Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (19): 4091-4101.doi: 10.12307/2025.068
Previous Articles Next Articles
Endothelial progenitor cell and mesenchymal stem cell therapy for vascular stent-associated diseases
Li Qingyin1, 2, Li Linhua1, Zhang Chunle1, Fu Ping1
- 1Kidney Research Institute, Department of Nephrology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China; 2Frontier Science Center for Disease-related Molecular Network, Sichuan University, Chengdu 610041, Sichuan Province, China
-
Received:2024-02-23Accepted:2024-04-29Online:2025-07-08Published:2024-09-13 -
Contact:Fu Ping, PhD, Professor, Chief physician, Kidney Research Institute, Department of Nephrology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China -
About author:Li Qingyin, Master candidate, Kidney Research Institute, Department of Nephrology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China; Frontier Science Center for Disease-related Molecular Network, Sichuan University, Chengdu 610041, Sichuan Province, China
CLC Number:
Cite this article
Li Qingyin, Li Linhua, Zhang Chunle, Fu Ping. Endothelial progenitor cell and mesenchymal stem cell therapy for vascular stent-associated diseases[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(19): 4091-4101.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
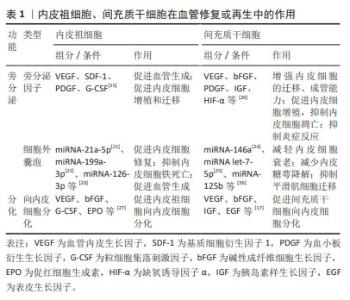
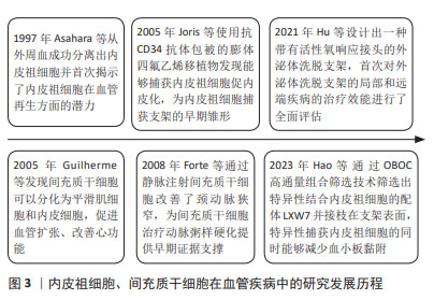
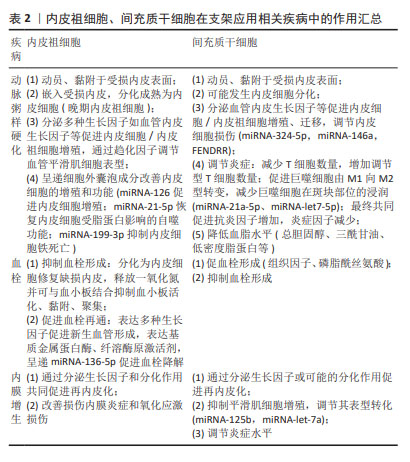
2.2 内皮祖细胞、间充质干细胞在血管支架相关疾病中的治疗作用 2.2.1 内皮祖细胞、间充质干细胞在血管修复或再生中的作用 (1)内皮祖细胞:内皮祖细胞可分为早期内皮祖细胞以及晚期内皮祖细胞[12],它们在血管内皮修复中发挥着至关重要的作用。不论早期还是晚期内皮祖细胞均具有分泌多种细胞因子、生长因子的能力[13],这些旁分泌因子能够促进血管生成、内皮细胞的增殖和迁移,此外内皮祖细胞分泌的细胞外囊泡通过细胞间通讯共同参与旁分泌调节[14]。其中分化程度较低即早期内皮祖细胞主要通过旁分泌作用促进内皮细胞增殖以及晚期内皮祖细胞分化,分化程度较高即晚期内皮祖细胞主要通过黏附、嵌入受损的血管内皮、增殖、分化取代受损内皮细胞,为血管内皮修复提供健康、成熟的细胞原料[15]。 (2)间充质干细胞:血管内皮受损后局部分泌异常水平的细胞、趋化因子能够募集间充质干细胞到损伤部位,分泌多种细胞因子以及细胞外囊泡促进血管内皮再生修复。较多研究认为其重要的功能是炎症调节,可以通过调节T细胞、自然杀伤细胞和巨噬细胞抑制炎症反应[16]。除了旁分泌作用,与内皮祖细胞一样,间充质干细胞具有分化为内皮细胞的能力,它可以在多种因子、缺氧以及剪切应力等条件下分化为内皮细胞[12,17-18],其中血管内皮生长因子和碱性成纤维细胞生长因子诱导间充质干细胞的内皮细胞分化效果较好[19]。除了分化为内皮细胞外,在转化生长因子β1、微小RNA(miRNA-503、miRNA-222-5p)等条件下间充质干细胞还会分化为血管平滑肌细胞[12]。 具体的旁分泌因子、细胞外囊泡功能成分及效能见表1。"
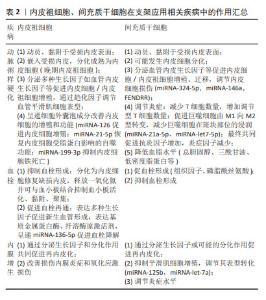
2.2.2 内皮祖细胞、间充质干细胞治疗动脉粥样硬化 (1)动脉粥样硬化发病机制:内皮细胞功能障碍、血管内皮屏障结构完整性破坏与内皮细胞修复的平衡被打破是动脉粥样硬化发生、发展的关键要素[28]。易发生动脉粥样硬化人群的血管内皮细胞可能受到低密度脂蛋白、高血压、高血糖、促炎因子如肿瘤坏死因子α等影响,在这些因素的作用下内皮细胞功能发生非适应性改变:表达的内皮一氧化氮合酶解偶联,产生一氧化氮能力下降;核因子κB通路被激活进而表达一系列效应蛋白激活炎症细胞、平滑肌细胞、血小板,即内皮细胞出现功能异常[29]。除了功能异常,在炎症与氧化应激的微环境下,参与构成内皮屏障的内皮细胞表面糖萼以及细胞间连接常会被打破,导致血管内皮通透性增加[30],此时被募集的炎症细胞更加容易通过内皮细胞间隙浸润在血管内皮下层,被活化的血小板黏附、聚集,促进单核细胞或巨噬细胞表达多种炎症因子进一步促进炎症发展[31]。浸润于血管内皮下层的单核细胞部分转化为巨噬细胞,而后吞噬大量氧化性低密度脂蛋白,与细胞外脂质共同构成脂质核心,这一脂质核心被发生表型转化、增殖、迁移的平滑肌细胞及其分泌的细胞外基质等成分包裹,与功能异常的内皮细胞共同构成动脉粥样硬化斑块[32-33]。血管内皮细胞自我修复通常以循环或损伤周围常驻的健康内皮细胞为主,以干细胞或其他一些细胞如平滑肌细胞修复为辅。受损的内皮细胞通过激活Notch1信号通路,上调Dlk1表达miRNA-126-5p以分泌更多的促血管生长、迁移因子,促进健康的内皮细胞聚集在损伤部位并增殖;内皮细胞还会通过表达N-钙黏蛋白等修复细胞间连接。干细胞则通过旁分泌多种血管生长、迁移因子或细胞外囊泡调节内皮细胞代谢与增殖,这一旁分泌作用的调节与晚期内皮祖细胞的内皮细胞分化作用共同促进损伤内皮细胞的修复再生[34],当内皮细胞损伤与修复平衡被打破时,血管发生动脉粥样硬化的风险随之升高,若修复始终处于异常状态则会进一步促进动脉粥样硬化的进展。 (2)内皮祖细胞治疗动脉粥样硬化的作用机制:内皮祖细胞参与血管内皮修复主要包括动员、归巢、增殖、分化、旁分泌等过程。损伤部位分泌的高水平血管内皮生长因子、粒细胞集落刺激因子、粒细胞-巨噬细胞集落刺激因子、基质细胞衍生因子1α等促进着内皮祖细胞的募集、黏附[35-36],WEI等[37]使用超小型超顺磁性氧化铁纳米颗粒标记内皮祖细胞,MRI示踪证实了内皮祖细胞在动脉粥样硬化部位聚集。如前所述晚期内皮祖细胞可以通过增殖、分化替代受损的内皮细胞[38],除了分化作用,内皮祖细胞能够通过呈递细胞外囊泡成分miRNA-126以及多种生长因子促进内皮细胞增殖再生,miRNA-21-5p成分够逆转氧化型低密度脂蛋白诱导的内皮细胞活性下降和自噬功能障碍[39],从而保护内皮细胞受到脂蛋白累积的损害,miRNA-199a-3p可抑制内皮细胞铁死亡并减轻动脉粥样硬化发生[22]。除了对内皮细胞的功能有调节作用,内皮祖细胞还可能对平滑肌细胞的表型转化具有调节作用,有研究将内皮祖细胞和平滑肌细胞共同培养,发现在脂蛋白累积的状态下,内皮祖细胞通过趋化因子CXCL12-CXCR4途径阻碍了平滑肌由收缩表型向合成表型转化,减少了平滑肌细胞分泌释放促炎因子,从而阻碍了动脉粥样硬化的进展[40]。有研究发现内皮祖细胞分泌的细胞外囊泡显著减少糖尿病并发动脉粥样硬化小鼠模型血管斑块数量,降低了细胞黏附分子1、白细胞介素8、C-反应蛋白以及氧化应激因子丙二醛和超氧化物歧化酶水平[21]。 (3)间充质干细胞治疗动脉粥样硬化的作用机制:目前研究证据表明间充质干细胞主要通过4个方面的作用改善动脉粥样硬化:①调节炎症:通过减少T细胞数量、降低血清单核细胞趋化蛋白1水平,促进调节性T细胞的发育和增殖[41-42],通过激活STAT6信号通路等诱导巨噬细胞转变为M2抗炎表型,通过细胞外囊泡成分miRNA-21a-5p[43]、miRNA-let7-5p抑制动脉粥样硬化斑块中巨噬细胞的浸润并减少巨噬细胞凋亡[25,44],最终减少血管炎症反应,炎症因子如肿瘤坏死因子α、白细胞介素6的表达降低,而抗炎因子白细胞介素10和转化生长因子β的表达增高;②保护内皮细胞,促进内皮细胞增殖并向内皮细胞分化,调节内皮祖细胞功能:通过细胞外囊泡成分miRNA-324-5p、miRNA-146a[24]、miRNA-145等抑制内皮功能障碍[45],通过细胞外囊泡成分FENDRR调节miRNA-28水平逆转内皮细胞损伤[46],抑制斑块炎症,减少内皮细胞凋亡;通过分化为内皮细胞以及促进内皮细胞、内皮祖细胞增殖迁移功能共同促进血管内皮细胞修复[47-49],但研究表明体内非给药条件下单纯向内皮细胞分化的间充质干细胞比例较少,约占8%[50];③降低血脂如总胆固醇、三酰甘油、低密度脂蛋白水平[51];④调节血管平滑肌细胞增殖:有研究认为间充质干细胞能够抑制血管平滑肌增殖[48],在炎症调节过程中生成的转化生长因子β1等是间充质干细胞向平滑肌细胞分化的重要调节因子,在一些研究中间充质干细胞被认为通过分化为平滑肌细胞稳定斑块,减少斑块破裂引起的血栓等问题[52]。由于该方面的报道较少,不同间充质干细胞的培养条件和应用状态的不同是否会导致与④观点的不同尚不可知,未来需要进一步探究。 2.2.3 内皮祖细胞、间充质干细胞治疗血管支架植入损伤 血栓和内膜增生是导致支架植入后患者远期预后较差的两大原因[53]。血管损伤后内膜增生与动脉粥样硬化发病机制有着相似的本质,支架植入损伤内皮后,部分内皮细胞脱落,暴露出基底面胶原,血小板激活、黏附、聚集并发生级联反应,此时可能导致急性血栓形成,而后中性粒细胞与巨噬细胞等炎症细胞聚集在损伤部位,血管平滑肌细胞由收缩型转变为分泌型并发生增殖,随着基质金属蛋白酶等对细胞外基质降解而向内膜下层迁移,最后细胞外基质重新合成与增殖迁移到内膜下的血管平滑肌细胞共同构成新生内膜[54-55],而晚期支架血栓形成主要是由支架植入后内皮化延迟导致。下面将从内皮祖细胞、间充质干细胞在血栓和内膜增生中的作用展开讨论二者在血管支架植入损伤中的治疗效能。 (1)血栓 内皮祖细胞抑制血栓形成并促进血栓再通:已有较多研究发现内皮祖细胞不仅能够抑制血栓形成,还能够促进血栓再通。血管内皮损伤后激活的血小板能够释放多种旁分泌因子(如基质细胞衍生因子1)并表达细胞表面黏附分子P-选择素[56],促进内皮祖细胞的募集和分化,内皮祖细胞具有健康内皮细胞维持血管正常生理状态下的许多重要功能,内皮祖细胞募集到损伤部位可能通过抑制血小板活性来抑制急性血栓形成,并促进再内皮化和血管修复[57]。目前内皮祖细胞对血栓的形成抑制以及再通作用机制主要包括以下5点:①内皮祖细胞能通过修复受损内皮细胞或分化补充丢失的内皮细胞以修复导致血栓形成的根源问题——内皮细胞受损导致的内皮屏障破坏基底胶原暴露;②内皮祖细胞分泌的多种生长因子(血管内皮生长因子、肝细胞生长因子、转化生长因子β等)能够诱导血栓中的新生血管形成以改善血栓中的血供状态[58],这与内皮细胞、巨噬细胞对血栓纤维蛋白网降解形成隧道后内皮祖细胞在局部分化、覆盖形成内皮表面的论点相互印证[59];③内皮祖细胞能够通过释放一氧化氮或通过与血小板结合抑制血小板活化、黏附与聚集[57,60];④内皮祖细胞释放的基质金属蛋白酶、纤溶酶原激活剂能够激活纤溶酶原,促进血栓成分的分解[60];⑤分泌的细胞外囊泡成分如miRNA-136-5p通过抑制硫氧还蛋白互作蛋白表达促进血栓溶解[61]。 间充质干细胞与血栓:在抗血栓方面,间充质干细胞并没有表现出相应的优势,目前主流研究认为间充质干细胞具有促凝血作用,已有较多研究发现使用间充质干细胞会引发凝血和补体途径的双重激活,发生即刻经血液介导的炎症反应(IBMIR)[62]。间充质干细胞通过多种途径调节凝血过程:间充质干细胞分泌的组织因子启动凝血,促进血小板的产生和活化,其分泌的细胞外囊泡中包含的磷脂酰丝氨酸会激活凝血级联反应[63]。但有少量文献研究认为间充质干细胞具有抗凝作用:NETSCH等[64]发表文章指出,不同来源(骨髓、脂肪和脐血)的间充质干细胞具有抗凝血特性,它们能够抑制全血中血小板的活化和聚集。一些学者认为间充质干细胞及其细胞外囊泡均同时具有抗凝血和促凝血的特性,其表达较高水平的促凝血分子的同时表达低水平的抗凝分子,因而也主要表现出促凝的特 点[65],这一观点解释了不同研究中间充质干细胞促凝和抗凝作用的矛盾结果,目前大量人类或动物研究报道的血栓形成事件也证实了间充质干细胞以促凝血为主的特性[66]。 (2)内膜增生 内皮祖细胞抑制内膜增生:研究认为内皮祖细胞可能通过旁分泌细胞因子(如血管内皮生长因子、转化生长因子β1、胰岛素样生长因子1)或增殖分化促进再内皮化而改善支架植入后再狭窄的问题。SUN等[67]将分离出的内皮祖细胞注射至动物模型中,发现实验组血管内皮生长因子和内皮型一氧化氮合酶表达显著升高,炎症调节和脂质过氧化物表达显著低于对照组,即改善了内膜炎症,减少了氧化应激,减轻了内皮功能障碍;WANG等[68]以及XU等[69]通过建立大鼠颈动脉球囊损伤模型证实了内皮祖细胞能够抑制球囊损伤后的内膜增生。内皮祖细胞外泌体也被证实可能通过修复内皮细胞,减慢平滑肌细胞增殖来抑制内膜增生[70]。 间充质干细胞抑制内膜增生:现已有多个研究发现不同来源(脐血、骨髓、脂肪等)的间充质干细胞能够抑制内膜增生,它们可能通过抗炎[71]、促内皮化以及抑制平滑肌细胞增殖周期和炎症表型转化等作用抑制血管内皮损伤后的内膜增生[72-73]。CAI等[74]发现脂肪来源间充质干细胞降低了球囊损伤后血管促炎基因的表达,减少了动静脉瘘球囊治疗术后的内膜增生,改善了血管重塑过程。间充质干细胞外泌体能够介导内皮细胞的血管内皮生长因子表达[75-76],促进内皮细胞增殖、迁移[77],从而加速内皮化进程;其细胞外囊泡组分miRNA-125b[26]、miRNA-let-7a能够下调α-平滑肌肌动蛋白表达抑制平滑肌细胞增殖[78],共同抑制血管内皮损伤后的内膜增生[79]。有部分研究发现损伤后血管内激活的转化生长因子β1/Smad信号转导通路诱导了骨髓间充质干细胞向损伤部位聚集、分化并促进内膜增生[80],间充质干细胞对内膜增生的抑制和促进作用之间是如何相互平衡的,是未来研究值得探索的一个问题。 内皮祖细胞、间充质干细胞在支架应用相关疾病中的机制总结见表2。"
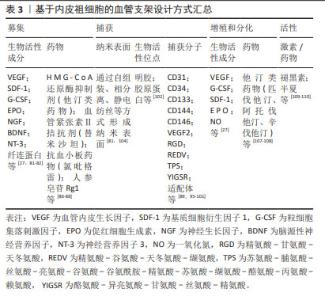
2.3 基于内皮祖细胞、间充质干细胞的血管支架表面改性 2.3.1 基于内皮祖细胞的血管支架表面设计 外周血中循环内皮祖细胞的浓度较低[67],往往不足以实现球囊损伤/支架植入损伤后的快速内皮化恢复,因此研究者往往会对材料表面进行改性以更好地募集、捕获骨髓和循环中的内皮祖细胞,增加内皮祖细胞与损伤部位结合。目前对支架表面改性以实现内皮祖细胞在局部损伤部位的聚集与修复的方式有多种,如何增强内皮祖细胞动员归巢、黏附、增殖、分化以及保护其活性以保证其旁分泌治疗作用等是近年来研究者们重点研究方向。下面将从募集、捕获、增殖与分化等方面展开讨论。 (1)募集:动员内皮祖细胞的因子有多种,如血管内皮生长因子、基质细胞衍生因子1、粒细胞集落刺激因子、HMG-CoA还原酶抑制剂(他汀类药物)、过氧化酶体增殖物激活受体γ激动剂、血管紧张素Ⅱ拮抗剂等 [27,81-82]。此外神经营养因子3也可以诱导内皮祖细胞动员和归巢加速内皮化,并通过抑制平滑肌细胞增生等抑制内膜增生[83]。其中粒细胞集落刺激因子和血管内皮生长因子等因子不仅会募集内皮祖细胞还可能动员炎症细胞。研究表明短期给予粒细胞集落刺激因子治疗能够防止动脉粥样硬化发生发展,而长期或频繁给药可能会促进动脉粥样硬化发展[84]。而基质细胞衍生因子1虽然能够促进内皮化,但是其可能会通过募集平滑肌祖细胞而增加内膜增生的风险[85],因而在设计血管支架表面时应注意避开或不要单独使用这些因子。 目前研究发现一些药物能够募集内皮祖细胞:替米沙坦(一种血管紧张素Ⅱ受体阻滞剂)能够显著募集内皮祖细胞,促进内皮化,减少内膜增生[86];西洛他唑、氯吡格雷等抗血小板药物通过募集内皮祖细胞到血管损伤部位来促进内皮损伤修复[87];人参皂苷Rg1能够募集内皮祖细胞,抑制血管平滑肌细胞的异常增殖,抑制内膜增生[88]。 (2)捕获:捕获内皮祖细胞的方式包括建立纳米表面、提供生物活性结合位点以及捕获分子修饰。纳米表面主要通过相分离、自组装以及静电纺丝等方式建立;生物活性结合位点主要是通过明胶、胶原蛋白等模拟细胞外基质[82];捕获分子表面设计则是目前研究较多的方向,下面将就此方向展开讨论。目前已知的内皮祖细胞表面标志物有多种,包括CD31、CD34、CD133、CD144(VE-钙黏蛋白)、CD146以及血管内皮生长因子2等[89]。尽管已有较多研究利用内皮祖细胞表面标志物与抗体之间的特异性结合反应,在支架表面涂覆这些抗体,成功设计了能够一定程度解决支架内再狭窄问题的血管支架[90],但这些抗体不具备高度特异性:如CD34和CD133在造血干细胞表面存在[91],血管内皮生长因子2在巨噬细胞表面表达[92]。以最经典的内皮祖细胞捕获支架CD34抗体表面包被支架为例,其捕获到的CD34+细胞不仅可以分化为内皮细胞,还可以分化为平滑肌细胞,存在着促内膜增生的风险[93]。因而也逐渐诞生了了联合使用多种表面标志物的设计方式,如CHEN等[94]通过CD34抗体联合VE-钙黏蛋白抗体设计出具有抗血小板黏附、晚期内皮祖细胞特异性捕获等功能的支架。未来通过联合使用多种抗体或其他生物分子有助于减少炎症、内膜增生等由非特异性结合引发的风险。 捕获内皮祖细胞还有许多方式,包括利用特殊的糖、肽/蛋白质或核酸序列以实现内皮祖细胞与支架表面的特异性结合。其中研究最多的为精氨酸-甘氨酸-天冬氨酸三肽序列(RGD),研究表明环状RGD与受体的亲和力优于线状RGD[95],但RGD会与血小板相互识别结合而导致血栓形成风险增加[96],最近HAO等[97]通过OBOC高通量组合筛选技术筛选出了一种能够特异性结合内皮祖细胞/内皮细胞但不与血小板黏附的配体LXW7,他们使用聚乙二醇接头将内皮祖细胞特异性结合配体LXW7接枝在支架表面,实现内源性内皮祖细胞尤其是晚期内皮祖细胞捕获的同时能够防止血小板黏附[98],不仅促进了再内皮化,还降低了血栓形成和内膜增生的风险,为解决非特异性结合问题提供了很好的思路,这提示即便没有寻找到天然的特异性抗体,也可以通过高通量筛选等方法,从抗原表面的特定结构域着手人工合成特异性结合配体。此外,REDV[99]、TPS[100]、YIGSR等也是研究较多的几类肽[101],层粘连蛋白、胶原[102]、适配体等也是用于实现捕获的有效分子[103]。 (3)增殖与分化:细胞因子/生长因子如血管内皮生长因子、粒细胞集落刺激因子、基质细胞衍生因子1、促红细胞生成素等,这些因子能够促进内皮祖细胞的增殖和分化[27],可以作为联合使用的辅助因子与材料结合用于诱导内皮祖细胞捕获后的增殖与分化,但应用时需要注意,一些因子可能会导致内膜增生。一氧化氮也影响着内皮细胞分化,它不仅兼具着抗血栓的功能还能够抑制内皮祖细胞向平滑肌细胞分化而减少内膜增生。目前实现支架表面稳定递送一氧化氮的方式包括创建催化位点,使内源性内皮一氧化氮前体(S-亚硝基硫醇)与之反应,产生以及利用一氧化氮供体如将S-亚硝基-N-乙酰青霉胺(SNAP)和S-亚硝基谷氨酰谷胱甘肽(GSNO)实现一氧化氮缓释[104-105]。但需要注意的是一氧化氮的疗效具有剂量依赖性,研究发现适当浓度范围内(100 nmol/L-10 μmol/L)的一氧化氮可以抑制干细胞向血管平滑肌细胞分化,但较高的一氧化氮水平(> 1 mmol/L)会产生促成骨分化的作用,从而增加血管钙化的风险[106],因此在设计一氧化氮缓释表面时应注意测定释放速率与释放量以避免不良反应的发生。 研究发现多种他汀类药物如匹伐他汀、阿托伐他汀、辛伐他汀等可以促进内皮祖细胞增殖,这类药物能够维持早期内皮祖细胞的活力并延缓晚期内皮祖细胞衰老的发生,这有助于改善具有糖尿病等基础疾病患者的内皮祖细胞活性,延长内皮祖细胞在这些患者中的治疗有效时长[107],这些他汀类药物可以通过改装成为载药纳米颗粒装配到支架表面[108],在内皮祖细胞归巢后促进其增殖并发挥功能保护作用。 除了从内皮祖细胞的募集、捕获、增殖、分化等方面考虑支架表面改性,维持内皮祖细胞活性,防止其损伤/凋亡亦是一个重要的设计点,有研究发现半夏(Pinellia ternata)能够通过PI3K/AKT信号通路增强内皮祖细胞的活性并减少内膜增生[109];褪黑素可以通过减轻氧化应激保护内皮祖细胞,保证其功能完整性[110]。 基于内皮祖细胞的血管支架表面设计方式汇总见表3。"

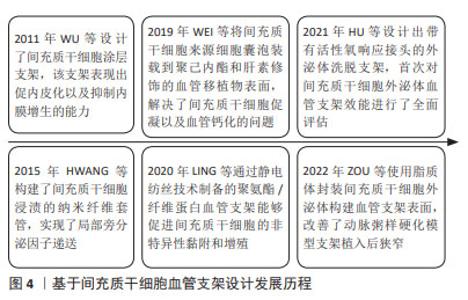
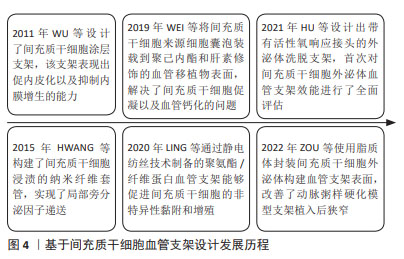
2.3.2 基于间充质干细胞的血管支架表面设计 基于间充质干细胞的血管支架设计发展历程见图4。截至目前基于间充质干细胞的血管支架设计研究较少,现有基于间充质干细胞的支架设计主要是通过形成纳米表面以实现间充质干细胞的非特异性黏附,从而发挥抗炎、血管重塑作用,如YANG等[111]采用静电纺丝技术将聚氨酯和纤维蛋白混合制备的聚氨酯/纤维蛋白血管支架能够促进间充质干细胞的黏附和增殖。早期研究主要通过细胞涂覆或浸渍形成功能支架,2011年有研究将间充质干细胞接种在316L SS支架的蛋白涂层上,表现出促进内皮化、抑制内膜增生的能力[112],2015年HWANG等[113]使用静电纺丝技术构建了间充质干细胞浸渍的纳米纤维支架套管,这些研究初步证明了将间充质干细胞纳入血管支架表面改性设计方案具有一定价值,但并没有讨论这类支架应用时血栓形成等不良反应。随着研究的不断推进,解决间充质干细胞促凝问题的方案也逐渐被提出,研究表明联合使用肝素抗凝治疗能够有效减少急性血栓形成[114],且肝素还具有促间充质干细胞增殖的能力[115]。最近JOSHI等[116]将脂肪来源间充质干细胞与内皮细胞共同接种在肝素化的聚己内酯/明胶共纺纳米纤维上,改善血栓问题的同时实现了快速内皮化;RANGASAMI等[117]通过层层自组装将间充质干细胞涂覆在明胶和肝素形成的聚合物表面,保留间充质干细胞旁分泌功能的同时减少了血栓形成。"
| [1] VISHWAKARMA A, SHARPE P, SHI ST, et al. Stem Cell Biology and Tissue Engineering in Dental Sciences. Boston: Academic Press. 2015:1-13. [2] BRIGNIER AC, GEWIRTZ AM. Embryonic and adult stem cell therapy. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S336-344. [3] ROBERTSON JA. Embryo stem cell research: ten years of controversy. J Law Med Ethics. 2010;38(2):191-203. [4] 曹雪洁,陶佳平,曲爱娟,等.血管壁干细胞与血管重塑相关性疾病[J].中国动脉硬化杂志,2022,30(11):921-929. [5] BIANCONI V, SAHEBKAR A, KOVANEN P, et al. Endothelial and cardiac progenitor cells for cardiovascular repair: A controversial paradigm in cell therapy. Pharmacol Ther. 2018;181:156-168. [6] SUN LL, LIU Z, RAN F, et al. Non-coding RNAs regulating endothelial progenitor cells for venous thrombosis: promising therapy and innovation. Stem Cell Res Ther. 2024;15(1):7. [7] WILS J, FAVRE J, BELLIEN J. Modulating putative endothelial progenitor cells for the treatment of endothelial dysfunction and cardiovascular complications in diabetes. Pharmacol Ther. 2017;170:98-115. [8] HICKSON LJ, EIRIN A, LERMAN LO. Challenges and opportunities for stem cell therapy in patients with chronic kidney disease. Kidney Int. 2016;89(4):767-778. [9] BARQUERA S, PEDROZA-TOBÍAS A, MEDINA C, et al. Global Overview of the Epidemiology of Atherosclerotic Cardiovascular Disease. Arch Med Res. 2015;46(5):328-338. [10] PETRIE JR, GUZIK TJ, TOUYZ RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34(5):575-584. [11] BOBRYSHEV YV, OREKHOV AN, CHISTIAKOV DA. Vascular stem/progenitor cells: current status of the problem. Cell Tissue Res. 2015;362(1):1-7. [12] WANG X, WANG R, JIANG L, et al. Endothelial repair by stem and progenitor cells. J Mol Cell Cardiol. 2022;163:133-146. [13] CHENG CC, CHANG SJ, CHUEH YN, et al. Distinct angiogenesis roles and surface markers of early and late endothelial progenitor cells revealed by functional group analyses. BMC Genomics. 2013;14:182. [14] YAN F, LIU X, DING H, et al. Paracrine mechanisms of endothelial progenitor cells in vascular repair. Acta Histochem. 2022;124(1): 151833. [15] MEDINA RJ, BARBER CL, SABATIER F, et al. Endothelial Progenitors: A Consensus Statement on Nomenclature. Stem Cells Transl Med. 2017;6(5):1316-1320. [16] AFRA S, MATIN MM. Potential of mesenchymal stem cells for bioengineered blood vessels in comparison with other eligible cell sources. Cell Tissue Res. 2020;380(1):1-13. [17] IKHAPOH I. Regulatory Mechanisms Underlying the Differentiation of Mesenchymal Stem Cells to Endothelial Cells. Creighton University. 2016. [18] WANG C, LI Y, YANG M, et al. Efficient Differentiation of Bone Marrow Mesenchymal Stem Cells into Endothelial Cells in Vitro. Eur J Vasc Endovasc Surg. 2018;55(2):257-265. [19] ZITTERMANN SI, ISSEKUTZ AC. Endothelial growth factors VEGF and bFGF differentially enhance monocyte and neutrophil recruitment to inflammation. J Leukoc Biol. 2006;80(2):247-257. [20] LIU Y, CHEN J, LIANG H, et al. Human umbilical cord-derived mesenchymal stem cells not only ameliorate blood glucose but also protect vascular endothelium from diabetic damage through a paracrine mechanism mediated by MAPK/ERK signaling. Stem Cell Res Ther. 2022;13(1):258. [21] BAI S, YIN Q, DONG T, et al. Endothelial progenitor cell-derived exosomes ameliorate endothelial dysfunction in a mouse model of diabetes. Biomed Pharmacother. 2020;131:110756. [22] LI L, WANG H, ZHANG J, et al. Effect of endothelial progenitor cell-derived extracellular vesicles on endothelial cell ferroptosis and atherosclerotic vascular endothelial injury. Cell Death Discov. 2021; 7(1):235. [23] MATHIYALAGAN P, LIANG Y, KIM D, et al. Angiogenic Mechanisms of Human CD34+ Stem Cell Exosomes in the Repair of Ischemic Hindlimb. Circ Res. 2017;120(9):1466-1476. [24] XIAO X, XU M, YU H, et al. Mesenchymal stem cell-derived small extracellular vesicles mitigate oxidative stress-induced senescence in endothelial cells via regulation of miR-146a/Src. Signal Transduct Target Ther. 2021;6(1):354. [25] LI Z, XU Y, LU S, et al. Bone mesenchymal stem cell extracellular vesicles delivered miR let-7-5p alleviate endothelial glycocalyx degradation and leakage via targeting ABL2. Cell Commun Signal. 2023;21(1):205. [26] WANG D, GAO B, YUE J, et al. Exosomes from mesenchymal stem cells expressing miR-125b inhibit neointimal hyperplasia via myosin IE. J Cell Mol Med. 2019;23(2):1528-1540. [27] GOH ET, WONG E, FARHATNIA Y, et al. Accelerating in situ endothelialisation of cardiovascular bypass grafts. Int J Mol Sci. 2014; 16(1):597-627. [28] SIMONCINI S, TOUPANCE S, LABAT C, et al. Functional Impairment of Endothelial Colony Forming Cells (ECFC) in Patients with Severe Atherosclerotic Cardiovascular Disease (ASCVD). Int J Mol Sci. 2022; 23(16):8969. [29] BLOOM SI, ISLAM MT, LESNIEWSKI LA, et al. Mechanisms and consequences of endothelial cell senescence. Nat Rev Cardiol. 2023; 20(1):38-51. [30] MUNDI S, MASSARO M, SCODITTI E, et al. Endothelial permeability, LDL deposition, and cardiovascular risk factors-a review. Cardiovasc Res. 2018;114(1):35-52. [31] BARRETT TJ, SCHLEGEL M, ZHOU F, et al. Platelet regulation of myeloid suppressor of cytokine signaling 3 accelerates atherosclerosis. Sci Transl Med. 2019;11(517):eaax0481. [32] LIBBY P. The changing landscape of atherosclerosis. Nature. 2021; 592(7855):524-533. [33] JEBARI-BENSLAIMAN S, GALICIA-GARCÍA U, LARREA-SEBAL A, et al. Pathophysiology of Atherosclerosis. Int J Mol Sci. 2022;23(6):3346. [34] EVANS CE, IRUELA-ARISPE ML, ZHAO YY. Mechanisms of Endothelial Regeneration and Vascular Repair and Their Application to Regenerative Medicine. Am J Pathol. 2021;191(1):52-65. [35] NAITO T, SHUN M, NISHIMURA H, et al. Pleiotropic effect of erythropoiesis-stimulating agents on circulating endothelial progenitor cells in dialysis patients. Clin Exp Nephrol. 2021;25(10):1111-1120. [36] YUAN Z, KANG L, WANG Z, et al. 17β-estradiol promotes recovery after myocardial infarction by enhancing homing and angiogenic capacity of bone marrow-derived endothelial progenitor cells through ERα-SDF-1/CXCR4 crosstalking. Acta Biochim Biophys Sin (Shanghai). 2018; 50(12):1247-1256. [37] WEI H, TAN T, CHENG L, et al. MRI tracing of ultrasmall superparamagnetic iron oxide nanoparticle‑labeled endothelial progenitor cells for repairing atherosclerotic vessels in rabbits. Mol Med Rep. 2020;22(4):3327-3337. [38] ALTABAS V, BILOŠ LSK. The Role of Endothelial Progenitor Cells in Atherosclerosis and Impact of Anti-Lipemic Treatments on Endothelial Repair. Int J Mol Sci. 2022;23(5):2663. [39] KE X, LIAO Z, LUO X, et al. Endothelial colony-forming cell-derived exosomal miR-21-5p regulates autophagic flux to promote vascular endothelial repair by inhibiting SIPL1A2 in atherosclerosis. Cell Commun Signal. 2022;20(1):30. [40] MAUSE SF, RITZEL E, DECK A, et al. Engagement of the CXCL12-CXCR4 Axis in the Interaction of Endothelial Progenitor Cell and Smooth Muscle Cell to Promote Phenotype Control and Guard Vascular Homeostasis. Int J Mol Sci. 2022;23(2):867. [41] MA Y, GU T, HE S, et al. Development of stem cell therapy for atherosclerosis. Mol Cell Biochem. 2023. doi: 10.1007/s11010-023-04762-8. [42] ZHANG X, REN Z, JIANG Z. EndMT-derived mesenchymal stem cells: a new therapeutic target to atherosclerosis treatment. Mol Cell Biochem. 2023;478(4):755-765. [43] MA J, CHEN L, ZHU X, et al. Mesenchymal stem cell-derived exosomal miR-21a-5p promotes M2 macrophage polarization and reduces macrophage infiltration to attenuate atherosclerosis. Acta Biochim Biophys Sin (Shanghai). 2021;53(9):1227-1236. [44] LI J, XUE H, LI T, et al. Exosomes derived from mesenchymal stem cells attenuate the progression of atherosclerosis in ApoE-/- mice via miR-let7 mediated infiltration and polarization of M2 macrophage. Biochem Biophys Res Commun. 2019;510(4):565-572. [45] YANG W, YIN R, ZHU X, et al. Mesenchymal stem-cell-derived exosomal miR-145 inhibits atherosclerosis by targeting JAM-A. Mol Ther Nucleic Acids. 2020;23:119-131. [46] ZHANG N, LUO Y, ZHANG H, et al. Exosomes Derived from Mesenchymal Stem Cells Ameliorate the Progression of Atherosclerosis in ApoE-/- Mice via FENDRR. Cardiovasc Toxicol. 2022;22(6):528-544. [47] 刘小春,吴素慧,王文珍,等.人脐带和脂肪来源间充质干细胞培养上清对内皮细胞血管新生作用[J].中华医学杂志,2020,100(6): 456-459. [48] LI Y, SHI G, LIANG W, et al. Allogeneic Adipose-Derived Mesenchymal Stem Cell Transplantation Alleviates Atherosclerotic Plaque by Inhibiting Ox-LDL Uptake, Inflammatory Reaction and Endothelial Damage in Rabbits. Cells. 2023;12(15):1936. [49] LI Z, YANG A, YIN X, et al. Mesenchymal stem cells promote endothelial progenitor cell migration, vascularization, and bone repair in tissue-engineered constructs via activating CXCR2-Src-PKL/Vav2-Rac1. FASEB J. 2018;32(4):2197-2211. [50] LEE J, HENDERSON K, MASSIDDA MW, et al. Mechanobiological conditioning of mesenchymal stem cells for enhanced vascular regeneration. Nat Biomed Eng. 2021;5(1):89-102. [51] FAN M, BAI J, DING T, et al. Adipose-Derived Stem Cell Transplantation Inhibits Vascular Inflammatory Responses and Endothelial Dysfunction in Rats with Atherosclerosis. Yonsei Med J. 2019;60(11):1036-1044. [52] 刘峰涛,于紫英.血管平滑肌细胞与动脉粥样硬化斑块稳定性的研究进展[J].中国心血管杂志,2021,26(3):299-302. [53] BYRNE RA, JONER M, KASTRATI A. Stent thrombosis and restenosis: what have we learned and where are we going? The Andreas Grüntzig Lecture ESC 2014. Eur Heart J. 2015;36(47):3320-3331. [54] WU B, MOTTOLA G, SCHALLER M, et al. Resolution of vascular injury: Specialized lipid mediators and their evolving therapeutic implications. Mol Aspects Med. 2017;58:72-82. [55] MELNIK T, JORDAN O, CORPATAUX JM, et al. Pharmacological prevention of intimal hyperplasia: A state-of-the-art review. Pharmacol Ther. 2022;235:108157. [56] ABOU-SALEH H, HACHEM A, YACOUB D, et al. Endothelial progenitor cells inhibit platelet function in a P-selectin-dependent manner. J Transl Med. 2015;13:142. [57] ABOU-SALEH H, YACOUB D, THÉORÊT JF, et al. Endothelial progenitor cells bind and inhibit platelet function and thrombus formation. Circulation. 2009;120(22):2230-2239. [58] LI WD, LI XQ. Endothelial progenitor cells accelerate the resolution of deep vein thrombosis. Vascul Pharmacol. 2016;83:10-16. [59] MOLDOVAN NI, ASAHARA T. Role of blood mononuclear cells in recanalization and vascularization of thrombi: past, present, and future. Trends Cardiovasc Med. 2003;13(7):265-269. [60] CARNEIRO GD, SIELSKI MS, VIEIRA CP, et al. Administration of endothelial progenitor cells accelerates the resolution of arterial thrombus in mice. Cytotherapy. 2019;21(4):444-459. [61] FENG Y, LEI B, ZHANG H, et al. MicroRNA-136-5p from Endothelial Progenitor Cells-released Extracellular Vesicles Mediates TXNIP to Promote the Dissolution of Deep Venous Thrombosis. Shock. 2022; 57(5):714-721. [62] WU X, JIANG J, GU Z, et al. Mesenchymal stromal cell therapies: immunomodulatory properties and clinical progress. Stem Cell Res Ther. 2020 ;11(1):345. [63] GUILLAMAT-PRATS R. Role of Mesenchymal Stem/Stromal Cells in Coagulation. Int J Mol Sci. 2022;23(18):10393. [64] NETSCH P, ELVERS-HORNUNG S, UHLIG S, et al. Human mesenchymal stromal cells inhibit platelet activation and aggregation involving CD73-converted adenosine. Stem Cell Res Ther. 2018;9(1):184. [65] YANG B, LONG Y, ZHANG A, et al. Procoagulant Properties of Mesenchymal Stem Cells and Extracellular Vesicles: A Novel Aspect of Thrombosis Pathogenesis. Stem Cells. 2024;42(2):98-106. [66] COPPIN L, SOKAL E, STÉPHENNE X. Thrombogenic Risk Induced by Intravascular Mesenchymal Stem Cell Therapy: Current Status and Future Perspectives. Cells. 2019;8(10):1160. [67] SUN H, MORIHARA R, FENG T, et al. Human Cord Blood-Endothelial Progenitor Cells Alleviate Intimal Hyperplasia of Arterial Damage in a Rat Stroke Model. Cell Transplant. 2023;32:9636897231193069. [68] WANG W, ZHANG Y, HUI H, et al. The effect of endothelial progenitor cell transplantation on neointimal hyperplasia and reendothelialisation after balloon catheter injury in rat carotid arteries. Stem Cell Res Ther. 2021;12(1):99. [69] XU RW, ZHANG WJ, ZHANG JB, et al. A Preliminary Study of the Therapeutic Role of Human Early Fetal Aorta-derived Endothelial Progenitor Cells in Inhibiting Carotid Artery Neointimal Hyperplasia. Chin Med J (Engl). 2015;128(24):3357-3362. [70] CHEN K, LI Y, XU L, et al. Comprehensive insight into endothelial progenitor cell-derived extracellular vesicles as a promising candidate for disease treatment. Stem Cell Res Ther. 2022;13(1):238. [71] SHOJI M, OSKOWITZ A, MALONE CD, et al. Human mesenchymal stromal cells (MSCs) reduce neointimal hyperplasia in a mouse model of flow-restriction by transient suppression of anti-inflammatory cytokines. J Atheroscler Thromb. 2011;18(6):464-474. [72] KIM AK, KIM MH, KIM DH, et al. Inhibitory effects of mesenchymal stem cells in intimal hyperplasia after balloon angioplasty. J Vasc Surg. 2016;63(2):510-517. [73] ISO Y, USUI S, TOYODA M, et al. Bone marrow-derived mesenchymal stem cells inhibit vascular smooth muscle cell proliferation and neointimal hyperplasia after arterial injury in rats. Biochem Biophys Rep. 2018;16:79-87. [74] CAI C, KILARI S, ZHAO C, et al. Therapeutic Effect of Adipose Derived Mesenchymal Stem Cell Transplantation in Reducing Restenosis in a Murine Angioplasty Model. J Am Soc Nephrol. 2020;31(8):1781-1795. [75] HADE MD, SUIRE CN, SUO Z. Mesenchymal Stem Cell-Derived Exosomes: Applications in Regenerative Medicine. Cells. 2021;10(8):1959. [76] LIU Z, WU C, ZOU X, et al. Exosomes derived from mesenchymal stem cells inhibit neointimal hyperplasia by activating the Erk1/2 signalling pathway in rats. Stem Cell Res Ther. 2020;11(1):220. [77] DENG Y, LI Y, CHU Z, et al. Exosomes from umbilical cord-derived mesenchymal stem cells combined with gelatin methacryloyl inhibit vein graft restenosis by enhancing endothelial functions. J Nanobiotechnology. 2023;21(1):380. [78] CHENG G, WANG X, LI Y, et al. Let-7a-transfected mesenchymal stem cells ameliorate monocrotaline-induced pulmonary hypertension by suppressing pulmonary artery smooth muscle cell growth through STAT3-BMPR2 signaling. Stem Cell Res Ther. 2017;8(1):34. [79] 刘指挥.间充质干细胞外泌体对血管损伤后新生内膜形成的影响与机制研究[D].重庆:西南大学,2020. [80] 郑仕杰,周敬群,杨维华,等.血管损伤后TGF-β1/Smad信号通路在诱导BMSCs分化参与血管再狭窄的相关性研究[J].中国医药科学,2019,9(17):50-54. [81] ZENG W, WEN C, WU Y, et al. The use of BDNF to enhance the patency rate of small-diameter tissue-engineered blood vessels through stem cell homing mechanisms. Biomaterials. 2012;33(2):473-484. [82] ZHUANG Y, ZHANG C, CHENG M, et al. Challenges and strategies for in situ endothelialization and long-term lumen patency of vascular grafts. Bioact Mater. 2020;6(6):1791-1809. [83] CHEN Y, CAO J, PENG W, et al. Neurotrophin-3 accelerates reendothelialization through inducing EPC mobilization and homing. Open Life Sci. 2020;15(1):241-250. [84] LIU P, ZHOU B, GU D, et al. Endothelial progenitor cell therapy in atherosclerosis: a double-edged sword? Ageing Res Rev. 2009 ;8(2):83-93. [85] HU A, SHUAI Z, LIU J, et al. Ginsenoside Rg1 prevents vascular intimal hyperplasia involved by SDF-1α/CXCR4, SCF/c-kit and FKN/CX3CR1 axes in a rat balloon injury. J Ethnopharmacol. 2020;260:113046. [86] LEE CH, LIU KS, ROTH JG, et al. Telmisartan Loaded Nanofibers Enhance Re-Endothelialization and Inhibit Neointimal Hyperplasia. Pharmaceutics. 2021;13(11):1756. [87] FUKAWA N, UEDA T, OGOSHI T, et al. Vascular Endothelial Repair and the Influence of Circulating Antiplatelet Drugs in a Carotid Coil Model. J Cent Nerv Syst Dis. 2021;13:11795735211011786. [88] XU S, HU A, CHEN J, et al. The role of calcium-sensing receptor in ginsenoside Rg1 promoting reendothelialization to inhibit intimal hyperplasia after balloon injury. Biomed Pharmacother. 2023;163:114843. [89] SALYBEKOV AA, KOBAYASHI S, ASAHARA T. Characterization of Endothelial Progenitor Cell: Past, Present, and Future. Int J Mol Sci. 2022;23(14):7697. [90] XIAO ST, KUANG CY. Endothelial progenitor cells and coronary artery disease: Current concepts and future research directions. World J Clin Cases. 2021;9(30):8953-8966. [91] CHRISTOPHER AC, VENKATESAN V, KARUPPUSAMY KV, et al. Preferential Expansion of Human CD34+CD133+CD90+ Hematopoietic Stem Cells Enhances Gene-Modified Cell Frequency for Gene Therapy. Hum Gene Ther. 2022;33(3-4):188-201. [92] LAI YS, WAHYUNINGTYAS R, AUI SP, et al. Autocrine VEGF signalling on M2 macrophages regulates PD-L1 expression for immunomodulation of T cells. J Cell Mol Med. 2019;23(2):1257-1267. [93] ROTMANS JI, HEYLIGERS JM, VERHAGEN HJ, et al. In vivo cell seeding with anti-CD34 antibodies successfully accelerates endothelialization but stimulates intimal hyperplasia in porcine arteriovenous expanded polytetrafluoroethylene grafts. Circulation. 2005;112(1):12-18. [94] CHEN H, WANG X, ZHOU Q, et al. Preparation of Vascular Endothelial Cadherin Loaded-Amphoteric Copolymer Decorated Coronary Stents for Anticoagulation and Endothelialization. Langmuir. 2017;33(46): 13430-13437. [95] KÄMMERER PW, HELLER M, BRIEGER J, et al. Immobilisation of linear and cyclic RGD-peptides on titanium surfaces and their impact on endothelial cell adhesion and proliferation. Eur Cell Mater. 2011;21: 364-372. [96] SÁNCHEZ-CORTÉS J, MRKSICH M. The platelet integrin alphaIIbbeta3 binds to the RGD and AGD motifs in fibrinogen. Chem Biol. 2009;16(9): 990-1000. [97] HAO D, LIN J, LIU R, et al. A bio-instructive parylene-based conformal coating suppresses thrombosis and intimal hyperplasia of implantable vascular devices. Bioact Mater. 2023;28:467-479. [98] HAO D, XIAO W, LIU R, et al. Discovery and Characterization of a Potent and Specific Peptide Ligand Targeting Endothelial Progenitor Cells and Endothelial Cells for Tissue Regeneration. ACS Chem Biol. 2017;12(4):1075-1086. [99] DUAN Y, YU S, XU P, et al. Co-immobilization of CD133 antibodies, vascular endothelial growth factors, and REDV peptide promotes capture, proliferation, and differentiation of endothelial progenitor cells. Acta Biomater. 2019;96:137-148. [100] YANG Z, ZHAO X, HAO R, et al. Bioclickable and mussel adhesive peptide mimics for engineering vascular stent surfaces. Proc Natl Acad Sci U S A. 2020;117(28):16127-16137. [101] LEE JS, LEE K, MOON SH, et al. Mussel-inspired cell-adhesion peptide modification for enhanced endothelialization of decellularized blood vessels. Macromol Biosci. 2014;14(8):1181-1189. [102] II M, TAKESHITA K, IBUSUKI K, et al. Notch signaling regulates endothelial progenitor cell activity during recovery from arterial injury in hypercholesterolemic mice. Circulation. 2010;121(9):1104-1112. [103] CHEN W, ZENG W, SUN J, et al. Construction of an Aptamer-SiRNA Chimera-Modified Tissue-Engineered Blood Vessel for Cell-Type-Specific Capture and Delivery. ACS Nano. 2015;9(6):6069-6076. [104] LI L, CAO Z, ZHANG C, et al. A Versatile Passivated Protein-Adsorption Platform for Rapid Healing of Vascular Stents by Modulating the Microenvironment. Adv Funct Mater. 2024;34:2312243. [105] DE MEL A, NAGHAVI N, COUSINS BG, et al. Nitric oxide-eluting nanocomposite for cardiovascular implants. J Mater Sci Mater Med. 2014;25(3):917-929. [106] WANG F, QIN K, WANG K, et al. Nitric oxide improves regeneration and prevents calcification in bio-hybrid vascular grafts via regulation of vascular stem/progenitor cells. Cell Rep. 2022;39(12):110981. [107] ANTÓNIO N, SOARES A, FERNANDES R, et al. Endothelial progenitor cells in diabetic patients with myocardial infarction - can statins improve their function? Eur J Pharmacol. 2014;741:25-36. [108] LIU H, BAO P, LI L, et al. Pitavastatin nanoparticle-engineered endothelial progenitor cells repair injured vessels. Sci Rep. 2017;7(1): 18067. [109] LU HK, HUANG Y, LIANG XY, et al. Pinellia ternata attenuates carotid artery intimal hyperplasia and increases endothelial progenitor cell activity via the PI3K/Akt signalling pathway in wire-injured rats. Pharm Biol. 2020;58(1):1184-1191. [110] LEE FY, SUN CK, SUNG PH, et al. Daily melatonin protects the endothelial lineage and functional integrity against the aging process, oxidative stress, and toxic environment and restores blood flow in critical limb ischemia area in mice. J Pineal Res. 2018;65(2):e12489. [111] YANG L, LI X, WU Y, et al. Preparation of PU/Fibrin Vascular Scaffold with Good Biomechanical Properties and Evaluation of Its Performance in vitro and in vivo. Int J Nanomedicine. 2020;15:8697-8715. [112] WU X, WANG G, TANG C, et al. Mesenchymal stem cell seeding promotes reendothelialization of the endovascular stent. J Biomed Mater Res A. 2011;98(3):442-449. [113] HWANG CW, JOHNSTON PV, GERSTENBLITH G, et al. Stem cell impregnated nanofiber stent sleeve for on-stent production and intravascular delivery of paracrine factors. Biomaterials. 2015;52: 318-326. [114] LIAO L, SHI B, CHANG H, et al. Heparin improves BMSC cell therapy: Anticoagulant treatment by heparin improves the safety and therapeutic effect of bone marrow-derived mesenchymal stem cell cytotherapy. Theranostics. 2017;7(1):106-116. [115] LING L, CAMILLERI ET, HELLEDIE T, et al. Effect of heparin on the biological properties and molecular signature of human mesenchymal stem cells. Gene. 2016;576(1 Pt 2):292-303. [116] JOSHI A, XU Z, IKEGAMI Y, et al. Co-culture of mesenchymal stem cells and human umbilical vein endothelial cells on heparinized polycaprolactone/gelatin co-spun nanofibers for improved endothelium remodeling. Int J Biol Macromol. 2020;151:186-192. [117] RANGASAMI VK, ASAWA K, TERAMURA Y, et al. Biomimetic polyelectrolyte coating of stem cells suppresses thrombotic activation and enhances its survival and function. Biomater Adv. 2023;147: 213331. [118] WEI Y, WU Y, ZHAO R, et al. MSC-derived sEVs enhance patency and inhibit calcification of synthetic vascular grafts by immunomodulation in a rat model of hyperlipidemia. Biomaterials. 2019;204:13-24. [119] HU S, LI Z, SHEN D, et al. Exosome-eluting stents for vascular healing after ischaemic injury. Nat Biomed Eng. 2021;5(10):1174-1188. [120] ZOU D, YANG P, LIU J, et al. Exosome-Loaded Pro-efferocytic Vascular Stent with Lp-PLA2-Triggered Release for Preventing In-Stent Restenosis. ACS Nano. 2022;16(9):14925-14941. [121] PARK KS, KANG SN, KIM DH, et al. Late endothelial progenitor cell-capture stents with CD146 antibody and nanostructure reduce in-stent restenosis and thrombosis. Acta Biomater. 2020;111:91-101. [122] WANG CH, CHERNG WJ, YANG NI, et al. Late-outgrowth endothelial cells attenuate intimal hyperplasia contributed by mesenchymal stem cells after vascular injury. Arterioscler Thromb Vasc Biol. 2008;28(1):54-60. [123] THANASKODY K, JUSOP AS, TYE GJ, et al. MSCs vs. iPSCs: Potential in therapeutic applications. Front Cell Dev Biol. 2022;10:1005926. [124] GAO A, HANG R, LI W, et al. Linker-free covalent immobilization of heparin, SDF-1α, and CD47 on PTFE surface for antithrombogenicity, endothelialization and anti-inflammation. Biomaterials. 2017;140: 201-211. [125] PELLICCIA F, ZIMARINO M, DE LUCA G, et al. Endothelial Progenitor Cells in Coronary Artery Disease: From Bench to Bedside. Stem Cells Transl Med. 2022;11(5):451-460. [126] XIANG Q, TIAN F, XU J, et al. New insight into dyslipidemia-induced cellular senescence in atherosclerosis. Biol Rev Camb Philos Soc. 2022; 97(5):1844-1867. [127] BASMAEIL YS, BAHATTAB E, ALSHABIBI MA, et al. Human Decidua Basalis mesenchymal stem/stromal cells reverse the damaging effects of high level of glucose on endothelial cells in vitro. J Cell Mol Med. 2021;25(4):1838-1850. |
| [1] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Yang Zhihang, Sun Zuyan, Huang Wenliang, Wan Yu, Chen Shida, Deng Jiang. Nerve growth factor promotes chondrogenic differentiation and inhibits hypertrophic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1336-1342. |
| [3] | Hu Taotao, Liu Bing, Chen Cheng, Yin Zongyin, Kan Daohong, Ni Jie, Ye Lingxiao, Zheng Xiangbing, Yan Min, Zou Yong. Human amniotic mesenchymal stem cells overexpressing neuregulin-1 promote skin wound healing in mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1343-1349. |
| [4] | Jin Kai, Tang Ting, Li Meile, Xie Yuan. Effects of conditioned medium and exosomes of human umbilical cord mesenchymal stem cells on proliferation, migration, invasion, and apoptosis of hepatocellular carcinoma cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1350-1355. |
| [5] | Li Dijun, Jiu Jingwei, Liu Haifeng, Yan Lei, Li Songyan, Wang Bin. Three-dimensional gelatin microspheres loaded human umbilical cord mesenchymal stem cells for chronic tendinopathy repair [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1356-1362. |
| [6] | Liu Qi, Li Linzhen, Li Yusheng, Jiao Hongzhuo, Yang Cheng, Zhang Juntao. Icariin-containing serum promotes chondrocyte proliferation and chondrogenic differentiation of stem cells in the co-culture system of three kinds of cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1371-1379. |
| [7] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [8] | Li Jialin, Zhang Yaodong, Lou Yanru, Yu Yang, Yang Rui. Molecular mechanisms underlying role of mesenchymal stem cell secretome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1512-1522. |
| [9] | He Bo, Chen Wen, Ma Suilu, He Zhijun, Song Yuan, Li Jinpeng, Liu Tao, Wei Xiaotao, Wang Weiwei, Xie Jing . Pathogenesis and treatment progress of flap ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1230-1238. |
| [10] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [11] | Sun Xianjuan, Wang Qiuhua, Zhang Jinyi, Yang Yangyang, Wang Wenshuang, Zhang Xiaoqing. Adhesion, proliferation, and vascular smooth muscle differentiation of bone marrow mesenchymal stem cells on different electrospinning membranes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 661-669. |
| [12] | Zheng Yitong, Wang Yongxin, Liu Wen, Amujite, Qin Hu. Action mechanism of intrathecal transplantation of human umbilical cord mesenchymal stem cell-derived exosomes for repair of spinal cord injury under neuroendoscopy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7743-7751. |
| [13] | Guo Zhao, Zhuang Haoyan, Shi Xuewen. Role of exosomes derived from mesenchymal stem cells in treatment of colorectal cancer [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7872-7879. |
| [14] | Ge Xiao, Zhao Zhuangzhuang, Guo Shuyu, Xu Rongyao. HOXA10 gene-modified bone marrow mesenchymal stem cells promote bone regeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7701-7708. |
| [15] | Zhang Xiongjinfu, Chen Yida, Cheng Xinyi, Liu Daihui, Shi Qin . Exosomes derived from bone marrow mesenchymal stem cells of young rats to reverse senescence in aged rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7709-7718. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||