1):21418. [38] RAINA DB, MARKEVICIUTE V, STRAVINSKAS M, et al. A New Augmentation Method for Improved Screw Fixation in Fragile Bone. Front Bioeng Biotechnol. 2022;10:816250. [39] ZENG W, LIU Y, HOU X. Biomechanical evaluation of internal fixation implants for femoral neck fractures: A comparative finite element analysis. Comput Meth Prog Bio. 2020;196:105714. [40] NODA M, NAKAMURA Y, ADACHI K, et al. Dynamic finite element analysis of implants for femoral neck fractures simulating walking. J Orthop Surg Res. 2018;26(2):230949901877789. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [3] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [4] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [5] | Li Shuai, Liu Hua, Shang Yonghui, Liu Yicong, Zhao Qihang, Liu Wen. Stress distribution on the maxilla when wearing the Twin-block appliance for Class II malocclusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 881-887. |
| [6] | Zhou Zonghao, Luo Siyang, Chen Jiawen, Chen Guangneng, Feng Hongchao. Finite element analysis of bioabsorbable plates versus miniature titanium plates in mandibular fracture fixation in different bone qualities [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 818-826. |
| [7] | Chen Yilong, Zhang Xu, Li Hong. Mechanical analysis of fiber post combined with different crown restorations for endodontically treated non-carious cervical lesions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 866-871. |
| [8] | Song Xubin, Wu Dou, Zhao Enzhe, Zhang Xingyu, Zhang Xiaolun, Wang Chuheng. Finite element analysis of a new femoral neck spiral blade system to treat femoral intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7041-7047. |
| [9] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| [10] | Xu Xin, Wurikaixi·Aiyiti, Lyu Gang, Maimaiaili·Yushan, Ma Zhiqiang, Ma Chao. Finite element analysis of four different internal fixation methods for complex acetabular double-column fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7063-7071. |
| [11] | Ma Shuangshuang, Gao Dedong, Shan Zhongshu, Xu Wenxu, Lu Zhirui. Finite element analysis and biomechanical validation of revision pedicle screw placement [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7087-7095. |
| [12] | Zhang Ziyi, Qin Qi, Alimujiang·Yusufu, Liu Yuzhe, Yusufu·Reheman, Ran Jian. Biomechanical analysis of three internal fixation schemes for Pauwels type III femoral neck fractures in young adults [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7102-7108. |
| [13] | Ma Tao, Li Xing, Wei Yajun, Deng Juncai. Effects of lateral screw-rod placement positions on segmental range of motion, internal fixation and cage stress during oblique lumber interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7165-7172. |
| [14] | Xu Tianyu, Chen Modi, Xie Mingru, Ye Xinghua, Pan Zhaohui. Finite element analysis of biomechanical effect of medial or lateral malleolar ligament defects on its neighboring core tendons [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7223-7230. |
| [15] | Zhuang Yan, Wang Xinyu, Cao Yilin, Ding Yuanxin, Wang Jiaqi, Yu Miao, Luan Chunyang, Ding Yuansheng. Three-dimensional finite element analysis of personalized orthodontic devices for 3D printed maxillary single-rooted rotated tooth [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6409-6415. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||





