Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (12): 1917-1923.doi: 10.3969/j.issn.2095-4344.3790
Previous Articles Next Articles
Application of tourniquet affects thickness of bone cement penetration in total knee arthroplasty: a meta-analysis
Song Min, Lu Chao, Chen Jin, Wu Gaoyi, Li Congcong, Li Anan, Ye Guozhu, Lin Wenzheng, Cai Yuning, Liu Wengang, Xu Weipeng
- Guangdong Second Traditional Chinese Medicine Hospital, Guangzhou University of Chinese Medicine, Guangzhou 510095, Guangdong Province, China
-
Received:2020-04-22Revised:2020-04-25Accepted:2020-06-03Online:2021-04-28Published:2020-12-25 -
Contact:Liu Wengang, MD, Chief TCM physician, Doctoral supervisor, Guangdong Second Traditional Chinese Medicine Hospital, Guangzhou University of Chinese Medicine, Guangzhou 510095, Guangdong Province, China -
About author:Song Min, Master candidate, Guangdong Second Traditional Chinese Medicine Hospital, Guangzhou University of Chinese Medicine, Guangzhou 510095, Guangdong Province, China -
Supported by:the Scientific Research Project of Guangdong Provincial Bureau of Traditional Chinese Medicine, No. 20183001 (to LWG); the Scientific Research Project of Guangdong Administration of Traditional Chinese Medicine, No. 20191021 (to LC)
CLC Number:
Cite this article
Song Min, Lu Chao, Chen Jin, Wu Gaoyi, Li Congcong, Li Anan, Ye Guozhu, Lin Wenzheng, Cai Yuning, Liu Wengang, Xu Weipeng. Application of tourniquet affects thickness of bone cement penetration in total knee arthroplasty: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1917-1923.
share this article
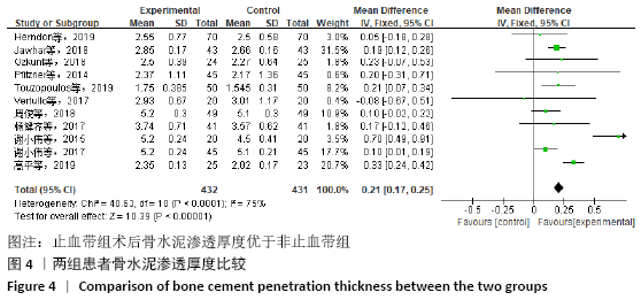
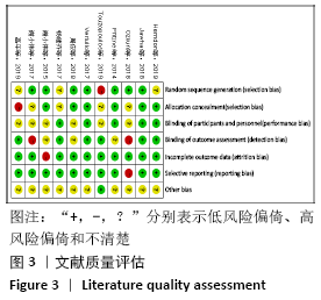
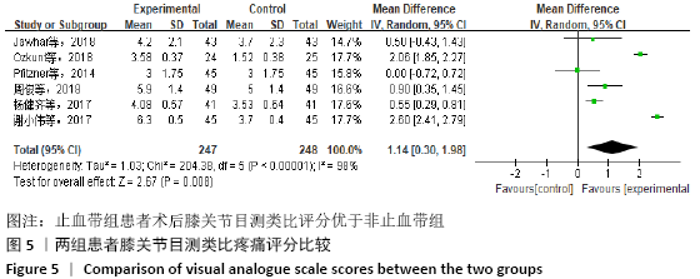
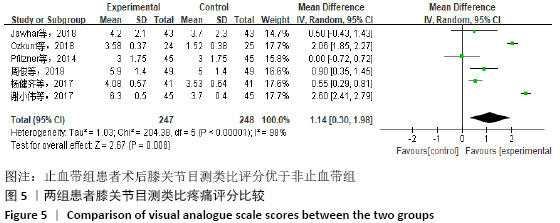
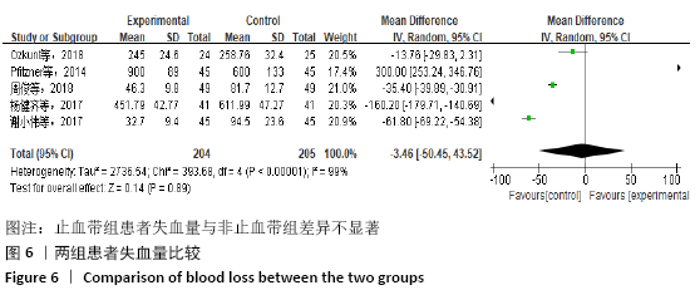
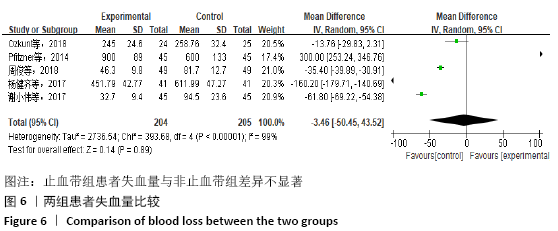
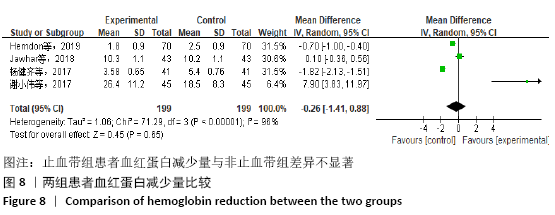
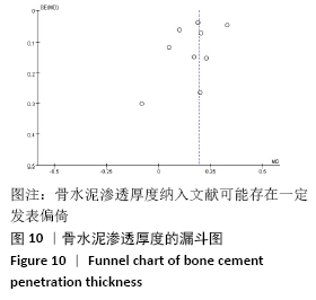
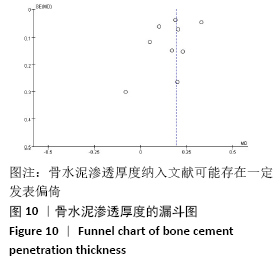
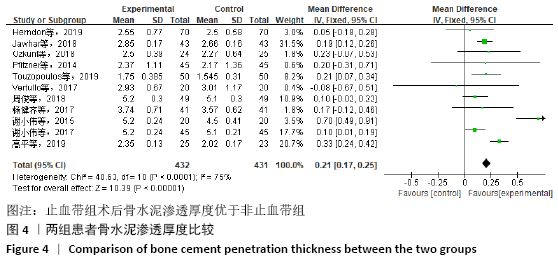
2.4 Meta分析结果 2.4.1 主要结局指标 (1)骨水泥渗透厚度:胫骨部分假体周围骨水泥渗入厚度是文章的主要结果之一。11项研究报道了骨水泥渗透厚度[7-9,12,15-17,19-21,23],共863例患者,试验组432例,对照组431例。经过异质性检验(I2=75%;MD=0.21,95%CI:0.04-0.25,P < 0.05),各研究组间有异质性,采用随机效应模型,经敏感性分析发现2篇文献中关于骨水泥渗透厚度的相关数据与其他文献中的均数不太一致[17,21],其他文献中骨水泥渗透厚度为2-4 mm,而这2篇文献为4-6 mm,且例数仅试验组与对照组各20例,考虑样本量数据少,测量分区及工具不一的影响,去除这2篇数据后,异质性I2=43%,发现余下的数据分析出的结果仍然提示两组骨水泥渗透厚度有显著差异,见图4。综上,止血带的应用能增加假体周围骨水泥渗透厚度。 "
| [1] 陆艳红,石晓兵.膝骨关节炎国内外流行病学研究现状及进展[J].中国中医骨伤科杂志,2012,20(6):81-84. [2] 刘铭柏,刘少津,乔荣勤,等.口服养血方联合蜡疗治疗膝骨关节炎气血虚弱证的疗效观察及作用机制分析[J].中医正骨,2018,30(9):67-69, 72. [3] 许蓓,林进.骨关节炎发病机制及治疗进展[J].浙江医学,2017, 39(21):1833-1835, 1851. [4] ZHANG P, LIANG Y, HE J, et al. Timing of tourniquet release in total knee arthroplasty: a meta-analysis. Medicine (Baltimore). 2017;96(17):e6786. [5] PARVIZI J, DIAZ-LEDEZMA C. Total knee replacement with the use of a tourniquet: more pros than cons. Bone Joint J. 2013; 95-B(11 Suppl A):133-134. [6] WANG K, NI S, LI Z, et al. The effects of tourniquet use in total knee arthroplasty: a randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9): 2849-2857. [7] TOUZOPOULOS P, VERVERIDIS A, MPOGIATZIS C, et al. The use of tourniquet may influence the cement mantle thickness under the tibial implant during total knee arthroplasty. Eur J Orthop Surg Traumatol. 2019;29(4):869-875. [8] PFITZNER T, VON ROTH P, VOERKELIUS N, et al. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):96-101. [9] Jawhar A, Stetzelberger V, Kollowa K, et al. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2071-2081. [10] LUTZ MJ, PINCUS PF, WHITEHOUSE SL, et al. The effect of cement gun and cement syringe use on the tibial cement mantle in total knee arthroplasty. J Arthroplasty. 2009;24(3):461-467. [11] MILLER MA, GOODHEART JR, IZANT TH, et al. Loss of cement-bone interlock in retrieved tibial components from total knee arthroplasties. Clin Orthop Related Res. 2014;472(1):304-313. [12] HERNDON CL, GROSSO MJ, SARPONG NO, et al. Tibial cement mantle thickness is not affected by tourniquetless total knee arthroplasty when performed with tranexamic acid. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1526-1531. [13] JAWHAR A, SKEIREK D, STETZELBERGER V, et al. Influence of the Tourniquet on Pain and Function in Total Knee Arthroplasty: a Systematic Review and Meta-Analysis. Z Orthop Unfall. 2019. doi: 10.1055/a-0983-3808. [14] 顾培伦,董金波,王维山,等.人工全膝关节置换中是否应用气囊止血带止血:一项Meta分析[J].中国组织工程研究, 2018,22(15):2446-2452. [15] VERTULLO CJ, NAGARAJAN M. Is cement penetration in TKR reduced by not using a tourniquet during cementation? A single blinded, randomized trial. J Orthop Surg (Hong Kong). 2017;25(1):2309499016684323. [16] OZKUNT O, SARIYILMAZ K, GEMALMAZ HC, et al. The effect of tourniquet usage on cement penetration in total knee arthroplasty: a prospective randomized study of 3 methods. Medicine. 2018;97(4): e9668. [17] 谢小伟,岳辰,黄泽宇,等.全膝关节置换术应用与不应用止血带的随机对照研究[J].中国矫形外科杂志, 2017,25(17): 1572-1576. [18] 杨健齐,魏鲁青,张健平,等.全膝关节置换术中止血带应用对假体骨水泥厚度影响的对照研究[J].重庆医学,2017, 46(6):782-785. [19] 高平,李会波,白正武,等.TKA术中不使用止血带对早期假体稳定性及膝关节功能的影响[J].中国骨与关节损伤杂志, 2019,34(12):1294-1296. [20] 周俊,钭伟国,欧阳海清,等.全膝关节置换术中不应用止血带对患者术后的影响[J].中国乡村医药,2018,25(23):10-11, 13. [21] 谢小伟.比较三种不同止血带方法:对初次全膝关节置换术患者早期康复及骨水泥厚度的影响[C].2015成都国际骨科论坛暨四川省医学会第19次骨科学术会议.2015. [22] 顾培伦.全膝关节置换术中是否应用止血带Meta分析[D].石河子:石河子大学, 2018. [23] 杨健齐.全膝关节置换术中止血带应用的研究进展[J].中华骨与关节外科杂志, 2018,11(11):877-880. [24] WANG FD, WANG YP, CHEN CF, et al. The incidence rate, trend and microbiological aetiology of prosthetic joint infection after total knee arthroplasty: a 13 years’ experience from a tertiary medical center in Taiwan. J Microbiol Immunol Infect. 2018;51(6):717-722. [25] EJAZ A, LAURSEN AC, KAPPEL A, et al. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85(4):422-426. [26] 杜传超,邱海滨,张衡,等.关于全膝关节置换术中使用止血带利弊随机对照性研究的系统回顾及Meta分析[J].中国骨与关节损伤杂志,2017,32(8):800-803. [27] YI S, TAN J, CHEN C, et al. The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2014;134(10):1469-1476. [28] 吴鑫杰,谭明生.充气式止血带在全膝关节置换术中应用的研究进展[J].中国矫形外科杂志,2018,26(17):1601-1604. [29] MAJKOWSKI RS, BANNISTER GC, MILES AW, et al. The effect of bleeding on the cement-bone interface. An experimental study. Clin Orthop Related Res. 1994;(299):293-297. [30] MOHER D, SHAMSEER L, CLARKE M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4(1):1. [31] HE S, ZHANG Y, LV N, et al. The effect of bone cement distribution on clinical efficacy after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Medicine. 2019;98(50):e18217. [32] Ledin H, Aspenberg P, Good L, et al. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012;83(5):499-503. [33] MOLT M, HARSTEN A, TOKSVIG-LARSEN S, et al. The effect of tourniquet use on fixation quality in cemented total knee arthroplasty a prospective randomized clinical controlled RSA trial. Knee. 2014;21(2):396-401. [34] BUCHER TA, BUTLER M, LEE C, et al. TKR without tourniquet: A laboratory study investigating the quality of the tibial cement mantle when using metaphyseal suction and cement gun. J Arthroscopy Joint Surg. 2015. doi:10.1016/j.jajs.2015.06.002. [35] Srinivasan P, Miller MA, Verdonschot N, et al. Strain shielding in trabecular bone at the tibial cement-bone interface. J Mech Behav Biomed Mater. 2017;66:181-186. [36] OLIVECRONA C, LAPIDUS J, BENSON L, et al. Tourniquet time affects postoperative complications after knee arthroplasty. Int Orthop. 2013;37(5):827-832. [37] GILLANI S, CAO J, SUZUKI T, et al. The effect of ischemia reperfusion injury on skeletal muscle. Injury. 2012;43(6):670-675. [38] MURATA I, NOZAKI R, OOI K, et al. Nitrite reduces ischemia/reperfusion-induced muscle damage and improves survival rates in rat crush injury model. J Trauma Acute Care Surg. 2012;72(6):1548-1554. [39] ZHANG P, LIANG Y, HE J, et al. Timing of tourniquet release in total knee arthroplasty: a meta-analysis. Medicine. 2017;96(17):e6786. [40] NA YG, BAMNE AB, WON HH, et al. After early release of tourniquet in total knee arthroplasty, should it be reinflated or kept deflated? A randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017; 25(9):2769-2777. [41] KOVESI T, ROYSTON D. Pharmacological approaches to reducing allogeneic blood exposure. Vox Sanguinis. 2003;84(1):2-10. [42] HU Y, LI Q, WEI BG, et al. Blood loss of total knee arthroplasty in osteoarthritis: an analysis of influential factors. J Orthop Surg Res. 2018;13(1):325. [43] CHEUY VA, FORAN JRH, PAXTON RJ, et al. Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty. 2017;32(8):2604-2611. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [5] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [6] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [7] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [8] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [9] | Peng Zhihao, Feng Zongquan, Zou Yonggen, Niu Guoqing, Wu Feng. Relationship of lower limb force line and the progression of lateral compartment arthritis after unicompartmental knee arthroplasty with mobile bearing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1368-1374. |
| [10] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [11] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [12] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [13] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [14] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [15] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||