Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (21): 3338-3344.doi: 10.12307/2022.641
Previous Articles Next Articles
Effect of hydroxyapatite three-dimensional scaffolds with different apertures on the biological properties of MC3T3-E1 cells
Yang Jiaojiao1, Hu Ming1, Li Yan2, Xia Delin1
- 1Department of Oral and Maxillofacial Surgery, The Affiliated Stomatology Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China; 2Taizhou Polytechnic College, Bone Tissue Engineering Research Center of Taizhou, Taizhou 225300, Jiangsu Province, China
-
Received:2021-08-23Accepted:2021-10-11Online:2022-07-28Published:2022-01-28 -
Contact:Xia Delin, MD, Chief physician, Professor, Department of Oral and Maxillofacial Surgery, The Affiliated Stomatology Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Yang Jiaojiao, Master candidate, Department of Oral and Maxillofacial Surgery, The Affiliated Stomatology Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
Supported by:Luzhou Science and Technology Bureau Project, No. 2013-S-48(8/30) (to XDL); the Applied Basic Research Grant Project of Sichuan Science and Technology Department, No. 2008JY0014 (to XDL)
CLC Number:
Cite this article
Yang Jiaojiao, Hu Ming, Li Yan, Xia Delin. Effect of hydroxyapatite three-dimensional scaffolds with different apertures on the biological properties of MC3T3-E1 cells[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3338-3344.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

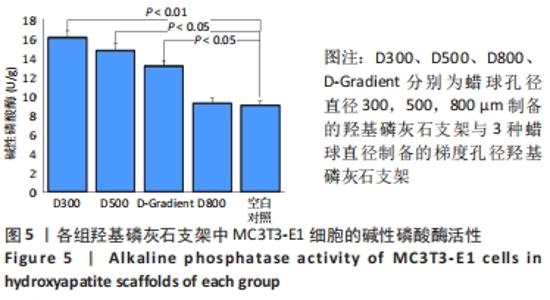
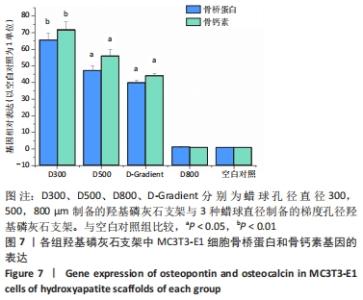
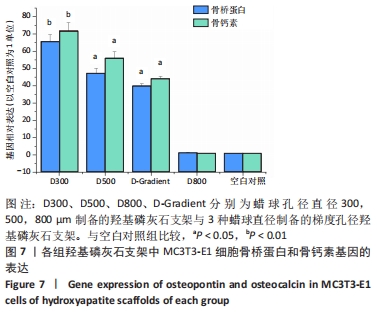
2.3.3 MC3T3-E1细胞骨架形态和黏着斑检测结果 见图6。与空白对照相比,各组支架上的细胞均呈现出较好的黏附及运动活性,其中D-Gradient组细胞发展最好、黏着最多,肌动蛋白纤维更加清晰可见。黏着斑与肌动蛋白荧光强度高低为:D-Gradient组>D500组>D800组>D300组>空白对照组。 2.3.4 MC3T3-E1细胞骨钙素与骨桥蛋白基因表达检测结果 见图7。与空白对照相比,D300组的骨桥蛋白和骨钙素基因表达活性明显增强(P < 0.01),更有利于促进成骨分化;D500组和D-Gradient组骨桥蛋白和骨钙素基因表达活性增强(P < 0.05),且两者的促进作用相近。骨桥蛋白与骨钙素基因表达量的高低为:D300组> D500组>D-Gradient组>D800组≈空白对照组。"

| [1] LEE JW, AHN G, KIM JY, et al. Evaluating cell proliferation based on internal pore size and 3D scaffold architecture fabricated using solid freeform fabrication technology. J Mater Sci Mater Med. 2010;21(12): 3195-3205. [2] AMINI AR, NUKAVARAPU SP. Oxygen-tension controlled matrices for enhanced osteogenic cell survival and performance. Ann Biomed Eng. 2014;42(6):1261-1270. [3] PEREZ RA, MESTRES G. Role of pore size and morphology in musculo-skeletal tissue regeneration. Mater Sci Eng C Mater Biol Appl. 2016;61: 922-939. [4] BAINO F, FIORILLI S, VITALE-BROVARONE C. Bioactive glass-based materials with hierarchical porosity for medical applications: Review of recent advances. Acta Biomater. 2016;42:18-32. [5] ZHANG Q, LU H, KAWAZOE N, et al. Preparation of collagen porous scaffolds with a gradient pore size structure using ice particulates. Mater Lett. 2013;107:280-283. [6] SHI D, SHEN J, ZHANG Z, et al. Preparation and properties of dopamine-modified alginate/chitosan-hydroxyapatite scaffolds with gradient structure for bone tissue engineering. J Biomed Mater Res A. 2019; 107(8):1615-1627. [7] MA H, XUE L, NIE T. Fabrication of PLLA scaffold with gradient macro/micro/nano structure by electrophoretic deposition of carbon nanotube. Mater Lett. 2015;159:185-188. [8] WILLIAMS JM, ADEWUNMI A, SCHEK RM, et al. Bone tissue engineering using polycaprolactone scaffolds fabricated via selective laser sintering. Biomaterials. 2005;26(23):4817-4827. [9] DI LUCA A, OSTROWSKA B, LORENZO-MOLDERO I, et al. Gradients in pore size enhance the osteogenic differentiation of human mesenchymal stromal cells in three-dimensional scaffolds. Sci Rep. 2016;6:22898. [10] LEE SJ, LEE IW, LEE YM, et al. Macroporous biodegradable natural/synthetic hybrid scaffolds as small intestine submucosa impregnated poly(D,L-lactide-co-glycolide) for tissue-engineered bone. J Biomater Sci Polym Ed. 2004;15(8):1003-1017. [11] SOBRAL JM, CARIDADE SG, SOUSA RA, et al. Three-dimensional plotted scaffolds with controlled pore size gradients: Effect of scaffold geometry on mechanical performance and cell seeding efficiency. Acta Biomater. 2011;7(3):1009-1018. [12] LIU B, CUI L, LIU GP, et al. [Tissue-engineering bone with ADSCs and coral scaffold for repairing of cranial bone defect in canine]. Zhonghua Zheng Xing Wai Ke Za Zhi. 2009;25(3):204-208. [13] FU R, LIU C, YAN Y, et al. Bone defect reconstruction via endochondral ossification: A developmental engineering strategy. J Tissue Eng. 2021; 12:20417314211004211. [14] GAO C, SOW WT, WANG Y, et al. Hydrogel composite scaffolds with an attenuated immunogenicity component for bone tissue engineering applications. J Mater Chem B. 2021;9(8):2033-2041. [15] WANG C, YUE H, HUANG W, et al. Cryogenic 3D printing of heterogeneous scaffolds with gradient mechanical strengths and spatial delivery of osteogenic peptide/TGF-β1 for osteochondral tissue regeneration. Biofabrication. 2020;12(2):025030. [16] SU X, WANG T, GUO S. Applications of 3D printed bone tissue engineering scaffolds in the stem cell field. Regen Ther. 2021;16:63-72. [17] CHANG BS, LEE CK, HONG KS, et al. Osteoconduction at porous hydroxyapatite with various pore configurations. Biomaterials. 2000; 21(12):1291-1298. [18] BOBYN JD, PILLIAR RM, CAMERON HU, et al. The optimum pore size for the fixation of porous-surfaced metal implants by the ingrowth of bone.Clin Orthop Relat Res. 1980;(150):263-270. [19] BAI F, WANG Z, LU J, et al. The correlation between the internal structure and vascularization of controllable porous bioceramic materials in vivo: a quantitative study. Tissue Eng Part A. 2010;16(12): 3791-3803. [20] XIAO X, WANG W, LIU D, et al. The promotion of angiogenesis induced by three-dimensional porous beta-tricalcium phosphate scaffold with different interconnection sizes via activation of PI3K/Akt pathways. Sci Rep. 2015;5:9409. [21] ITÄLÄ AI, YLÄNEN HO, EKHOLM C, et al. Pore diameter of more than 100 microm is not requisite for bone ingrowth in rabbits. J Biomed Mater Res. 2001;58(6):679-683. [22] KUBOKI Y, JIN Q, TAKITA H. Geometry of carriers controlling phenotypic expression in BMP-induced osteogenesis and chondrogenesis. J Bone Joint Surg Am. 2001;83-A Suppl 1(Pt 2):S105-115. [23] 郑威,董学明,何阳,等.生物活性聚合物及其复合材料在骨组织工程中的应用进展[J].哈尔滨工业大学学报,2021,53(8):1-16. [24] YEUNG M, ABDULMAJEED A, CARRICO CK, et al. Accuracy and precision of 3D-printed implant surgical guides with different implant systems: An in vitro study. J Prosthet Dent. 2020;123(6):821-828. [25] GOH YQ, OOI CP. Fabrication and characterization of porous poly(L-lactide) scaffolds using solid-liquid phase separation. J Mater Sci Mater Med. 2008;19(6):2445-2452. [26] 廖欣宇,王福科,王国梁.骨组织工程支架的进展与挑战[J].中国组织工程研究,2021,25(28):4553-4560. [27] 王启帆,马志勇,钟林娜,等.PCL/ZrO2骨组织工程支架3D打印制备方法及其性能研究[J].北京生物医学工程,2020,39(4):418-424. [28] LO DICO G, NUÑEZ ÁP, CARCELÉN V, et al. Machine-learning-accelerated multimodal characterization and multiobjective design optimization of natural porous materials. Chem Sci. 2021;12(27):9309-9317. [29] WU Z, LUO J, ZHANG J, et al. Silver-Releasing Micro-/Nanoporous Coating on Additively Manufactured Macroporous Ti-Ta-Nb-Zr Scaffolds with High Osseointegration and Antibacterial Properties. Coatings. 2021;11(6):716. [30] CABALLERO-FLORES H, NABESHIMA CK, SARRA G, et al. Development and characterization of a new chitosan-based scaffold associated with gelatin, microparticulate dentin and genipin for endodontic regeneration. Dent Mater. 2021;37(7):e414-e425. [31] XUE G, ZHANG Y, XIE T, et al. Cell Adhesion-Mediated Piezoelectric Self-Stimulation on Polydopamine-Modified Poly(vinylidene fluoride) Membranes. ACS Appl Mater Interfaces. 2021;13(15):17361-17371. [32] BLAINE J, DYLEWSKI J. Regulation of the Actin Cytoskeleton in Podocytes. Cells. 2020;9(7):1700. [33] SUN Y, LIU X, TAN J, et al. Strontium ranelate incorporated 3D porous sulfonated PEEK simulating MC3T3-E1 cell differentiation. Regen Biomater. 2020;8(1):rbaa043. [34] WANG X, CHEN T, DENG Z, et al. Melatonin promotes bone marrow mesenchymal stem cell osteogenic differentiation and prevents osteoporosis development through modulating circ_0003865 that sponges miR-3653-3p. Stem Cell Res Ther. 2021;12(1):150. [35] LI Q, LU F, CHEN T, et al. VPS4B mutation impairs the osteogenic differentiation of dental follicle cells derived from a patient with dentin dysplasia type I. Int J Oral Sci. 2020;12(1):22. [36] CHEN Y, HU Y, YANG L, et al. Effects of Different Concentrations of Glucose on the Osteogenic Differentiation of Orofacial Bone Mesenchymal Stem Cells. Sichuan Da Xue Xue Bao Yi Xue Ban. 2016; 47(5):679-684. [37] JAFARY F, HANACHI P, GORJIPOUR K. Osteoblast Differentiation on Collagen Scaffold with Immobilized Alkaline Phosphatasec Int J Organ Transplant Med. 2017;8(4):195-202. [38] VARMA SR, SHARATH KUMAR LM, VIDYASHANKAR S, et al. Water Soluble Components of ‘Osteocare’ Promote Cell Proliferation, Differentiation, and Matrix Mineralization in Human Osteoblast-Like SaOS-2 Cells. Sci Pharm. 2014;82(2):375-391. [39] HUH JE, YANG HR, PARK DS, et al. Puerariae radix promotes differentiation and mineralization in human osteoblast-like SaOS-2 cells. J Ethnopharmacol. 2006;104(3):345-350. [40] CHIEN HH, LIN WL, CHO MI. Expression of TGF-beta isoforms and their receptors during mineralized nodule formation by rat periodontal ligament cells in vitro. J Periodontal Res. 1999;34(6):301-309. [41] YE G, LI C, XIANG X, et al. Bone morphogenetic protein-9 induces PDLSCs osteogenic differentiation through the ERK and p38 signal pathways. Int J Med Sci. 2014;11(10):1065-1072. |
| [1] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [2] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [3] | Chen Chichi, Zhang Yu, He Jiachen, Shi Qin. Osteogenic differentiation of bone marrow mesenchymal stem cells in obese mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(24): 3846-3851. |
| [4] | Lu Haiping, Lang Xuemei, Zhang Cheng, Ju Songli, Zhang Yi, Wang Xin. Application of polycaprolactone modified biological barrier membrane in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3580-3585. |
| [5] | Liu Ming, Wang Kai. Theaflavin-3-gallate modified nano-hydroxyapatite/polycaprolactone composite porous scaffold in bone defect repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3480-3486. |
| [6] | Tang Zhenzhou, Gu Yong, Chen Liang. Preparation of modified dextran composite hydrogel with osteogenetic effect and in vitro experiment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3521-3527. |
| [7] | Meng Lulu, Liu Hao, Liu Han, Zhang Jun, Li Ruixin, Gao Lilan. Mechanical properties of silk fibroin/type I collagen/hydroxyapatite scaffolds based on low-temperature 3D printing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3550-3555. |
| [8] | Meng Zengdong, Zhu Bin, Zhang Yanan, Luo Lilin, Zhang Yuqin. Mechanical properties and biocompatibility of porous ZnO/hydroxyapatite composites with different porosities [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3498-3504. |
| [9] | Guo Xiaopeng, Liu Yingsong, Shang Hui. Silk fibroin/nano hydroxyapatite composite combined with icariin can promote the proliferation and differentiation of bone marrow mesenchymal stem cells into nucleus pulposus like cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3528-3534. |
| [10] | Liu Longzhu, Long Yuanzhu, Yang Chengxue, Zhong Xinqi, Wang Yifang, Liu Jianguo. Preparation and characterization of the composites of amino-modified artificial jaw nano-hydroxyapatite/polylactic acid [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3319-3326. |
| [11] | Zhang Chunyu, Hu Baoyang, Feng Yao, Zhang Wanfen, Sun Leiye, Yang Yan. Performance optimization of a new type of calcium silicate (based) scaffold matched with bone tissue regeneration in the bone defect area [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3421-3428. |
| [12] | Zhang Hongmei, Sun Xirao, Wang Chengyue. Effect of polymethyl methacrylate/mineralized collagen/Mg-Ca composite material on osteogenic differentiation of mouse preosteoblasts [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(16): 2498-2503. |
| [13] | Ma Ziyu, Zhang Yuntao, Ma Xiangrui, Qiao Luhui, Guo Haoyu, Hou Yudong. Surface treatment of iron oxide nanoparticles in bone defect repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(16): 2570-2575. |
| [14] | Tang Yanan, Gao Teng, Ren Guiyun. Preparation and biological properties of zinc-doped hydroxyapatite [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(16): 2602-2607. |
| [15] | Peng Huizhen, Cai Mingxiang, Liu Xiangning. Angiogenesis regulation in bone repair: new ideas and new methods [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(15): 2400-2405. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||