Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1775-1782.doi: 10.12307/2025.144
Previous Articles Next Articles
Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths
Zhou Jinhai1, Li Jiangwei2, Wang Xuquan1, Zhuang Ying1, Zhao Ying1, Yang Yuyong1, Wang Jiajia1, Yang Yang1, Zhou Shilian1
- 1Department of Orthopedics, Guiqian International Hospital, Guiyang 550024, Guizhou Province, China; 2Department of Orthopedics, Affiliated Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China
-
Received:2023-12-19Accepted:2024-02-29Online:2025-03-28Published:2024-10-09 -
Contact:Li Jiangwei, Chief physician, Department of Orthopedics, Affiliated Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
About author:Zhou Jinhai, Master, Attending physician, Department of Orthopedics, Guiqian International Hospital, Guiyang 550024, Guizhou Province, China -
Supported by:Guizhou Provincial Health Commission Science Fund Project, No. gzwkj2021-507 (to ZY)
CLC Number:
Cite this article
Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

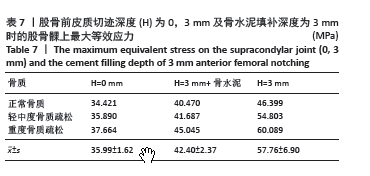
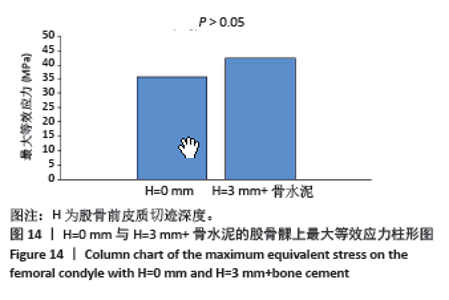
2.3.1 AFN深度为0 mm和3 mm的比较 如图12所示,从表7中可看出,正常没有AFN组和AFN深度为3 mm组股骨髁上最大等效应力分别为(35.99±1.62)及(57.76±6.90) MPa,差异近12 MPa,差异有显著性意义(P=0.02 < 0.05)。 2.3.2 AFN深度为3 mm和采用骨水泥填充AFN比较 如图13所示,AFN深度为3 mm+骨水泥、AFN深度为3 mm时股骨髁上最大等效应力分别为(42.40±2.37) MPa及(57.76±6.90) MPa,用骨水泥填补AFN后髁上最大等效应力降低,差异有显著性意义(P=0.018 < 0.05)。 2.3.3 正常没有AFN和AFN深度为3 mm+骨水泥的比较 如图14所示,没有AFN组和骨水泥填补3 mm深度AFN组的股骨髁最大等效应力分别为(35.99±1.62) MPa和(42.40±2.37) MPa,相差不到7 MPa,在3组数据的单因素方差分析的多重比较中,两个样本差异无显著性意义(P=0.119 > 0.05)。"

| [1] WANG JC, PIPLE AS,HILL WJ, et al. Computer-Navigated and Robotic-Assisted Total Knee Arthroplasty: Increasing in Popularity Without Increasing Complications. J Arthroplasty. 2022;37(12):2358-2364. [2] LOMBARDO DJ, SILJANDER MP, SOBH A, et al. Periprosthetic fractures about total knee arthroplasty. Musculoskelet Surg. 2020;104(2):135-143. [3] CARON É, GABRION A, EHLINGER M, et al. French society of orthopedic surgery and traumatology (SOFCOT); Complications and failures of non-tumoral hinged total knee arthroplasty in primary and aseptic revision surgery: A review of 290 cases. Orthop Traumatol Surge Res. 2021;107(3):102875. [4] MA LL, YU XR, WENG XS, et al. Possible Risk Factors for Severe Complications Occurring after Primary Total Knee Arthroplasty. Chin Med Sci J. 2022;37(4):303-308. [5] DELSMANN MM, SCHMIDT C, MÜHLENFELD M, et al. Prevalence of osteoporosis and osteopenia in elderly patients scheduled for total knee arthroplasty. Arch Orthop Trauma Surg. 2022;142(12):3957-3964. [6] SKIBICKI HE, PONZIO DY, BRUSTEIN JA, et al. A cautionary case: osteoporotic femur fracture after robotic-assisted total knee arthroplasty. Osteoporos Int . 2021;32(10):2125-2129. [7] STAMIRIS D, GKEKAS NK, ASTERIADIS K, et al. Anterior femoral notching ≥ 3 mm is associated with increased risk for supracondylar periprosthetic femoral fracture after total knee arthroplasty: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2022;32(3):383-393. [8] ZHANG JC, ZHANG LS, ZHOU H, et al. Stress distribution patterns during the gait cycle in patients with anterior femoral notching following total knee replacement. BMC Musculoskelet Disord. 2022;23(1):718. [9] CHATURONG P, AKRAPORN S, PAKPOOM R, et al. Risk factors of early periprosthetic femoral fracture after total knee arthroplasty. BMC Musculoskelet Disord. 2021;22(1):1009. [10] PURANIK HG, MUKARTIHAL R, PATIL SS, et al. Does Femoral Notching During Total Knee Arthroplasty Influence Periprosthetic Fracture. A Prospective Study. J Arthroplasty. 2019;34(6):1244-1249. [11] WANG DG, LI Y, YIN HL, et al. Three-dimensional finite element analysis of optimal distribution model of vertebroplasty. Ann Palliat Med. 2020; 9(3):1062-1072. [12] XIE XJ, CAO SL, TONG K, et al. Three-dimensional finite element analysis with different internal fixation methods through the anterior approach. World J Clin Cases. 2021;9(8):1814-1826. [13] 李志帅,张红倩,李丽,等.有膝关节有限元分析的研究热点及趋势[J].中国组织工程研究,2022,26(15):2412-2418. [14] FALCINELLI C, WHYNE C. Image-based finite-element modeling of the human femur. Comput Methods Biomech Biomed Engin. 2020;23(14): 1138-1161. [15] KANAIZUMI A, SUZUKI D, NAGOYA S, et al. Patient-specific three-dimensional evaluation of interface micromotion in two different short stem designs in cementless total hip arthroplasty: a finite element analysis. J Orthop Surg Res. 2022;17(1):437. [16] 熊恒恒,聂伟志.三维有限元分析对骨关节和相关软组织损伤时应力状态的精准模拟[J].中国组织工程研究,2022,26(36):5875-5880. [17] RHO JY, HOBATHO MC, ASHMAN RB. Relations of mechanical properties to density and CT numbers in human bone. Med Eng Phys. 1995;17(5): 347-355. [18] HOU YJ. Investigation in the dependency of stiffness of cancellous bone on apparent density—based on the combination model of rod-rod structure and perforated plate structure. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. 2006;23(1):78-81. [19] JETHANANDANI R, PATWARY MB, SHELLITO AD, et al. Biomechanical consequences of anterior femoral notching in cruciate-retaining versus posterior-stabilized total knee arthroplasty. Am J Orthop. 2016; 45(5):E268. [20] WIJAYATHUNGA VN, JONES AC, OAKLAND RJ, et al. Development of specimen-specific finite element models of human vertebrae for the analysis of vertebroplasty. Proc Inst Mech Eng H. 2008;222(2):221-228. [21] COMPLETO A1, SIMÕES JA, FONSECA F. Revision total knee arthroplasty: The influence of femoral stems in load sharing and stability. Knee. 2009; 16(4):275-279. [22] WU WD, HAN ZH, HU BI, et al. A graphical guide for constructing a finite element model of the cervical spine with digital orthopedic software. Ann Transl Med. 2021;9(2):169. [23] KAZEMI M, DABIRI Y, LI LP. Recent advances in computational mechanics of the human knee joint.Computational and mathematical methods in medicine. 2013;2013:718423. [24] KIM JG, KANG KT, WANG JW. Biomechanical Difference between Conventional Transtibial Single-Bundle and Anatomical Transportal Double-Bundle Anterior Cruciate Ligament Reconstruction Using Three-Dimensional Finite Element Model Analysis. J Clin Med. 2021; 10(8):1625. [25] MEHBOOB H, TARLOCHAN F, MEHBOOB A, et al. Finite element modelling and characterization of 3D cellular microstructures for the design of a cementless biomimetic porous hip stem. Mater Design. 2018;149: 101-112. [26] ACEVEDO C, SYLVIA M, SCHAIBLE E, et al. Contributions of material properties and structure to increased bone fragility for a given bone mass in the UCD‐T2DM rat model of type 2 diabetes. J Bone Miner Res. 2018;33(6):1066-1075. [27] GAUTAM A, CALLEJAS MA, ACHARYYA A, et al. Shape-memory-alloy-based smart knee spacer for total knee arthroplasty: 3D CAD modelling and a computational study. Med Eng Phys. 2018;55:43-51. [28] LI Y, GAO YH, LU D, et al. Analysis of the effect of tibial torsion on tibial osteotomy in knee arthroplasty using a three-dimensional computed tomography-based modelling technique. BMC Musculoskelet Disord . 2019;20(1):361. [29] PHILIPPE M, SARA C, INES K, et al. Physiological joint line total knee arthroplasty designs are especially sensitive to rotational placement – A finite element analysis. Plos One. 2018;13(2):e0192225. [30] JEFFREY NK, KAETLYN RA, RICHARD FL. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA. 2021;325(6):568-578. [31] BRYAN SB, JEREMIAH JM, SAMUEL FT, et al. Complication Rates in Total Knee Arthroplasty Performed for Osteoarthritis and Post-Traumatic Arthritis: A Comparison Study. J Arthroplasty. 2020;35(2):371-374. [32] ZALZAL P, BACKSTEIN D, GROSS AE, et al. Notching of the anterior femoral cortex during total knee arthroplasty characteristics that increase local stresses. J Arthroplasty. 2006;21:737-743. [33] CULP RW, SCHMIDT RG, HANKS G, et al. Supracondylar fracture of the femur following prosthetic knee arthroplasty. Clin Orthop Relat Res. 1987;(222):212-222. [34] HOENIG T, KATHRYN EA, BELINDA RB, et al. Bone stress injuries. Nature reviews. Dis Primers. 2022;8(1):26. [35] CEN HP, JIA YM, WU XG, et al. Effects of the microcrack’s shape, size and direction on the poroelasticbehaviors of a single osteon: a finite element study. Acta Bioeng Biomech. 2016;18(1):3-10. [36] STOCKLEY I, MCAULEY JP, GROSS AE. Allograft reconstruction in total knee arthroplasty. Bone Joint J. 1992;74(3):393-397. [37] RAND JA. Bone deficiency in total knee arthroplasty. Use of metal wedge augmentation. Clin Orthop Relat Res. 1991;271(271):63. [38] RÖHNER E, HEINECKE M, MATZIOLIS G. Bone defect management in revision knee arthroplasty. Der Orthopade. 2021;50(12):1004-1010. [39] AGGARWAL AK, BABURAJ V. Managing bone defects in primary total knee arthroplasty: options and current trends. Musculoskelet Surg. 2021;105(1):31-38. [40] ZOHRE Z, MAJEDEH N, MAJID N, et al. Effect of Cement Type and Cementation Technique on the Retention of Implant-Supported Restorations. J Long Term Eff Med Implants. 2020;30(1):61-67. [41] AJAY K, RAJESH G. Fracture Toughness of Acrylic PMMA Bone Cement: A Mini-Review. Indian J Orthop. 2021;55(5):1208-1214. |
| [1] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [2] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [3] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [4] | Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904. |
| [5] | Zhao Jiyu, Wang Shaowei. Forkhead box transcription factor O1 signaling pathway in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1923-1930. |
| [6] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [7] | Zhao Jiacheng, Ren Shiqi, Zhu Qin, Liu Jiajia, Zhu Xiang, Yang Yang. Bioinformatics analysis of potential biomarkers for primary osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1741-1750. |
| [8] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [9] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [10] | Li Yueyao, Zhang Min, Yang Jiaju. Cistanoside A mediates p38/MAPK pathway to inhibit osteoclast activity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1144-1151. |
| [11] | Zheng Lin, Jin Wenjun, Luo Shanshan, Huang Rui, Wang Jie, Cheng Yuting, An Zheqing, Xiong Yue, Gong Zipeng, Liao Jian. Eucommia ulmoides promotes alveolar bone formation in ovariectomized rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1159-1167. |
| [12] |
Huang Xiaobin, Ge Jirong, Li Shengqiang, Xie Lihua, Huang Jingwen, He Yanyan, Xue Lipeng.
Mechanisms of different yin nourishing and kidney tonifying methods on osteoclastysis pathway in ovariectomized rats #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1214-1219.
|
| [13] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [14] | Lan Shuangli, Xiang Feifan, Deng Guanghui, Xiao Yukun, Yang Yunkang, Liang Jie. Naringin inhibits iron deposition and cell apoptosis in bone tissue of osteoporotic rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 888-898. |
| [15] | Wang Dongyang, Yang Qiaohui, Lin Xinchao. Relationship between vitamin D levels and reproductive characteristics and exercise dietary situation in postmenopausal women [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1021-1025. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||