Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (4): 632-637.doi: 10.3969/j.issn.2095-4344.2333
Previous Articles Next Articles
Development prospect of orthopedic rehabilitation medicine based on three-dimensional printing technology
Peng Kun1, Lin Yimin2, Gan Xiaoling1, Wu Zhiyong3
- 1Chongqing Medical and Pharmaceutical College, Chongqing 401331, China; 2Chongqing Key Laboratory of Translational Research for Cancer Metastasis and Individualized Treatment, Chongqing University Cancer Hospital, Chongqing 400030, China; 3Chongqing Gonggang Zhihui Additive Manufacturing Technology Service Co., Ltd., Chongqing 400030, China
-
Received:2019-12-18Revised:2020-01-04Accepted:2020-02-26Online:2021-02-08Published:2020-11-25 -
Contact:Lin Yimin, Chief technician, Chongqing Key Laboratory of Translational Research for Cancer Metastasis and Individualized Treatment, Chongqing University Cancer Hospital, Chongqing 400030, China -
About author:Peng Kun, MD, Associate professor, Chongqing Medical and Pharmaceutical College, Chongqing 401331, China -
Supported by:the Natural Science Foundation of Chongqing, No. cstc2018jcyjAX0828; the Backbone Teachers Foundation Youth Fund of Chongqing Colleges and Universities, No. 2016
CLC Number:
Cite this article
Peng Kun, Lin Yimin, Gan Xiaoling, Wu Zhiyong. Development prospect of orthopedic rehabilitation medicine based on three-dimensional printing technology[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 632-637.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
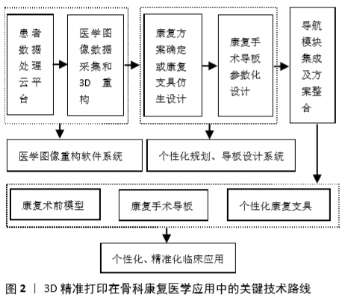
2.1 3D精准打印技术在骨科康复医学领域应用的现状 数字化精准医疗在骨科康复医学领域受到关注,3D打印技术的成熟为其发展提供了更大的空间。在临床治疗上,骨科康复治疗手术可凭借3D打印的医疗模型进行术前规划、术中导航等[8-10]。临床医学辅助人员可利用患者术前CT或MRI数据完成三维建模,生成可被识别的打印数据,利用医学 3D 打印机生成可辅助临床治疗的医学3D模型[11-13]。生成的医学3D模型可以协助医生开展手术训练、术前规划和术中指导,帮助医生或者患者更好地理解病患位置的医学治疗机制,设计符合手术需要的导板,帮助医生顺利实施手术,提高手术精准度,改善手术效果,提高患者满意度。 3D精准打印技术在骨科康复医疗领域应用的第一阶段是图像三维建模,但目前在医疗行业提供具有专业针对医疗应用3D重构软件开发及3D打印的技术创新平台尚属比较空白的领域[14-17]。建模软件个性化诊疗3D打印数字设计技术能够依据患者的一组医学CT或MRI图像重建出患处的三维数学模型,建模数据能与商业3D打印机无缝对接,是国际领先的专门针对医学领域应用的图像三维重构建模软件,市场上仅有比利时公司Materialise的Mimics软件拥有类似功能,但其主要为科研人员所设计,操作复杂、医生适用性差,无法满足实际临床的现实需求。 2.2 3D精准打印在骨科康复医学领域应用的关键 3D精准打印在骨科康复医学领域应用的关键是基于患者的CT或MRI医学图像[18-19],利用医学图像处理、个性化手术规划及植入物设计软件系统重建出与患者骨破损部位一致的3D模型;在此基础上设计术前模型、手术导板、个性化植入物、康复支具等个性化医疗器械;利用医学3D打印机对设计的产品进行增材制造,从而提高患者的治疗效果,其关键技术路径如图2所示。"
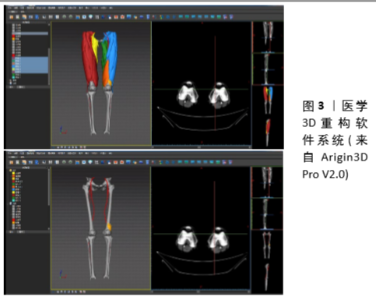
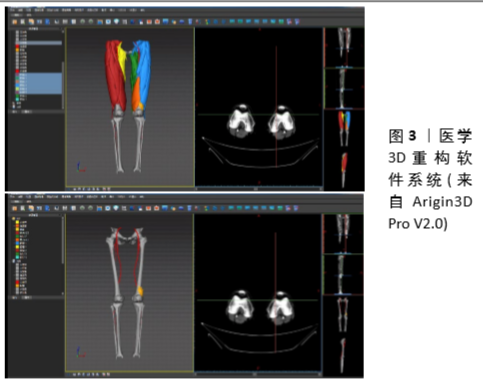
2.2.1 3D精准打印在骨科康复医学应用中的关键技术 医学图像处理与3D建模:医学影像开发可以实现2D切片和3D重建技术,如MRI和CT,提供了5种不同的3D重建技术:多层面重组、容积再现技术、最大密度投影、最小密度投影和表面阴影显示。全面支持裁剪、缩放、变焦、视角控制、透明度、灰度、投影、测量、标注。获取的MRI扫描图像可通过医学成像工具包(medical imaging tool kit,MITK)软件处理,直接读取MRI采集的医学数字成像及通信(digital imaging and communication of medicine,DICOM)数据,分割提取影像数据内的兴趣区域进行可视化,再计算生成并导出STL格式的三维网格模型[20-23]。利用曹桂平等[24]提及的Arigin3D Pro软件三维重建获得医学3D重构效果,见图3所示。 医生在与患者沟通的过程中,用个性化康复治疗3D打印数字设计技术软件重构的三维模型可视化地展示给患者观看,可显著提升医患沟通效率[25-28]。在此基础上,利用个性化康复治疗3D打印数字设计技术软件的移动客户端应用,将图像处理、模型重构等过程进行整合,可进一步简化医生的阅片过程[29-30]。"

个性化骨科康复手术模拟规划:基于患者三维模型的康复手术规划可用于指导医生制定骨科康复手术方案,软件系统应具有可视化、高精度的特点,可提供多种常规手术的手术规划流程[31-32]。同时,利用人工智能赋能3D精准打印可通过计算机来模拟医生的康复手术思维过程和智能行为,制造类似于医生人脑智能的云服务中心,辅助其他医生开展康复手术规划[33-35]。骨科康复术前规划与模拟涉及到复杂手术截骨、修复重建、骨穿刺的骨科手术中,医生往往面临确定截骨面以便于重建、修复,寻找穿刺入口,避免损伤周围神经、血管及精准穿刺肿瘤,确定截骨量和截骨部位等问题。实际操作中通过计算机辅助设计软件与3D打印技术[36-37],医生以DICOM格式将CT扫描数据导入3D辅助设计软件可获得骨折患处的精准三维模型,比起传统的X射线片、CT片、MRI图像更能辅助其了解患者立体解剖结构、准确诊断病情,确定手术方案。医生可从不同角度和方向观察骨折情况,再参照骨折AO治疗原则模拟选择合适手术入路,形成复位骨折模型,利用模型进行术前操作训练,也可用于向患者及其家属解释病情与手术方案,有利于医患沟通,减轻患者心理负担,实现个性化骨科康复手术模拟规划。利用曹桂平等[24]提及的Arigin3D Pro软件三维重建获得智能手术规划效果,如图4所示。 "

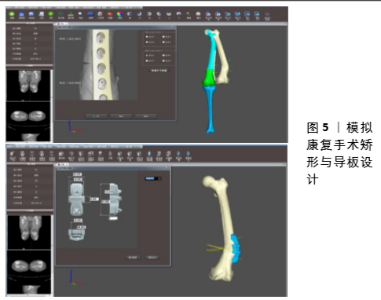
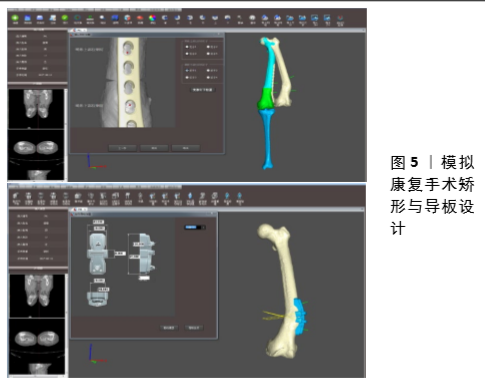
个性化骨科康复手术导板设计:手术导板基于三维重建和手术模拟,通过数字化设计并3D打印而成,帮助医生在术中实施精准手术,是精准外科手术的强有力工具。在使用自体骨重建缺损的手术中,将自体骨截取成合适重建的长度具有较大困难,过程繁琐且耗时[38]。利用个性化康复手术导板设计软件辅助可实现移植骨截骨导板为医生规划截骨线和截骨范围,辅助医生精准截取成多段骨块,减少磨骨操作,缩短手术时间,提高手术安全性。 在个性化骨科康复手术模拟规划中,骨科康复手术导板被认为是关键之一。由于人体解剖结构的复杂性,在传统的截骨、假体和螺钉植入手术中医生需要有多年临床经验,术中需反复进行透视以决定假体螺钉植入通道,容易造成手术时间过长和误操作等问题,同时大量X射线照射对于患者与医生均会产生伤害[39]。结合数字化设计和3D打印技术制作的个性化肩关节经皮导板,克服了传统肩关节穿刺过程中易出现的反复多次穿刺、无法穿刺到病变甚至引起肿瘤病变播散等弊端,基本实现了肩关节病变手术诊断与手术中的精准定位与穿刺。通过个性化骨科康复手术模拟规划,对患者行颈椎椎弓根螺钉内固定术前利用其CT数据三维建模,设计并模拟螺钉的最佳进钉通道,设计并3D打印定位导向孔的导向模板辅助手术,通过对术后效果的评估,肯定了数字导向模板在椎弓根螺钉固定的实用性和安全性[40]。利用曹桂平等[24]提及的Arigin3D Pro软件三维重建获得模拟康复手术矫形与导板设计效果,如图5所示。 那么,基于人工智能赋能的康复手术规划设定方案,利用软件自动参数化设计,使得个性化康复手术导板与人体骨骼实现高度匹配,生成个性化康复手术导板,可极大提高康复手术精度。"
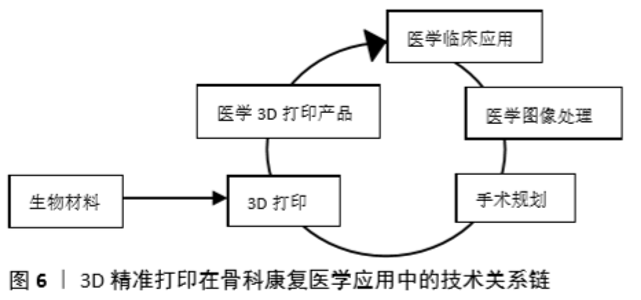
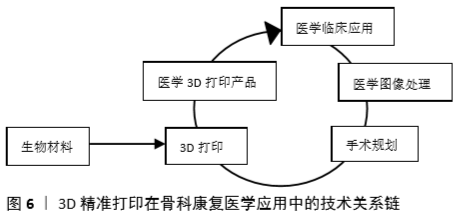
个性化骨科康复植入物设计:在现有临床案例中,考虑假体几何特征的个性化适配仅依靠医生个人的经验而进行,对于植入体本身的力学属性、生物学表现、植入假体与人体组织之间的关系和作用机制等并不明确,宿主与植入体之间的契合程度较差。个性化植入假体的个性适配不仅仅是几何尺寸或形态的简单适配,更多的是力学适配、生理适配,只有进一步考虑植入体与宿主组织相互作用的生物力学与力生物学适配,才能达到真正的生理功能适配[41]。另外,用于3D打印的材料包括聚合材料、金属材料、陶瓷材料等。常用的聚合物材料主要包括光敏树脂、热塑性塑料及水凝胶等。其中光敏树脂主要有自由基聚合的丙烯酸酯体系;热塑性塑料有最丙烯腈-丁二烯-苯乙烯塑料、聚乳酸、尼龙、聚碳酸酯、聚苯乙烯、聚己内酯、聚苯砜、热塑性聚氨酯、聚醚醚酮等[42-43];水凝胶主要有天然水凝胶与合成水凝胶。常用的金属材料包括钛、铝、钢、钴、镍、铜等。常用的陶瓷材料包括氧化铝陶瓷、磷酸三钙陶瓷、多孔氮化硅陶瓷等。 通过结合智能水凝胶技术及三维打印技术,快速设计并制备具有梯度结构的软骨修复康复植入物,从而实现骨缺损部位的自动识别与金属植入物三维模型的高效智能设计[44];构建由智能水凝胶、生物陶瓷、可降解聚合物组成的与软骨缺损部位性能匹配的一系列软骨修复植入物;明确影响三维结构孔隙尺寸及成型质量的关键工艺参数;实现3D打印植入物的生物修复效果。 3D精准打印装备研发及制造:根据用于康复医学骨修复材料的设计及性能要求[45],研发用于医学领域的3D打印装备,包括软骨修复材料的生物3D打印机喷头、个性化骨科手术中使用的手术器械及具有梯度结构的骨修复植入物,解决目前生物3D设计软件的自动化程度低、骨科医疗器械性能与缺损部位的匹配度低、植入物内部孔隙结构单一、细胞装载效果不理想等问题。3D精准打印在骨科康复医学应用中的技术关系链如图6所示。 常用3D打印机包括:熔融型3D打印机,采用丝状热塑性成形材料,连续地送入喷头后在其中加热熔融并挤出喷嘴,逐步堆积成形;光固化型3D打印机,采用激光一点点照射光固化液态树脂使之固化的方法成型;激光烧结型3D打印机,采用激光逐点烧结粉末材料,使包覆于粉末材料外的固体粘接剂或粉末材料本身熔融实现材料的粘接;激光熔化型3D打印机,利用金属粉末在激光束的热作用下完全熔化、经冷却凝固而成型。 2.2.2 3D精准打印技术浸入式骨科康复医学教学 基于医学3D建模数据建立3D精准打印技术浸入式骨科康复医学教学系统,在3D系统基础上升级VR交互显示系统,生成模拟手术场景,将各种模型数据添加到场景中,用户可通过佩戴VR头盔、借助VR手柄实现对模型的平移、旋转、缩放、复位等功能,进行实时交互操作和观察。通过3D精准打印技术浸入式康复医学教学系统,帮助用户可以掌握软件进行图像分割与重构操作、康复术前规划与个性化康复手术导板/康复植入物设计,实现系统软件与3D打印机的无缝对接,培养跨学科医工结合的人才,解决目前医疗器械研发速度慢、产品与患者实际不匹配等缺点。"
| [1] 李东阳,郝萱语.3D打印技术在临床医学中的应用进展[J].山东医药, 2015 (9):100-102. [2] NYBERG EL, FARRIS AL, HUNG BP, et al. 3D-Printing technologies for craniofacial rehabilitation, Reconstruction,and regeneration.Ann Biomed Eng.2017;45(1):45-57. [3] WEI YC, LIU J. 3D-printed transparent face-masks in the treatment of facial hypertrophic scars of young chil-dren with bums.Bums. 2017; 43(3):19-26. [4] 王忠宏,李扬帆,张曼茵.中国3D打印产业的现状及发展思路[J].经济纵横, 2013(1):90-93. [5] TEN KJ, SMIT G, BREEDVELD P. 3D-printed upper limb prostheses: a review. Disabil Rehabil Assist Technol.2017;12(3):300-314. [6] OLSZEWSKI R. Three-dimensional rapid prototyping models in cranio-maxillofacial surgery: systematic review and new clinical applications.P Belg Roy Acad Med.2013;11(2):43-77. [7] 王燎,戴克戎.骨科个体化治疗与3D打印技术[J].医用生物力学, 2014, 29(3):193-199. [8] WANG XJ, XU SQ, ZHOU S, et al. Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants:A review.Biomaterials. 2016;83:127-141. [9] 钟世镇.医用3D打印技术的探索[J].中华创伤骨科杂志, 2017, 19(2):138-139. [10] WIEDING J, WOLF A, BADER R. Numerical optimization of open-porous bone scaffold structures to match the elastic properties of human cortical bone.J Mech Behav Biomed.2014;37(37):56-68. [11] LUO Y, ZHAI D, HUAN Z, et al. Three-dimensional printing of hollow-struts-packed bioceramic scaffolds for bone regeneration.ACS Appl Mater Interacs.2015;7(43):24377-24383. [12] XU N, YE X, WEI D, et al. 3D artificial bones for bone repair prepared by computed tomography-guided fused deposition modeling for bone repair.ACS Appl Mater Interacs.2014;6(17):14952-14963. [13] COMPTON BG, LEWIS JA. 3D-printing of light weight cellular composites. Adv Mater. 2014;26(34):5930-5935. [14] FARZADI A, WARAN V, SOLATI-HASHJIN M, et al. Effect of layer printing delay on mechanical properties and dimensional accuracy of 3D printed porous prototypesin bone tissue engineering.Ceram Int. 2015; 41(7):8320-8330. [15] FERLIN KM, PRENDERGST ME, MILLER ML, et al. Influence of 3D printed porous architecture on mesenchymal stem cell enrichment and differentiation.Acta Mater.2016;32:161-169. [16] WU C, FAN W, ZHOU Y, et al. 3D-printing of highly uniform CaSiO3 ceramic scaffolds: preparation, characterization and in vivo osteogenesis. J Mater Chem.2012;22(24):12288-12295. [17] ZHANG Y, XIA L, ZHAI D, et al. Mesoporous bioactive glass nanolayer-functionalized 3D-printed scaffolds for accelerating osteogenesis and angiogenesis.Nanoscale.2015;7(45):19207-19221. [18] HWANG TJ, KIANG C, PAUL M. Surgical applications of 3-dimensional printing and precision medicine. JAMA Otolarygngol Head Neck Surg. 2015;141(4):305-306. [19] EBERT LC, THALI MJ, ROSS S. Getting in touch-3D printing in forensic imaging.Forensic Sci Int.2011;211(3):1-6. [20] AIALI AB, GRIFFIN MF, BUTLER PE. Three-dimensional printing surgical applications.Eplasty. 2015;15:e37. [21] IGAMI T, NAKAMURA Y, HIROSE T, et al. Application of a three-dimensional print of a liver in hepatectomy for small tumors invisible by intraoperative ultrasonography: preliminary experience. Word J Surg. 2014;38(12):3163-31666. [22] SCHMAUSS D, HAEBERLE S, HAGL C, et al. Three-dimensional printing in cardiac surgery and interventional cardiology: a single-center experience.Eur J Cardiothorac Surg.2015; 47(6): 1044-1052. [23] BAGARIA V, DESHPANDE S, RASALKAR DD, et al. Use of rapid prototyping and three-dimensional reconslruetion modeling in the management of complex fractures.Eur J Radiol.2011;80(3):814-820. [24] 曹桂平,张明娇,刘非,等.Arigin 3D Pro软件与Mimics软件三维重建模型的精度研究[J].中国组织工程研究,2018,22(15):2384-2389. [25] PARTRIDGE R, CONHSK N, DAVIES JA. In-lab three-dimensional printing: an inexpensive tool for experimentation and visualization for the field of organogenesis.Organogenesis.2012;8(1): 22-27. [26] MULFORD JS, BABAZADEH S, MACKAY N. Three dimensional printing in orthopaedic surgery:A review of current and future applications. ANZ J Surg.2016;86(9):648-653. [27] JANG J, PARK JY, GAO G, et al. Biomaterials-based 3D cell printing for next-generation therapeutics and diagnostics.Biomaterials. 2017; 156: 88-106. [28] ELTORAI AE, NGUYEN E, DANIELS AH. Three-dimensional printing in orthopedic surgery. Orthopedics. 2015;38(11):684-687. [29] XIAO J, HUANG W, YANG X, et al. En bloc resection of primary malignant bone tumor in the cervical spine based on 3-dimensional printing technology. Orthop Surg.2016;8(2):171-178. [30] MOBBS RJ, COUGHLAN M, THOMPSON R, et al. The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: case report.J Neurosurg Spine. 2017; 26(4): 513-518. [31] NYBERG EL, FARRIS AL, HUNG BP, et al. 3D-Printing Technologies for Craniofacial Rehabilitation, Reconstruction, and Regeneration.Ann Biomed Eng.2017;45(1):45-57. [32] TEN KATE J, SMIT G, BREEDVELD P. 3D-printed upper limb prostheses: a review. Disabil Rehabil Assist Technol. 2017;12(3): 300-314. [33] CHA YH, LEE KH, RYU HJ, et al. Ankle-Foot Orthosis Made by 3D Printing Technique and Automated Design Software.Appl Bionics Biomech. 2017;2017:9610468. [34] LI C, YANG M, XIE Y, et al. Application of the polystyrene model made by 3D printing rapid prototyping technology for operation planning in revision lumbar discectomy.J Orthop Sci. 2015;20(3):475-480. [35] ACKLAND DC, ROBINSON D, REDHEAD M, et al. A personalized 3D-printed prosthetic joint replacement for the human temporomandibular joint: from implant design to implantation.J Mech Behav Biomed Mater.2017;69:404-411. [36] ZERR J, CHATZINOFF Y, CHOPRA R, et al. Three-dimensional printing for preoperative planning of total hip arthroplasty revision: case report.Skeletal Radiol.2016;45(10):1431-1435. [37] HAMID KS, PAREKH SG, ADAMS SB. Salvage of severe foot and ankle trauma with a 3D printed scaffold. Foot Ankle Int.2016;37(4):433-439. [38] GALL M, XING LI, XIAOJUN CHEN, et al. Computer-aided planning and reconstruction of cranial 3D implants. Conf Proc IEEE Eng Med Biol Soc.2016:1179-1183. [39] HUANG YH, SEELAUS R, ZHAO L, et al. Virtual surgical planning and 3D printing in prosthetic orbital reconstruction with percutaneous implants: a technical case report.Int Med Case Rep J. 2016;9:341-345. [40] DEKKER TJ, STEELE JR, FEDERER AE, et al. Use of patient-specific 3D-printed titanium implants for complex foot and ankle limb salvage, deformity correction and arthrodesis procedures.Foot Ankle Int. 2018; 8: 916-921. [41] WANG B, HAO Y, PU F, et al. Computer-aided designed, three dimensional-printed hemipelvic prosthesis for periacetabular malignant bone tumour.Int Orthop.2018;3:687-694. [42] 何岷洪,宋坤,莫宏斌,等.3D打印光敏树脂的研究进展[J].功能高分子学报, 2015,28(1):102-108. [43] 罗文峰,杨雪香,敖宁建.生物医用材料的3D打印技术与发展[J].材料导报, 2016,30(13):81-86. [44] 张常贵,杨柳,段小军.3D打印技术在关节外科的临床应用进展[J].中国矫形外科杂志,2019,27(16):1497-1501. [45] 史建峰,王涵,王迎,等.3D生物打印技术的发展与应用[J].医疗装备, 2017, 30(17):202-204. [46] SUMMIT S. “Additive manufacturing of a prosthetic limb”, rapid prototyping of biomaterials, principles and applications. Series: Wood Head Publishing Serieson Biomaterials.2014:285-296. [47] MA H, LUO J, SUN Z, et al. 3D printing of biomaterials with mussel-inspired nanostructures for tumor therapy and tissue regeneration.Biomaterials. 2016;111:138-148. [48] BILLIET T, VANDENHAUTE M, SCHELFHOUT J, et al. A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials. 2012;33(26):6020-6041. [49] GERMANY EI, PINO EJ, AQUEVEQUE PE. Myoelectric intuitive control and transcutaneous electrical stimulation ofthe forearm for vibrotactile sensation feedback applied to a 3D printed prosthetic hand.ConfProc IEEE Eng Med Biol Soc.2016;2016:5046-5050. [50] 刘非,邱冰,薛向东,等.基于3D打印技术的个性化外固定支具设计[J].中国矫形外科杂志,2016,24(24):2260-2263. [51] SING SL, AN J, YEONG WY, et al. Laser and electron-beam powder-bed additive manufacturing of metallic implants: A review on processes, materials and designs. J Orthop Res.2016;34(3):369-385. [52] VENTOLA CL. Medical applications for 3d printing: current and projected uses. Phys Ther. 2014;39(10):704-711. [53] WON SH, LEE YK, HA YC, et al. Improving pre-operative planning for complex total hip replacement with a Rapid Prototype model enabling surgical simulation.Bone Joint J.2013;95B(11):1458-1463. [54] 苏宏伦,李剑,莫中军,等.个性化植入假体—骨修复、骨置换的未来趋势[J].中国医疗器械信息,2017,23(7):19-22. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [3] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [4] | Lu Dezhi, Mei Zhao, Li Xianglei, Wang Caiping, Sun Xin, Wang Xiaowen, Wang Jinwu. Digital design and effect evaluation of three-dimensional printing scoliosis orthosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1329-1334. |
| [5] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [6] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [7] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [8] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [9] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [10] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [11] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [12] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [13] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [14] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [15] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||