Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (33): 7102-7108.doi: 10.12307/2025.849
Previous Articles Next Articles
Biomechanical analysis of three internal fixation schemes for Pauwels type III femoral neck fractures in young adults
Zhang Ziyi1, 2, Qin Qi1, 2, Alimujiang·Yusufu1, 2, Liu Yuzhe1, 2, Yusufu·Reheman1, 2, Ran Jian1, 2
- 1Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous region, China; 2Sixth Affiliated Hospital of Xinjiang Medical University, Urumqi 830092, Xinjiang Uygur Autonomous region, China
-
Received:2024-05-13Accepted:2024-08-12Online:2025-11-28Published:2025-04-12 -
Contact:Ran Jian, Chief physician, Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous region, China; Sixth Affiliated Hospital of Xinjiang Medical University, Urumqi 830092, Xinjiang Uygur Autonomous region, China -
About author:Zhang Ziyi, Master candidate, Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous region, China; Sixth Affiliated Hospital of Xinjiang Medical University, Urumqi 830092, Xinjiang Uygur Autonomous region, China -
Supported by:Xinjiang Uygur Autonomous Region Graduate Innovation Project, No. XJ2023G186 (to AY)
CLC Number:
Cite this article
Zhang Ziyi, Qin Qi, Alimujiang·Yusufu, Liu Yuzhe, Yusufu·Reheman, Ran Jian. Biomechanical analysis of three internal fixation schemes for Pauwels type III femoral neck fractures in young adults[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7102-7108.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
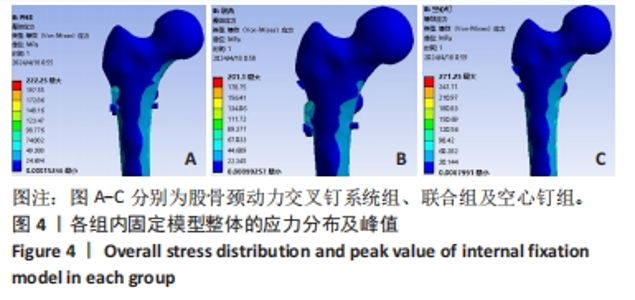
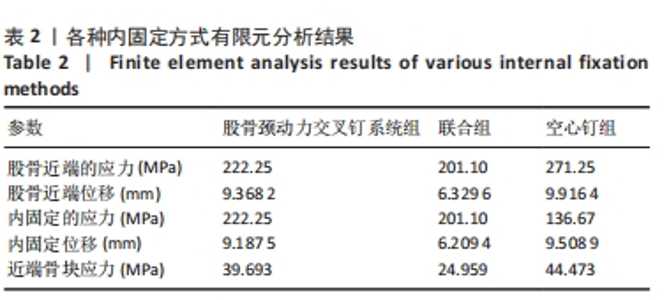
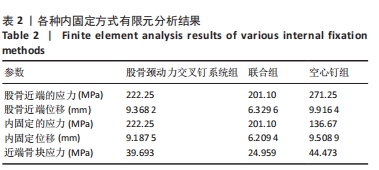
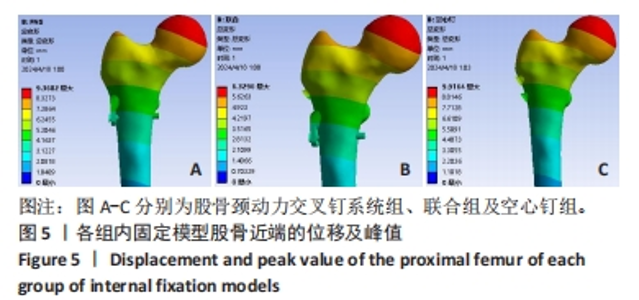
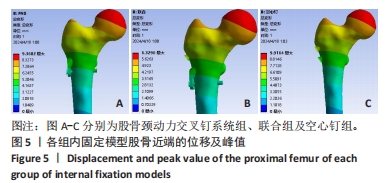
2.1 股骨近端的应力分布及峰值 3种固定模型整体的主要应力分布都集中在骨折端周围,特别是靠近骨折端下方的区域。这是因为骨折端是力学传递的关键点,承受着骨折两端相对运动所产生的应力和应变。空心钉组的应力峰值最高,为271.25 MPa,提示在空心钉组内固定模型下,骨折端及其周围区域可能面临更高的应力风险,需要特别注意骨折愈合过程中的力学环境。FNS组的应力峰值为222.25 MPa,较空心钉组低,这个峰值表明在FNS组内固定模型下,骨折端及其周围区域承受了相对较低的应力。联合组的应力峰值为201.1 MPa,与FNS组相比更低,意味着联合组的内固定模型在分散应力或降低应力集中方面表现最好。见图4及表2。"

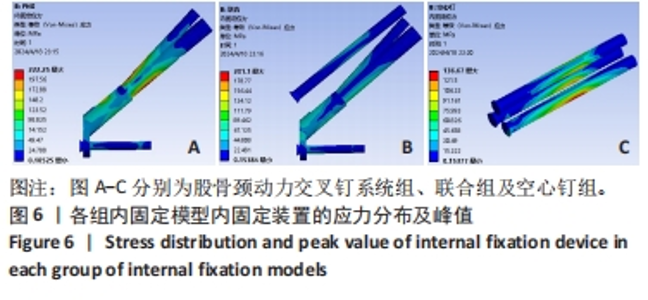
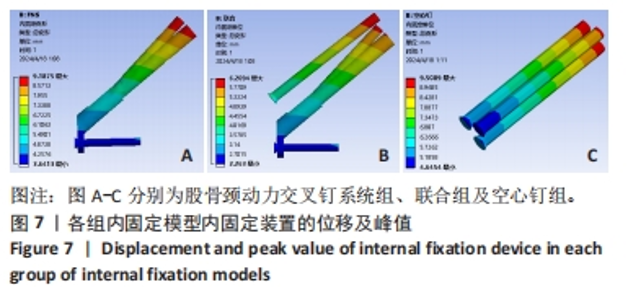
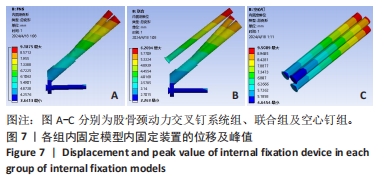
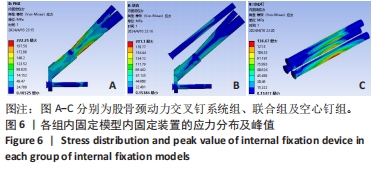
2.3 内固定装置的应力分布及峰值 在对比3种不同的内固定装置模型时,发现这些模型的应力分布主要集中在骨折断端处的螺钉表面,并从该处向两侧逐渐延伸。空心钉组的应力主要分布在骨折端周围,最下方的螺钉承受着较最高的应力,实现了较好的应力分散效果,应力峰值达到136.67 MPa,是3组中应力峰值最低的,但是从应力分布云图上看,其显示出较高的应力集中。FNS组的应力主要集中在支撑棒与拉力螺钉的上下表面,表明该区域的应力承受较为集中,应力峰值为222.25 MPa,相较于空心钉组明显升高,但从应力分布云图中分析,其整体的应力分布较空心钉组均匀,且能够更好地将应力向远端传导。联合组从云图整体上分析,这种应力分布方式在3组模型中最为均匀,主要集中在2枚交叉钉与空心钉的上下表面,应力峰值为201.10 MPa,相比于FNS组也更低,显示出最好的应力分散和承载效果。见图6及表2。"
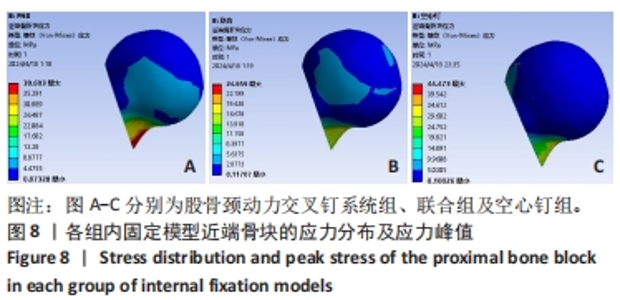
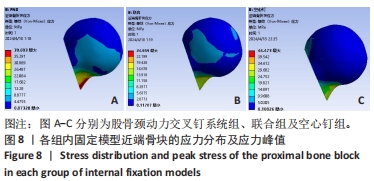
2.5 近端骨块的应力分布及应力峰值 在评估3组不同的内固定装置模型对近端骨块应力的影响时,观察到以下应力分布和峰值特点:3组模型的近端骨块应力主要集中在骨折断端,特别是在骨折端靠下方的区域,这表明这些区域在力学传递过程中承受了较大的应力和应变。空心钉组的应力峰值达到了44.473 MPa,是3组中最高的,这表明在空心钉组的内固定方式下,近端骨块在骨折端下方区域的应力集中现象最为明显。FNS组的应力峰值相对较低,为39.693 MPa,这一结果说明FNS组在减少应力集中、优化应力分布方面表现出较空心钉组更好的性能。联合组的应力峰值为24.959 MPa,应力峰值最低,且从云图上看,其近端骨块的应力分布也更均匀合理。综上所述,虽然3组模型在近端骨块的应力分布上表现出相似的特点,但应力峰值的大小和分布却存在明显差异。见图8及表2。"
| [1] 葛双雷, 王雪飞, 刘亮, 等. 股骨颈动力交叉钉系统联合支撑空心钉对伴后内侧粉碎的中青年股骨颈骨折的疗效研究[J].中华医学杂志,2023,103(21):1631-1637. [2] 张英泽. 临床创伤骨科流行病学[M]. 3版. 北京: 人民卫生出版社, 2018:223-225. [3] RAUDENBUSH B, WALTON I, SIMELA A, et al. Inflammatory bowel disease, high-dose steroids, osteoporosis, or an oncological etiology for a pathological femoral neck fracture in a young adult: a case report. Open Orthop J. 2014;8:27-33. [4] FORTINA M, CARTA S, CRAINZ E, et al. Management of displaced intracapsulatfemoral neck fracture in young adult:why complications are still so high? Casereport of posttraumatic avascular necrosis in a 30-year-old man and a briefreview. J Trauma. 2009;67(5):E163-E166. [5] LIU BC, SUN C, XING Y, et al. Analysis ofrisk factors for necrosis of femoral headafter internal fixation surgery in young and mid-aged patients with femoral neckfracture. Beijing Da Xue Xue Bao Yi Xue Ban. 2020;52(2):290-297. [6] LIPORACE F, GAINES R, COLLINGE C, et al. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90:1654-1659. [7] MARSH JL, SLONGO TF, AGEL J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1-133. [8] KUNAPULI SC, SCHRAMSKI MJ, LEE AS, et al. Biomechanical analysis of augmented plate fixation for the treatment of vertical shear femoral neck fractures. J Orthop Trauma. 2015;29:144-150. [9] LI M, COLE PA. Anatomical considerations in adult femoral neck fractures: how anatomy influences the treatment issues? Injury. 2015; 46(3):453-458. [10] LIPORACE F, GAINES R, COLLINGE C, et al. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90(8):1654-1659. [11] JIAN-QIAO PENG M, CHEN HY, JU X, et al. CoMParative analysis for five fixations of Pauwels-I by the biomechanical finite-element method. J Invest Surg. 2020;33(5):428-437. [12] FLORSCHUTZ AV, LANGFORD JR, HAIDUKEWYCH GJ, et al. Femoral neck fractures:current management. J Orthop Trauma. 2015;29(3):121 -129. [13] WANG G, TANG Y, WU X, et al. Finite element analysis of a new plate for Pauwels type Ⅲ femoral neck fractures. J Int Med Res. 2020;48(2): 1220703221. [14] STOFFEL K, ZDERIC I, GRAS F, et al. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A CoMParison with the Dynamic Hip Screw and Cannulated Screws. J Orthop Trauma. 2017;31(3):131-137. [15] JUNG CH, CHA Y, YOON HS, et al. Mechanical effects of surgical variations in the femoral neck system on Pauwels type III femoral neck fracture : a finite element analysis. Bone Joint Res. 2022;11(2):102-111. [16] 葛双雷, 王雪飞, 刘亮, 等. 股骨颈动力交叉钉系统联合支撑空心钉对伴后内侧粉碎的中青年股骨颈骨折的疗效研究[J].中华医学杂志,2023,103(21):1631-1637. [17] ZHENG S, LIN D, CHEN P, et al. CoMParison of femoral neck shortening after femoral neck system and cannulated cancellous screw fixation for displaced femoral neck fractures in young adults. Injury. 2024;55(6):111564. [18] WANG SH, YANG JJ, SHEN HC, et al. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury. 2015;46(10):1969-1974. [19] LI J, WANG M, LI L, et al. Finite element analysis of different configurations of fully threaded cannulated screw in the treatment of unstable femoral neck fractures. J Orthop Surg Res. 2018;13(1):272. [20] GARDNER MP, CHONG AC, POLLOCK AG, et al. Mechanical evaluation of large-size fourth-generation composite femur and tibia models. Ann Biomed Eng, 2010;38(3):613-620. [21] HEINER AD. Structural properties of fourth-generation composite femurs and tibias. J Biomech. 2008;41(15):3282-3284. [22] MA L, ZHOU Y, ZHANG Y, et al. Biomechanical evaluation with finite element analysis of the reconstruction of femoral tumor defects by using a double-barrel free vascularized fibular graft combined with a locking plate. Int J Clin Exp Med. 2014;7(9):2425-2434. [23] ZHENG L, CHEN X, ZHENG Y, et al. Cement augmentation of the proximal femoral nail antirotation for the treatment of two intertrochanteric fractures - a coMParative finite element study. BMC Musculoskelet Disord. 2021;22(1):1010. [24] VAN HOUCKE J, SCHOUTEN A, STEENACKERS G, et al. Computer-basedestimation of the hip joint reaction force and hip flexion angle in three different sitting configurations. Appl Ergon. 2017;63:99-105. [25] JACOB G, PAI S, HUGGI V, et al. Lag screw with DHS (LSD) for vertical angle femoral neck fractures in young adults. Injury. 2020;51(11): 2628-2633. [26] WANG K, LIN D, CHEN P, et al. Incidence and factors influencing neck shortening after screw fixation of femoral neck fractures with the femoral neck system. J Orthop Surg Res. 2023;18(1):317. [27] 徐高伟,陈廷,张松,等.55-65 岁 Garden Ⅲ、W型股骨颈骨折患者手术方式选择及疗效的比较[J].中华解剖与临床杂志,2020, 25(4):388-392. [28] 张长青,张英泽,余斌,等.成人股骨颈骨折诊治指南[J].中华创伤骨科杂志,2018,20(11):921-928. [29] LIPORACE F, GAINES R, COLLINGE C, et al. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone joint Surg Am. 2008;90:1654-1659. [30] SLOBOGEAN GP, SPRAGUE SA, SCOTT T, et al. Complications following young femoral neck fractures. Injury. 2015;46:484-491. [31] DUCKWORTH AD, BENNET SJ, ADERINTO J, et al. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone joint Surg Br. 2011;93:811-816. [32] WANG Y, MA JX, BAI HH, et al. Mechanical analysis of the femoral neck dynamic intersection system with different nail angles and clinical applications. World J Clin Cases. 2023;11(20):4814-4823. [33] TENG Y, ZHANG Y, GUO C. Finite element analysis of femoral neck system in the treatment of Pauwels type III femoral neck fracture. Medicine. 2022;101(28):e29450. [34] WANG K, LIN D, CHEN P, et al. Incidence and factors influencingneck shortening after screw fixation of femoral neck fractures with thefemoral neck system. J Orthop Surg Res. 2023;18(1):317. [35] LU Y, CANAVESE F, NAN G, et al. Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A CoMParative Study of Femoral Neck System versus Cannulated Compression Screw. Medicina (Kaunas). 2022;58(8):999. [36] ZHANG YZ, LIN Y, LI C, et al. A CoMParative Analysis of Femoral Neck System and Three Cannulated Screws Fixation in the Treatment of Femoral Neck Fractures: A Six-Month Follow-Up. Orthop Surg. 2022; 14(4):686-693. [37] NIBE Y, MATSUMURA T, TAKAHASHI T, et al. A coMParison between the femoral neck system and other implants for elderly patients with femoral neck fracture: A preliminary report of a newly developed implant. J Orthop Sci. 2022;27(4):876-880. [38] SAAD A, PATRALEKH MK, JAIN VK, et al. Femoral neck system reduces surgical time and complications in adults with femoral neck fractures: A systematic review and meta-analysis. J Clin Orthop Trauma. 2022; 30:101917. [39] 杨家赵,周雪锋,朱万博,等.FNS与空心钉固定治疗青壮年股骨颈骨折的近期疗效比较[J].中华创伤骨科杂志,2021,23(9):761-768. [40] 许翔宇,周方,田耘,等.FNS与DHS固定治疗股骨颈骨折的早期疗效比较[J].中华创伤骨科杂志,2021,23(9):754-760. [41] FELTON J, SLOBOGEAN GP, JACKSON SS, et al. Femoral neck shorteningafter hip fracture fixation is associated with inferior hip function: results from the FAITH trial. J Orthop Trauma. 2019;33(10): 487-496. [42] 李正刚,尚学红,吴张,等.不同载荷条件下三种内固定方式治疗PauwelsⅢ型股骨颈骨折的有限元分析[J].中国组织工程研究, 2025,29(3):455-463. [43] 荆玉龙,张树栋,韩紫音,等.骨科机器人辅助股骨颈动力交叉钉系统治疗新鲜股骨颈骨折的近期疗效[J].中国修复重建外科杂志, 2022,36(8):946-950. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904. |
| [3] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [4] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [5] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [6] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [7] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [8] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [9] | Li Shuai, Liu Hua, Shang Yonghui, Liu Yicong, Zhao Qihang, Liu Wen. Stress distribution on the maxilla when wearing the Twin-block appliance for Class II malocclusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 881-887. |
| [10] | Zhou Zonghao, Luo Siyang, Chen Jiawen, Chen Guangneng, Feng Hongchao. Finite element analysis of bioabsorbable plates versus miniature titanium plates in mandibular fracture fixation in different bone qualities [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 818-826. |
| [11] | Chen Yilong, Zhang Xu, Li Hong. Mechanical analysis of fiber post combined with different crown restorations for endodontically treated non-carious cervical lesions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 866-871. |
| [12] | Song Xubin, Wu Dou, Zhao Enzhe, Zhang Xingyu, Zhang Xiaolun, Wang Chuheng. Finite element analysis of a new femoral neck spiral blade system to treat femoral intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7041-7047. |
| [13] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| [14] | Xu Xin, Wurikaixi·Aiyiti, Lyu Gang, Maimaiaili·Yushan, Ma Zhiqiang, Ma Chao. Finite element analysis of four different internal fixation methods for complex acetabular double-column fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7063-7071. |
| [15] | Liang Cheng, Zhuo Chuanchuan, Zhang Xiaogang, Wang Guan, Duan Ke, Li Zhong, Lu Xiaobo, Zhuo Naiqiang, Jin Zhongmin. Biomechanical characteristics of a novel sacroiliac lag screw [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7080-7086. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||