Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (19): 3044-3055.doi: 10.3969/j.issn.2095-4344.2017.19.015
Previous Articles Next Articles
Age-related changes in condyle evaluated by cone-beam CT reconstruction
Li Xin1, Tang Jing2, Li Ze-kui1, Li Hong-fa1, Liang Meng3, Zhang Juan1
- 1Hospital of Stomatology, Tianjin Medical University, Tianjin 300070, China; 2Rytime Dental Hospital, Beijing 100107, China; 3School of Medical Imaging, Tianjin Medical University, Tianjin 300203, China
-
Online:2017-07-08Published:2017-08-10 -
Contact:Zhang Juan, M.D., Associate chief physician, Hospital of Stomatology, Tianjin Medical University, Tianjin 300070, China -
About author:Li Xin, Studying for master’s degree, Hospital of Stomatology, Tianjin Medical University, Tianjin 300070, China -
Supported by:the Teaching Research Foundation of Stomatological School of Tianjin Medical University, No. kqjg201504; the Basic Application and High-Tech Research Program of Tianjin, No. 15JCBYJC55100
CLC Number:
Cite this article
Li Xin, Tang Jing, Li Ze-kui, Li Hong-fa, Liang Meng, Zhang Juan. Age-related changes in condyle evaluated by cone-beam CT reconstruction[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(19): 3044-3055.
share this article

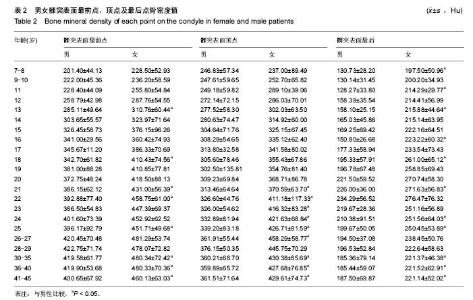
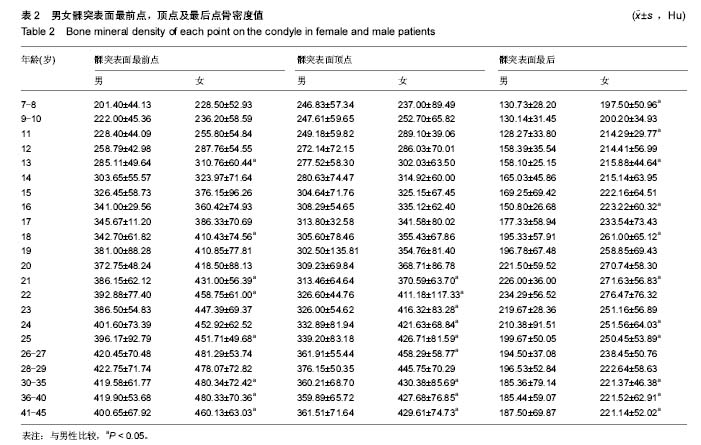
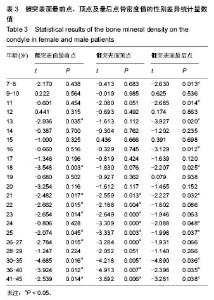
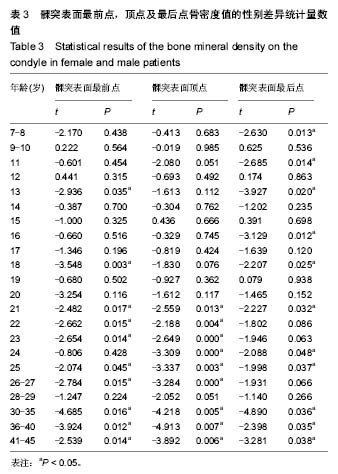
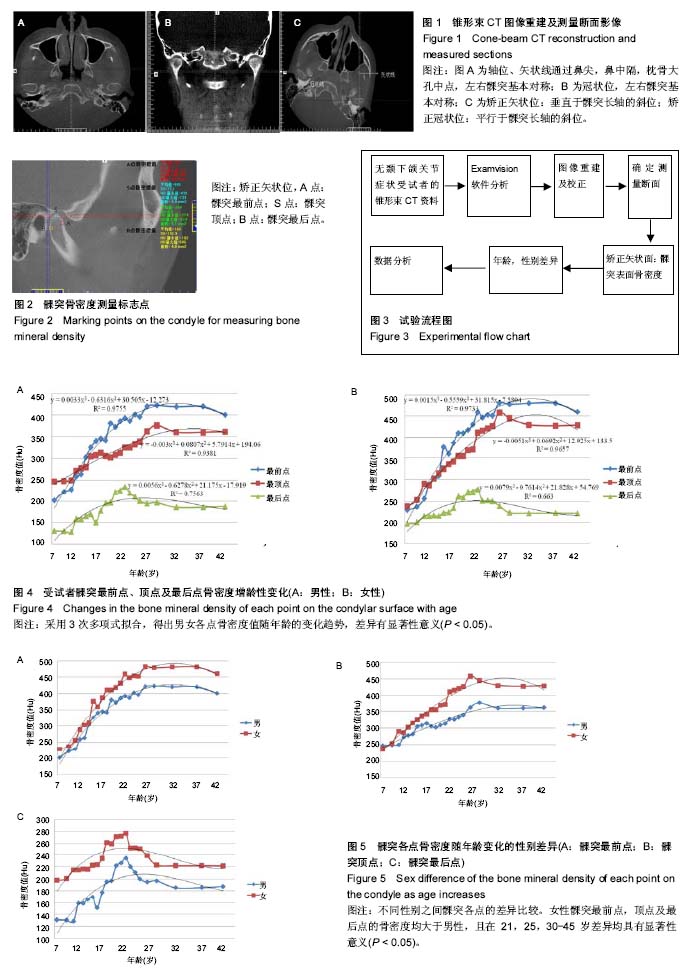
2.1 受试者数量分析 纳入对象为883例无颞下颌关节症状患者的锥形束CT影像资料,均进入结果分析。试验流程图见图3。 2.2 男、女髁突各点骨密度随年龄变化趋势 男女髁突表面最前点,顶点及最后点骨密度值见表2及图4。男女患者髁突最前点及顶点骨密度随年龄增长不断增高,达到高峰期后基本保持稳定,40岁后出现下降趋势;女性患者达到高峰期年龄早于男性:女性26-27岁,男性28-29岁。男女患者髁突最后点骨密度均在22岁时达到高峰后继而下降,30岁后保持基本稳定。 男女受试者髁突各点骨密度表现出相似的趋势:髁突最前点,顶点的骨密度变化拟合曲线于12岁有“交叉”,“交叉”之前,髁突顶点骨密度高于最前点,此后,髁突最前点骨密度均高于顶点。各年龄段髁突最前点,顶点骨密度均大于最后点。 2.3 髁突表面各点骨密度值性别差异 女性受试者髁突最前点、顶点及最后点的骨密度均大于男性,且在21,25,30-45岁差异均有显著性意义(P < 0.05),见表3及图5。"
| [1] Gomes LR, Gomes M, Jung B, et al. Diagnostic index of three-dimensional osteoarthritic changes in temporomandibular joint condylar morphology. J Med Imaging (Bellingham). 2015;2(3):034501.[2] Comert Kilic S, Kilic N, Sumbullu MA. Temporomandibular joint osteoarthritis: cone beam computed tomography findings, clinical features, and correlations. Int J Oral Maxillofac Surg. 2015,44(10):1268-1274.[3] de Sousa ST, de Mello VV, Magalhaes BG, et al. The role of occlusal factors on the occurrence of temporomandibular disorders. Cranio. 2015;33(3):211-216.[4] Silvola AS, Tolvanen M, Rusanen J, et al. Do changes in oral health-related quality-of-life, facial pain and temporomandibular disorders correlate after treatment of severe malocclusion? Acta Odontol Scand. 2016;74(1):44-50.[5] Peltola JS, Kononen M, Nystrom M. A follow-up study of radiographic findings in the mandibular condyles of orthodontically treated patients and associations with TMD. J Dent Res. 1995;74(9):1571-1576.[6] Talic NF. Adverse effects of orthodontic treatment: a clinical perspective. Saudi Dent J. 2011;23(2):55-59.[7] Barngkgei I, Al Haffar I, Khattab R. Osteoporosis prediction from the mandible using cone-beam computed tomography. Imaging Sci Dent. 2014;44(4):263-271.[8] Kazuo L, Koji H. Estimation of effective dose from limited cone beam X-ray CT examination. Dent Radiol. 2000;40:251-259.[9] 徐子卿,冯静.口腔颌面部锥形束CT线距测量准确性和可靠性的评价[J].国际口腔科学杂志,2012,39(4):557-560.[10] 傅开元,张万林,柳登高,等.应用锥形束CT诊断颞下颌关节骨关节病的探讨[J].中华口腔医学杂志,2007,42(7):417-420.[11] Talaat W, Al Bayatti S, Al Kawas S. CBCT analysis of bony changes associated with temporomandibular disorders. Cranio. 2016;34(2):88-94.[12] Alexiou K, Stamatakis H, Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography. Dentomaxillofac Radiol. 2009;38(3):141-147.[13] 秦林林,马海波,张卫,等.中国北方汉族健康人骨密度正常值[J].中国骨质疏松杂志,2002,8(2):110-111.[14] 吴玉洁,赵方,靖涛.辽宁地区正常成年人不同部位骨密度测量分析[J].中国骨质疏松杂志,2008,14(6):422-424.[15] Lei J, Han J, Liu M, et al. Degenerative temporomandibular joint changes associated with recent-onset disc displacement without reduction in adolescents and young adults. J Craniomaxillofac Surg. 2017. doi: 10.1016/j.jcms.2016.12.017.[16] Carrasco R. Juvenile idiopathic arthritis overview and involvement of the temporomandibular joint: prevalence, systemic therapy. Oral Maxillofac Surg Clin North Am. 2015;27(1):1-10.[17] Nah KS. Condylar bony changes in patients with temporomandibular disorders: a CBCT study. Imaging Sci Dent. 2012;42(4):249-253.[18] dos Anjos Pontual ML, Freire JS, Barbosa JM, et al. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac Radiol. 2012;41(1):24-29.[19] Pasqualini L, Leli C, Ministrini S, et al. Relationships between global physical activity and bone mineral density in a group of male and female students. J Sports Med Phys Fitness. 2017; 57(3):238-243.[20] Stagi S, Cavalli L, Iurato C, et al. Bone metabolism in children and adolescents: main characteristics of the determinants of peak bone mass. Clin Cases Miner Bone Metab. 2013;10(3): 172-179.[21] Sidebottom AJ. Alloplastic or autogenous reconstruction of the TMJ. J Oral Biol Craniofac Res. 2013;3(3):135-139.[22] Chalhoub D, Orwoll ES, Cawthon PM, et al. Areal and volumetric bone mineral density and risk of multiple types of fracture in older men. Bone. 2016;92:100-106.[23] Paknahad M, Shahidi S, Iranpour S, et al. Cone-beam computed tomographic assessment of mandibular condylar position in patients with temporomandibular joint dysfunction and in healthy subjects. Int J Dent. 2015;2015:301796.[24] Solberg WK, Hansson TL, Nordstrom B. The temporomandibular joint in young adults at autopsy: a morphologic classification and evaluation. J Oral Rehabil. 1985;12(4):303-321.[25] Drozdzowska B, Pluskiewicz W. Longitudinal changes in mandibular bone mineral density compared with hip bone mineral density and quantitative ultrasound at calcaneus and hand phalanges. Br J Radiol. 2002;75(897):743-747.[26] 张林,杨锡让.人体骨量变化研究发展[J].体育与科学, 1999, 20(2):7-10.[27] Pluskiewicz W, Tarnawska B, Drozdzowska B. Mandibular bone mineral density measured using dual-energy X-ray absorptiometry: relationship to hip bone mineral density and quantitative ultrasound at calcaneus and hand phalanges. Br J Radiol. 2000;73(867):288-292.[28] Stagi S, Cavalli L, Cavalli T, et al. Peripheral quantitative computed tomography (pQCT) for the assessment of bone strength in most of bone affecting conditions in developmental age: a review. Ital J Pediatr. 2016;42(1):88.[29] Ilguy D, Ilguy M, Fisekcioglu E, et al. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. Scientific World J. 2014;2014: 761714.[30] Ballabriga A. Morphological and physiological changes during growth: an update. Eur J Clin Nutr. 2000;54 Suppl 1:S1-S6.[31] Lei J, Liu MQ, Yap AU, et al. Condylar subchondral formation of cortical bone in adolescents and young adults. Br J Oral Maxillofac Surg. 2013;51(1):63-68.[32] Imanimoghaddam M, Madani AS, Hashemi EM. The evaluation of lateral pterygoid muscle pathologic changes and insertion patterns in temporomandibular joints with or without disc displacement using magnetic resonance imaging. Int J Oral Maxillofac Surg. 2013;42(9):1116-1120.[33] Juran CM, Dolwick MF, McFetridge PS. Shear mechanics of the TMJ disc: relationship to common clinical observations. J Dent Res. 2013;92(2):193-198.[34] de Farias JF, Melo SL, Bento PM, et al. Correlation between temporomandibular joint morphology and disc displacement by MRI. Dentomaxillofac Radiol. 2015;44(7):20150023.[35] Utreja A, Dyment NA, Yadav S, et al. Cell and matrix response of temporomandibular cartilage to mechanical loading. Osteoarthritis Cartilage. 2016;24(2):335-344.[36] Kim DG, Jeong YH, Kosel E, et al. Regional variation of bone tissue properties at the human mandibular condyle. Bone. 2015;77:98-106.[37] Southard KA, Southard TE, Schlechte JA, et al. The relationship between the density of the alveolar processes and that of post-cranial bone. J Dent Res. 2000;79(4):964-969.[38] Brotto M, Bonewald L. Bone and muscle: Interactions beyond mechanical. Bone. 2015,80:109-114.[39] Nickel JC, McLachlan KR, Smith DM. A theoretical model of loading and eminence development of the postnatal human temporomandibular joint. J Dent Res. 1988;67(6):903-910.[40] 王世平,陈新明,杜昌连,等.39例髁突骨密度的测量[J].中华口腔医学杂志,1995,30(4):218-219.[41] 秦林林,陈金标,葛崇华,等.781例15-50岁健康者骨密度与影响因素分析[J].中华预防医学杂志,1999,33(5):282-285.[42] Abrahamsen B, Brask-Lindemann D, Rubin KH, et al. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. Bonekey Rep. 2014;3:574.[43] 任荣,李凌伟,郭启发.骨水泥型股骨柄人工股骨头置换治疗老年骨质疏松股骨颈骨折的可行性:随机对照临床试验方案[J].中国组织工程研究,2016,20(48):7261-7266. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||