Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (20): 3259-3264.doi: 10.12307/2024.356
Previous Articles Next Articles
Measurement and evaluation of proprioception of foot and ankle complexes
Feng Liang1, Zhang Yafei2, Huo Hongfeng1, 3
- 1School of Physical Education, Hebei Normal University, Shijiazhuang 050024, Hebei Province, China; 2Clinical School of Hebei Medical University, Shijiazhuang 050017, Hebei Province, China; 3Hebei Province Key Laboratory of Human Sports Biological Information Evaluation, Shijiazhuang 050024, Hebei Province, China
-
Received:2023-05-08Accepted:2023-06-07Online:2024-07-18Published:2023-09-11 -
Contact:Huo Hongfeng, Master, Senior experimentalist, School of Physical Education, Hebei Normal University, Shijiazhuang 050024, Hebei Province, China; Hebei Province Key Laboratory of Human Sports Biological Information Evaluation, Shijiazhuang 050024, Hebei Province, China -
About author:Feng Liang, Master, School of Physical Education, Hebei Normal University, Shijiazhuang 050024, Hebei Province, China
CLC Number:
Cite this article
Feng Liang, Zhang Yafei, Huo Hongfeng. Measurement and evaluation of proprioception of foot and ankle complexes[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(20): 3259-3264.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
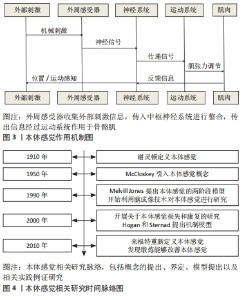
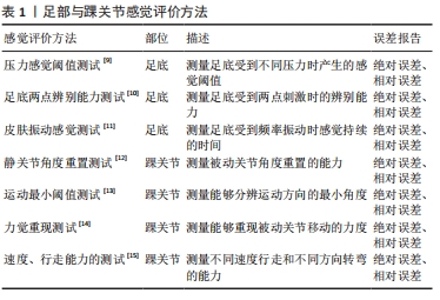
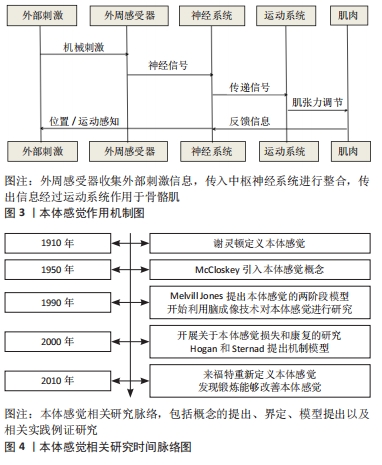
通过对纳入文献的阅读与梳理,明晰了本体感觉的研究脉络以及作用机制,见图3,4。研究重点聚焦到足踝感觉评价方法时发现,对足踝复合体感觉的评价主要分为对足部的感觉评价和踝关节的本体感觉评价[9-21],部分研究成果见表1。足部的感觉评价主要描述其皮肤的感觉,方法主要包括:压力感觉阈值测试、足底两点辨别能力测试、皮肤振动感觉持续时间测试。踝关节本体感觉评价着重描述关节位置、运动范围、力值及功能表现,方法主要分为静态的关节角度重置测试、运动最小阈值测试、力觉重现测试以及动静态平衡、速度、行走能力的测试。对量化结果的报道一般以“误差”来表示,根据报道的需要一般分为:绝对误差(absolute error,AE)、变量误差(variable error,VE)、恒定误差(constant error,CE)以及归一化绝对误差(normalized absolute error,NAE)等。"
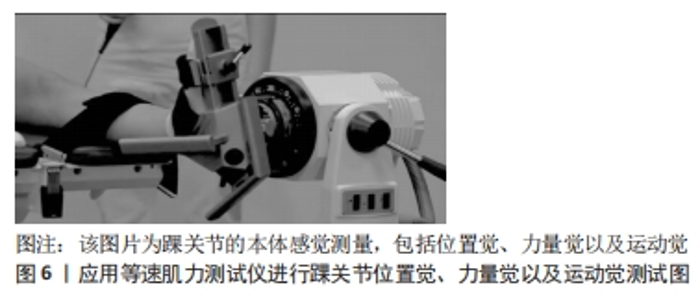
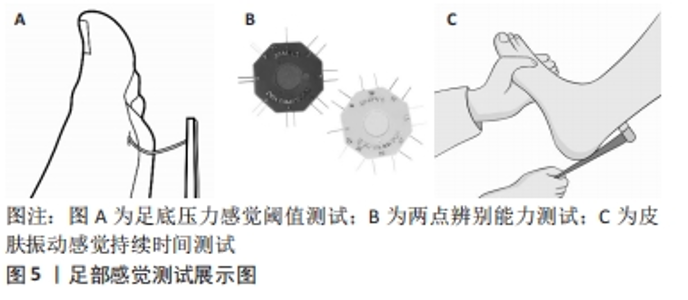
两点辨别能力测试通过使用触觉测量仪对足底前足和足跟进行两点辨别能力评估[22,24],并将2个刺激点之间的最小距离(mm)作为得分,在每个位置的3次试验中2次被正确地识别距离为测量结果。每种条件下进行3次试验(两点刺激、一点刺激、假试验)和位置随机进行,并要求受试者报告刺激的数量(即2个,1个,或没有)。该程序首先测试最大距离(50 mm),以确保受试者识别两种不同刺激的能力。如果受试者正确地识别出这一点,将继续进行最小的测试距离(10 mm),并增加5 mm的增量,直到45 mm,直到达到阈值。两点辨别阈值定义为2个刺激点之间的最小距离,以毫米为单位。 皮肤振动感觉持续时间测试是一种可靠有效的临床工具,用于评估振动感知障碍[25-26]。使用128 Hz音叉评估双侧第一跖骨头和内踝的振动感觉[27]。评估人员在参与者脚旁的橡胶垫表面敲击音叉,以引起音叉尖部的剧烈运动。然后,音叉被垂直放置在预定的骨头突起或皮肤上。振动刺激的持续时间由精密计时器记录下来,从音叉的激活时间开始,直到参与者报告他/她感觉不到它,用于分析的是每个部位3次试验的平均时间(s)。 2.2 踝关节本体感觉的静态评价 2.2.1 关节角度重置测试 受试者仰卧位姿势在测试平台上,要求受试者戴眼罩、塞软耳塞或戴播放有电磁干扰声的耳麦,将优势侧足放于充气套中再与等速测力计装置的测试臂通过绑带固定;先确定好受试者的踝关节跖屈背屈的完整运动幅度(角度°),随后在运动范围内从0°向跖屈和背屈方向每隔5°选取一个角度,预设为目标角度。分别让受试者感受目标角度,并识记目标角度之后进行复现。正式复现时每一角度测试3次,被动运动角速度5 (°)/s。比较2次角度的差异,判断测试结果精确度采用2次角度的绝对误差表示[28]。 2.2.2 运动最小阈值测试 在告知受试者开始测试后的3-10 s 内,随机开始利用等速动力装置提供持续而缓慢的关节被动运动,被动运动角速度0.5 (°)/s,起始角度为踝关节0°向跖屈和背屈方向每隔5°选取一个角度,预设为目标角度,每个角度顺时针和逆时针方向各运动测试3次,测量关节能够感知到的被动运动的运动阈值,即测量起始时运动的关节角度与受试者能够觉察到运动时的关节角度。比较2次角度的差异,判断测试结果精确度采用2次角度的绝对误差表示[29]。 2.2.3 力量重现法 等速测力装置设定为等长肌力测试模式,见图6。首先进行受试者最大自主等长收缩测试,获得最大自主等长收缩肌力(maximal voluntary isometric contraction,MVIC);各关节角度进行3次5 s的等长伸展肌力测试,次间休息5 s,组间休息300 s,去除疲劳影响,变异系数(coefficient of variance,CV)要求控制在15%以下。休息30 min后,以MVIC的50%作为目标力值[31],要求受试者保持这个目标力值(在电脑屏幕上目标力值处画线,受试者通过视觉反馈控制发力大小),同时让受试者注意感受此时用力的大小;在此之后,要求受试者闭上眼睛,产生5 s相同大小力量输出并记录为实测力值。计算目标力值与实测力值的差异采用2次测试结果的绝对误差表示[30]。"

2.3 踝关节本体感觉的动态评价以及间接评价 对踝关节本体感觉的动态评价以及间接评价也是非常重要的测评方法:主动运动程度辨别评估(Active Movement and Extension Discrimination Assessment,AMEDA)来测试踝关节本体感觉[32]。AMEDA测试是通过向参与者展示不同程度的主动运动来进行的,区分这些程度的能力被视为他们的感官灵敏度。在每次实验中,参与者主动进行脚踝的反转,以达到目标角度;跌落着陆测试中的脚踝本体感觉(ankle inversion and dorsiflexion assessment of the landing,AIDAL)用于测试下降着陆期间的脚踝本体感觉[33]。着陆测试平台有4个角度:10°,12°,14°和16°,按从小到大的顺序编号为1,2,3,4。 参与者赤脚站在跳跃平台上,双手放在髂峰的上边缘,并保持头部和眼睛向前。在每次测试中,参与者在测试者的指导下从起跳平台跳到测试平台,要求参与者自然弯曲臀部和膝盖,同时脚落地。在正式测试之前,参与者被要求熟悉三轮(12次试验)的4个脚踝反转着陆姿势。在正式测试期间,随机出现了4个角度的着陆测试平台,总共进行了40次试验(每次脚踝翻转10次试验)。参与者被要求对着陆后脚踝反转的角度作出绝对判断,并立即给出一个数字。此过程不应该向参与者提供正确和错误的反馈。一些研究人员将“平衡感”纳入本体感觉的定义中。遵循这一逻辑,平衡任务可以作为替代方法,以(间接)评估使用非意识本体感觉(以保持平衡状态)的功能能力,特别是在视觉信息被消除的情况下(即参与者被蒙住眼睛)。静态平衡是指在支撑基础内保持身体质量中心的能力,可以通过专业的静态平衡测试平台完成,通过分析压力中心轨迹的长度、轨迹变化速率、包络面积以及偏移方向对静态平衡做出评价;而动态平衡需要用适当的反应来处理外部扰动,除了使用专业的动态平衡测试平台测试外,还可以使用便捷式的Y形人体动态平衡测试,通过评分来反映结果[33]。"

| [1] CHEN Z, HAN J, WADDINGTON G, et al. Somatosensory perception sensitivity in voluntary postural sway movements: age, gender and sway effect magnitudes. Exp Gerontol. 2019;122:53-59. [2] KUNKEL D, POTTER J, MAMODE L. A cross-sectional observational study comparing foot and ankle characteristics in people with stroke and healthy controls. Disabil Rehabil. 2017;39(12):1149-1154. [3] WITCHALLS J, BLANCH P, WADDINGTON G, et al. Intrinsic functional deficits associated with increased risk of ankle injuries: a systematic review with meta-analysis. Br J Sports Med. 2012;46(7):515-523. [4] KNOX MF, CHIPCHASE LS, SCHABRUN SM, et al. Anticipatory and compensatory postural adjustments in people with low back pain: a systematic review and meta-analysis. Spine J. 2018;18(10):1934-1949. [5] ASSLANDER L, PETERKA RJ. Sensory reweighting dynamics in human postural control. J Neurophysiol. 2014;111(9):1852-1864. [6] UETA Y, MATSUGI A, OKU K, et al. Gaze stabilization exercises derive sensory reweighting of vestibular for postural control. J Phys Ther Sci. 2017;29(9): 1494-1496. [7] JULIE B, KATHRYN SH, GERT K, et al. Agreed definitions and a shared vision for new standards in stroke recovery research: the stroke recovery and rehabilitation roundtable taskforce. Int J Stroke. 2017,12(5):444-450. [8] COLLETT J, FLEMING MK, MEESTER D, et al. Dual-task walking and automaticity after Stroke: Insights from a secondary analysis and imaging sub-study of a randomised controlled trial. Clin Rehabil. 2021;35(11): 1599-1610. [9] TESARZ J, EICH W, TREEDE R, et al. Altered pressure pain thresholds and increased wind-up in adult patients with chronic back pain with a history of childhood maltreatment: a quantitative sensory testing study. Pain. 2016; 157(8):1799-1809. [10] DELLON AL, MUSE VL, SCOTT ND, et al. A positive Tinel sign as predictor of pain relief or sensory recovery after decompression of chronic tibial nerve compression in patients with diabetic neuropathy. J Reconstruc Microsurg. 2012;28(4):235-240. [11] GILMAN S. Joint position sense and vibration sense: anatomical organisation and assessment. Journal of neurology, neurosurgery, and psychiatry. J Neurol Neurosurg Psychiatry. 2002;73(5):473-477. [12] LJL, JI ZQ, LI YX, et al. Correlation study of knee joint proprioception test results using common testmethods. J Phys Ther Sci. 2016;28(2):478-482. [13] ROBERT JS, EMMA K. Motion perception in the ageing visual system: minimum motion, motion coherence, and speed discrimination thresholds. Perception. 2006;35(1):9-24. [14] MINOO KZ, BAHRAM A, ASGHAR R, et al. Measurement of force sense reproduction in the knee joint: application of anew dynamometric device. J Phys Ther Sci. 2016;28(8):2311-2315. [15] VAN HEDEL HJ, WIRZ M, DIETZ V. Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Physical Med Rehabil. 2005;86(2):190-196. [16] JAMES RA, WILLIAM JP, WILLIAM GC. Arthroscopy of the ankle: technique and normal anatomy. Foot Ankle. 1985;6(1):29-33. [17] CHARIS M, KENNEETH R. Assessing mobility in elderly people. A review of performance-based measures of balance, gait and mobility for bedside use. Rev Clin Gerontol. 1995;5(4):615. [18] BOYLE J, NEGUS V. Joint position sense in the recurrently sprained ankle. Aust J Physiother. 1998;44(3):159-163. [19] YOU SH. Joint position sense in elderly fallers: a preliminary investigation of the validity and reliability of the SENSERite measure. Arch Physical Med Rehabil. 2005;86(2):346-352. [20] KATHY L, JOSEPH G, ERIK W, et al. mining the diagnostic accuracy of dynamic postural stability measures in differentiating among ankle instability status. Clin Biomech. 2013;28(2):211-217. [21] ELANGOVAN N, HERRMANNA, KONCZAK J. Assessing proprioceptive function: evaluating joint position matching methods against psychophysical thresholds. Phys Ther. 2014;94(4):553-561. [22] MEYERB C, LYDEN PD. The modified national institutes of health stroke scale: its time has come. Int J Stroke. 2009;4(4):267-273. [23] CRUZ-ALMEIDA Y, BLACK ML, CHRISTOU EA, et al. Site-specific differences in the association between plantar tactile perception and mobility function in older adults. Front Aging Neurosci. 2014;6:68. [24] PATEL AT, DUNCAN PW, LAI SM, et al. The relation between impairments and functional outcomes poststroke. Arch Phys Med Rehabil. 2000;81(10):1357-1363. [25] MENZ HB, TIEDEMANN A, KWAN MM, et al. Reliability of clinical tests of foot and ankle characteristics in older people. J Am Podiatr Med Assoc. 2003;93(5):380-387. [26] CORNWALL MW, MCPOIL TG, LEBEC M, et al. Reliability of the modified foot posture index. J Am Podiatr Med Assoc. 2008;98(1):7-13. [27] AULD ML, BOYD R, MOSELEY G L, et al. Tactile function in children with unilateral cerebral palsy compared to typically developing children. Disabil Rehabil. 2012;34(17):1488-1494. [28] 尹彦.功能性踝关节不稳者动态姿势稳定性评价方法及其影响因素的研究[D].北京:北京体育大学,2016. [29] HORVATH A, FERENTZI E, SCHWARTZ K, et al. The measurement of proprioceptive accuracy: a systematic literature review. J Sport Health Sci. 2023;12(2):219-225. [30] 张秋霞,花秀琴,施永健.踝关节本体感觉的测量方法研究与应用[J].中国组织工程研究与临床康复,2011,15(35):6619-6623. [31] 李林,纪仲秋,李艳霞,等.关节角度重置法、运动最小阈值测量法和力量重现法的相关性研究[J].天津体育学院学报,2016,31(1):36-40. [32] YANG N, ADAMS R, WADDINGTON G, et al. Ankle complex proprioception and plantar cutaneous sensation in older women with different physical activity levels. Exp Brain Res. 2022;240(3):981-989. [33] LIU Y, SONG Q, ZHOU Z, et al. Effects of fatigue on balance and ankle proprioception during drop landing among individuals with and without chronic ankle instability. J Biomech. 2023;146:111431. [34] PAPPAS E, HAGINS M, SHEIKHZADEH A, et al. Biomechanical differences between unilateral and bilateral landings from a jump: gender differences. Clin J Sport Med. 2007;17(4):263-268. [35] LESINSKI M, HORTOBAGYI T, MUEHLBAUER T, et al. Effects of balance training on balance performance in healthy older adults: a systematic review and meta-analysis. Sports medicine (Auckland, N.Z.). 2015;45(12): 1721-1738. [36] 朱婷,安丙辰,梁贞文,等.认知对姿势控制能力影响的研究进展[J].中华老年病研究电子杂志,2015,2(1):35-38. [37] Kandel ER. Principles of Neural Science. Psychological Medicine. McGraw-Hill Medical. 2001. [38] KLOUS M, MIKULIC P, LATASH ML. Two aspects of feedforward postural control: anticipatory postural adjustments and anticipatory synergy adjustments. J Neurophysiol. 2011;105(5):2275-2288. [39] BERGQUIST R, WEBER M, SCHWENK M, et al. Performance-based clinical tests of balance and muscle strength used in young seniors: a systematic literature review. BMC Geriatrics. 2019;19(1):1471-2318. [40] 杨凯,黄万红,杨禹珺,等.传统导引对慢性踝关节不稳干预研究[J].湖北医药学院学报,2021,40(4):378-381,390. [41] NEILSON LJ, MACASKILL LA, LUK J, et al. Children’s school-day nutrient intake in ontario: a cross-sectional observational study comparing students’ packed lunches from two school schedules. Nutrients. 2022;14(9):104-110. [42] PETERSEN BA, SPARTO PJ, FISHER LE. Clinical measures of balance and gait cannot differentiate somatosensory impairments in people with lower-limb amputation. Gait Posture. 2023;99:104-110. [43] SIRAGY T, NANTEL J. Quantifying dynamic balance in young, elderly and parkinson’s individuals: a systematic review. Front Aging Neurosci. 2018; 10:387. [44] BERGINP S, BRONSTEIN AM, MURRAY NM, et al. Body sway and vibration perception thresholds in normal aging and in patients with polyneuropathy. J Neurol Neurosurg Psychiatry. 1995;58(3):335-340. [45] LORD SR, CLARKR D, WEBSTER IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991; 46(3):M69-M76. [46] HELEN MB, NILS AH, MARKUS DJ, et al. The effects of a fatiguing lifting task on postural sway among males and females. Hum Mov Sci. 2018;59:193-200. [47] LI L, LI Y, WANGH, et al. Effect of force level and gender on pinch force perception in healthy adults. Iperception. 2020;11(3):2041669520927043. [48] DUZGUN I, KANBUR NO, BALTACI G, et al. Effect of Tanner stage on proprioception accuracy. J Foot Ankle Surg. 2011;50(1):11-15. [49] PETERS RM, MCKEOWN MD, CARPENTER MG, et al. Losing touch: age-related changes in plantar skin sensitivity, lower limb cutaneous reflex strength, and postural stability in older adults. J Neurophysiol. 2016;116(4): 1848-1858. [50] 张鹏,张琳,李向哲,等.以头眼运动为主的感觉运动整合训练对脑卒中偏瘫患者平衡及步行功能的影响[J].中国康复医学杂志,2023,38(1): 98-100. [51] KOO TK, LI MY. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. [52] HOPKINS WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30(1):1-15. [53] RANKIN G, STOKES M. Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil. 1998;12(3):187-199. [54] WEIR JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231-240. [55] AGEBERG E, FLENHAGEN J, LJUNG J. Test-retest reliability of knee kinesthesia in healthy adults. BMC Musculoskelet Disord. 2007;8:57. [56] ELLISON PH, SPARKS SA, MURPHY PN, et al. Determining eye-hand coordination using the sport vision trainer: an evaluation of test-retest reliability. Res Sports Med. 2014;22(1):36-48. [57] AANDSTAD A, SIMON EV. Reliability and validity of the soccer specific INTER field test. J Sports Sci. 2013;31(13):1383-1392. |
| [1] | Zhang Xihui, Li Zhengrong, Li Shineng, Xing Zengyu, Wang Jiao. Effect of rehabilitation training guided by Pro-kin balance system on proprioception and balance function of the affected knee after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1259-1264. |
| [2] | Cai Zhihao, Xie Zhaoyong. Femoral neck anteversion measurement assessment: how to establish a unified method and standard [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1448-1454. |
| [3] | Chen Peng, Wang Ling, Dong Shiyu, Ding Yue, Jia Shaohui, Kou Xianjuan, Zheng Cheng. Effects of whole-body vibration training on anterior cruciate ligament reconstruction: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(36): 5875-5883. |
| [4] | Yang Qiang, Huang Jian. Measurement research method and measurement equipment for knee-spine syndrome [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(29): 4751-4756. |
| [5] | Wu Yihan, Wei Qiaoye, Pang Yu, Liu Zhongqiang. Proprioception characteristics of functional ankle instability: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2943-2952. |
| [6] | Wang Ling, Chen Peng, Wang Guanglan, Zheng Cheng. Effects of kinesio taping on chronic ankle instability: a systematic review and Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(14): 2283-2290. |
| [7] | Lu Pan, Zhang Chunlin, Wang Yongkui, Yan Xu, Dong Chao, Yue Yisen, Li Long, Zhu Andi. Volume changes of cervical herniated discs after open-door laminoplasty and conservative treatment as assessed by three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1395-1401. |
| [8] | Liao Xinyu, He Lu, Li Yanlin, Wang Fuke, Zhou Xiaoxiang, Wang Xu, Zhong Ruiying, Wang Guoliang. Single-bundle anatomical reconstruction of the anterior cruciate ligament with residual ligament stump is beneficial to the recovery of proprioception [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(17): 2631-2635. |
| [9] | Chen Zehua, Ye Xiangling, Chen Weijian, Du Jianping, Liu Wengang, Xu Xuemeng. Effect of pronated foot posture on proprioception and postural stability based on foot posture index [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1324-1328. |
| [10] | Tan Biao, Zuo Biao, Huang Yong. Evaluation of balance function of unicompartmental and total knee arthroplasties for treating unicompartmental knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(6): 827-832. |
| [11] | Chen Zehua, Ye Xiangling, Chen Weijian, Xu Xuemeng. Relationship between proprioception and postural stability of lower limbs in healthy adults [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(29): 4692-4696. |
| [12] | Yan Xianke. Total knee arthroplasty through a midvastus approach reduces postoperative adverse reactions and accelerates functional recovery of the knee [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(21): 3336-3340. |
| [13] | Yin Lulu, Wang Lin. Effects of kinesio taping on motor neuromuscular control in chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(11): 1783-1789. |
| [14] | Feng Xinyuan, Bai Lunhao. Significance of preserving anterior cruciate ligament stump for the stability of knee joint [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 525-531. |
| [15] | Chai Hao, Wu Ting, Shu Li, Zhang Lei. Proprioception recovery after anterior cruciate ligament reconstruction with and without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(15): 2332-2337. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||