Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (35): 7544-7551.doi: 10.12307/2025.955
Previous Articles Next Articles
Correlation of echocardiographic parameters with disability at 3 months after acute ischemic stroke
Yang Bo, Pan Xinfang, Chang Liuhui, Ni Yong
- Department of Anesthesiology, The Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China
-
Received:2024-10-22Accepted:2024-12-23Online:2025-12-18Published:2025-04-30 -
Contact:Ni Yong, MD, Associate chief physician, Department of Anesthesiology, The Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China -
About author:Yang Bo, MD, Attending physician, Department of Anesthesiology, The Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China -
Supported by:National Natural Science Foundation of China, No. 81601147 (to YB); Suzhou Heath Young Key Talents "National Tutorial System" Training Project, No. Qngg2024006 (to YB); Suzhou Applied Basic Research (Healthcare) Science and Technology Innovation Youth Project, No. SYW2024082 (to YB)
CLC Number:
Cite this article
Yang Bo, Pan Xinfang, Chang Liuhui, Ni Yong. Correlation of echocardiographic parameters with disability at 3 months after acute ischemic stroke[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7544-7551.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
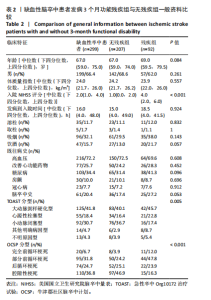
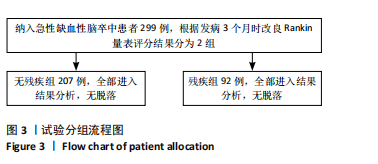
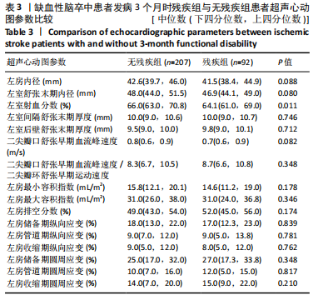
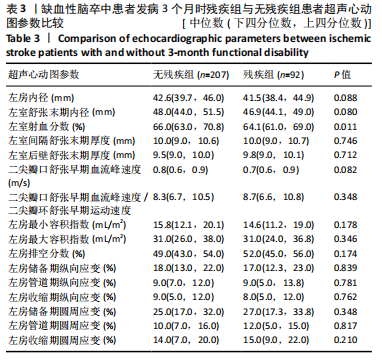
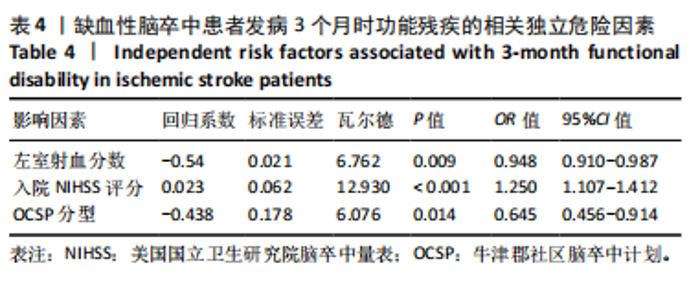
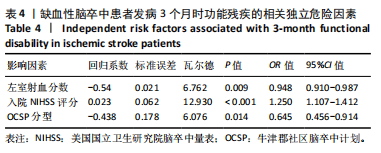
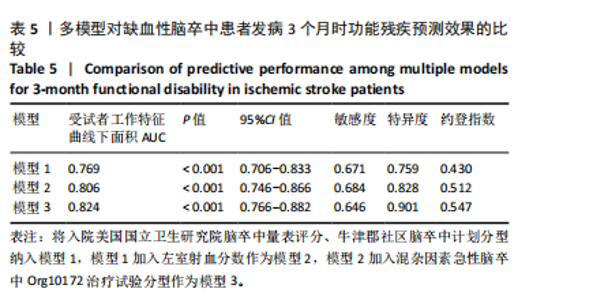
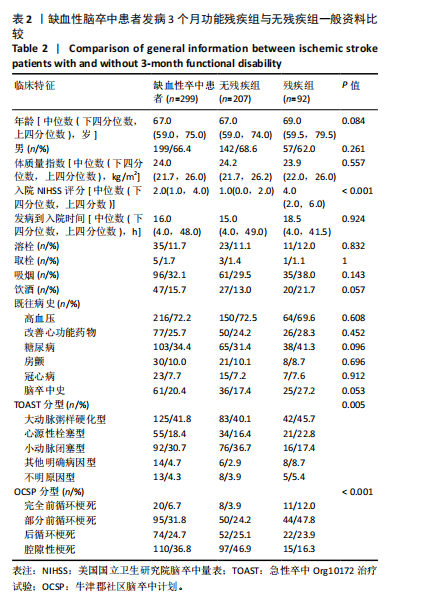
2.3 无残疾组与残疾组患者基线资料比较 299例急性缺血性脑卒中患者年龄中位数为67岁,女性100例,男性199例,体质量指数中位数为24.0 kg/m2,入院NIHSS评分中位数为2分,发病到入院时间中位数为16 h;入院时溶栓者35例,取栓者(包括桥接治疗)5例;既往吸烟者96例,饮酒者47例;合并高血压病者216例,口服改善心功能药物者77例,糖尿病者103例,房颤者30例,冠心病者23例,有脑卒中史者61例(20.4%);TOAST分型中大动脉粥样硬化型125例,心源性栓塞型55例,小动脉闭塞型92例,其他明确病因型14例,不明原因型13例;OCSP分型中完全前循环梗死20例,部分前循环梗死95例,后循环梗死74例,腔隙性梗死110例。 发病3个月时残疾患者有92例(30.8%),无残疾者207例(69.2%)。比较两组的基线特征发现,两组人口统计学资料(年龄、性别)、体质量指数、发病到入院时间、特殊治疗方式(是否行静脉溶栓、机械取栓)、个人史(吸烟、饮酒史)、既往病史及用药史(高血压病、改善心功能药物服用情况、糖尿病、房颤、冠心病、脑卒中史)比较差异均无显著性意义(P > 0.05),残疾组患者入院NIHSS评分更高(4.0分vs. 1.0分,P < 0.001),TOAST分型中小动脉闭塞型占比低(17.4% vs. 36.7%,P=0.005),OCSP分型中后循环梗死(23.9% vs. 25.1%)和腔隙性梗死(16.3% vs. 46.9%)占比更低(P < 0.001),见表2。"
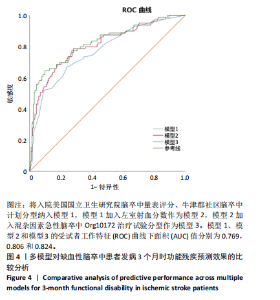
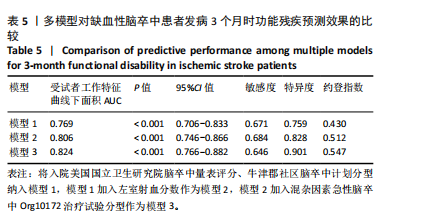
2.4.3 缺血性脑卒中患者发病3个月时功能残疾的ROC曲线分析 根据表2-4结果,脑卒中患者发病3个月时残疾的独立影响因素为左室射血分数、入院NIHSS评分、OCSP分型,混杂因素为TOAST分型。将入院NIHSS评分、OCSP分型纳入模型1,模型1加入左室射血分数作为模型2,模型2加入混杂因素作为模型3,使用ROC曲线分析3个模型对患者发病3个月时残疾的预测效果。 模型1、模型2、模型3的ROC曲线下面积AUC分别为0.769,0.806,0.824,AUC值的提升提示了左室射血分数在脑卒中患者预后评估中的重要性,模型2与模型3的ROC曲线下面积AUC变化虽小,但进一步说明校正混杂因素后左室射血分数对预测模型的独立贡献仍然存在且作用稳定,见图4,表5。表明在实际临床工作中,"
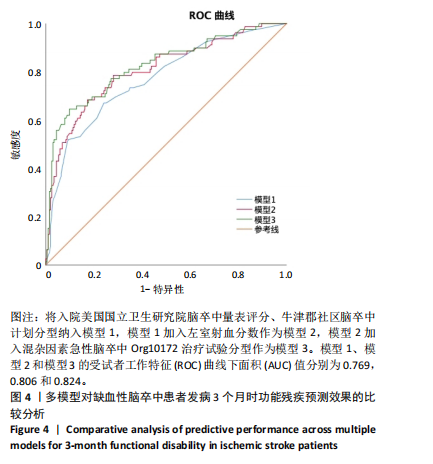
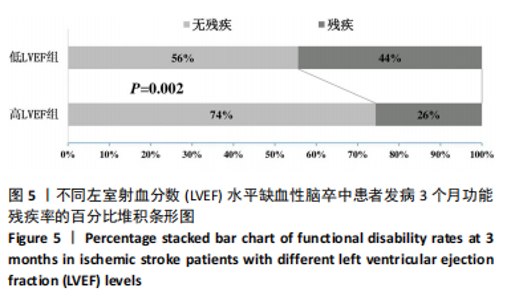
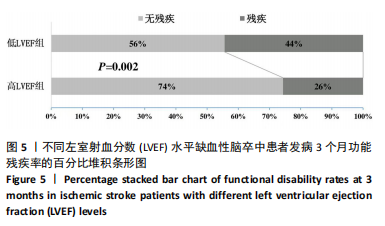
通过常规超声心动图测量左室射血分数,不仅可用于判断心功能状态,还可为脑卒中患者的个体化风险分层提供可靠依据。随着左室射血分数的加入,模型的敏感度和特异度均有所优化,这提示结合左室射血分数的预测模型能够更精准地筛选出高风险患者,同时减少低风险患者的误分类,从而在临床实践中具备更高的适用性。因此,模型预测效果的逐步提升表明,在以入院NIHSS评分和OCSP分型为基础的预测模型中加入左室射血分数,不仅可以改善模型的预测性能,还能通过敏感度和特异度的优化实现更高效的风险分层。未来应进一步探讨如何将左室射血分数与其他心脏功能指标联合应用以构建更全面的脑卒中预后评估工具,从而指导个体化治疗决策。 2.4.4 不同左室射血分数水平缺血性脑卒中患者发病3个月时功能残疾率的比较 根据左室射血分数与脑卒中患者发病3个月时残疾的ROC曲线,得到左室射血分数的最佳切点为60.25%,据此将299例患者分为低左室射血分数组(左室射血分数≤60.25%)和高左室射血分数组(左室射血分数> 60.25%),比较两组间发病3个月残疾率并绘制百分比堆积条形图,低左室射血分数组患者发病3个月时的残疾率高于高左室射血分数组(44% vs. 26%,P=0.002),见图5。"
| [1] FEIGIN VL, BRAININ M, NORRVING B, et al. World stroke organization (wso): Global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18-29. [2] KE C, SHI W, ZHOU Z, et al. Overview of evidence-based research on acupuncture for stroke treatment using magnetic resonance imaging technology. Front Neurosci. 2024;18:1495435. [3] Hernandez-Jimenez M, Abad-Santos F, Cotgreave I, et al. Safety and efficacy of aptoll in patients with ischemic stroke undergoing endovascular treatment: A phase 1/2 randomized clinical trial. JAMA Neurol. 2023;80(8):779-788. [4] MA R, SUN X, LIU Z, et al. Ferroptosis in ischemic stroke and related traditional chinese medicines. Molecules. 2024;29(18):4359. [5] CHEN J, LI X, HU R, et al. The clinical value of fibrosis indices for predicting the hemorrhagic transformation in patients with acute ischemic stroke after intravenous thrombolysis. Front Aging Neurosci. 2024;16:1492410. [6] MIKI K, NAKANO M, AIZAWA K, et al. Risk factors and localization of silent cerebral infarction in patients with atrial fibrillation. Heart Rhythm. 2019;16(9):1305-1313. [7] KELLEY RE, KELLEY BP. Heart-brain relationship in stroke. Biomedicines. 2021;9(12):1835. [8] EDWARDS JD, HEALEY JS, FANG J, et al. Atrial cardiopathy in the absence of atrial fibrillation increases risk of ischemic stroke, incident atrial fibrillation, and mortality and improves stroke risk prediction. J Am Heart Assoc. 2020;9(11):e013227. [9] PARK HK, KIM BJ, YOON CH, et al. Left ventricular diastolic dysfunction in ischemic stroke: Functional and vascular outcomes. J Stroke. 2016; 18:195-202. [10] RYU WS, PARK JB, KO SB, et al. Diastolic dysfunction and outcome in acute ischemic stroke. Cerebrovasc Dis. 2016;41(3-4):148-155. [11] MANNINA C, ITO K, JIN Z, et al. Association of left atrial strain with ischemic stroke risk in older adults. JAMA Cardiol. 2023;8:317-325. [12] OBOKATA M, NEGISHI K, KUROSAWA K, et al. Left atrial strain provides incremental value for embolism risk stratification over cha(2)ds(2)-vasc score and indicates prognostic impact in patients with atrial fibrillation. J Am Soc Echocardiogr. 2014;27(7):709-716. e4. [13] ZINGALES V, ESPOSITO MR, QUAGLIATA M, et al. Comparative study of spheroids (3d) and monolayer cultures (2d) for the in vitro assessment of cytotoxicity induced by the mycotoxins sterigmatocystin, ochratoxin a and patulin. Foods. 2024;13(4):564. [14] WU T, GONG L, ZHANG C, et al. Three-dimensional echocardiography and strain cardiac imaging in patients with prediabetes and type 2 diabetes mellitus. Quant Imaging Med Surg. 2023;13(12):7753-7764. [15] BRAND A, FRUMKIN D, HUBSCHER A, et al. Phasic left atrial strain analysis to discriminate cardiac amyloidosis in patients with unclear thick heart pathology. Eur Heart J Cardiovasc Imaging. 2021;22(6):680-687.
[16] MARCHESE P, SCALESE M, GIORDANO R, et al. Pediatric ranges of normality for 2d speckle-tracking echocardiography atrial strain: Differences between p- and r-gating and among new (atrial designed) and conventional (ventricular specific) software’s. Echocardiography. 2021;38(12):2025-2031. [17] REDDIN C, CANAVAN M, HANKEY GJ, et al. Association of vascular risk with severe vs non-severe stroke: An analysis of the interstroke study. Neurology. 2024;103:e210087. [18] SALIM HA, LAKHANI DA, MEI J, et al. Prolonged venous transit is associated with lower odds of excellent recovery after reperfusion in anterior large-vessel occlusion stroke. Eur J Neurol. 2025;32(1):e16563. [19] ZEDDE M, LATTANZI S, PILOTTO A, et al. Premorbid frailty, stress hyperglycemia ratio, and functional outcome in patients with acute ischemic stroke. Front Neurol. 2024;15:1463814. [20] 中国卒中学会,中国卒中学会神经介入分会,中华预防医学会卒中预防与控制专业委员会介入学组.急性缺血性卒中血管内治疗中国指南 2018[J].中国卒中杂志,2018,13(7):706-729. [21] Correction to: Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2019;50:e440-e441. [22] WOLF PA, ABBOTT RD, KANNEL WB. Atrial fibrillation as an independent risk factor for stroke: The framingham study. Stroke. 1991;22:983-988. [23] VIRK HUH, ESCOBAR J, RODRIGUEZ M, et al. Dual antiplatelet therapy: A concise review for clinicians. Life (Basel). 2023;13(7):1580. [24] SCHEITZ JF, SPOSATO LA, SCHULZ-MENGER J, et al. Stroke-heart syndrome: Recent advances and challenges. J Am Heart Assoc. 2022; 11:e026528. [25] QU Y, SUN YY, ABUDUXUKUER R, et al. Heart rate variability parameter changes in patients with acute ischemic stroke undergoing intravenous thrombolysis. J Am Heart Assoc. 2023;12:e028778. [26] BALINT B, JAREMEK V, THORBURN V, et al. Left atrial microvascular endothelial dysfunction, myocardial inflammation and fibrosis after selective insular cortex ischemic stroke. Int J Cardiol. 2019;292:148-155. [27] SIMATS A, ZHANG S, MESSERER D, et al. Innate immune memory after brain injury drives inflammatory cardiac dysfunction. Cell. 2024;187: 4637-4655.e26. [28] JINAWONG K, APAIJAI N, CHATTIPAKORN N, et al. Cognitive impairment in myocardial infarction and heart failure. Acta Physiol (Oxf). 2021;232: e13642. [29] HJALMARSSON C, FU M, ZVERKOVA SANDSTROM T, et al. Risk of stroke in patients with heart failure and sinus rhythm: Data from the swedish heart failure registry. ESC Heart Fail. 2021;8(1):85-94. [30] SHOURAV MMI, GODASI RR, ANISETTI B, et al. Association between heart failure and cerebral collateral flow in large vessel occlusive ischemic stroke. J Stroke Cerebrovasc Dis. 2024;33(11):107999. [31] NAKAO K, DAFAALLA M, NAKAO YM, et al. Comparison of care and outcomes for myocardial infarction by heart failure status between united kingdom and japan. ESC Heart Fail. 2023;10:1372-1384. [32] CHETAN IM, GERGELY-DOMOKOS B, BEYER R, et al. The role of 3d speckle tracking echocardiography in the diagnosis of obstructive sleep apnea and its severity. Sci Rep. 2022;12:22347. [33] PARSOVA KE, KELES N, KARATAS M, et al. Assessment of right ventricular sequelae by speckle tracking echocardiography in recovered covid-19 patients. Acta Cardiol. 2024;79:909-914. [34] WANG C, XING J, ZHAO B, et al. The effects of high-intensity interval training on exercise capacity and prognosis in heart failure and coronary artery disease: A systematic review and meta-analysis. Cardiovasc Ther. 2022;2022:4273809. [35] DOCHERTY KF, HENDERSON AD, JHUND PS, et al. Efficacy and safety of finerenone across the ejection fraction spectrum in heart failure with mildly reduced and preserved ejection fraction: A prespecified analysis of the finearts-hf trial. Circulation. 2024. doi: 10.1161/CIRCULATIONAHA.124.072011. [36] RADAKRISHNAN A, DOKKO J, PASTENA P, et al. Thromboembolism in peripartum cardiomyopathy: A systematic review. J Thorac Dis. 2024;16:645-660. [37] KANG JB, SON HK, SHAH MA, et al. Retinoic acid attenuates ischemic injury-induced activation of glial cells and inflammatory factors in a rat stroke model. PLoS One. 2024;19:e0300072. [38] VENKAT P, CUI C, CHEN Z, et al. Cd133+exosome treatment improves cardiac function after stroke in type 2 diabetic mice. Transl Stroke Res. 2021;12:112-124. [39] KWON HM, PARK JH, KIM JM, et al. Mild left ventricular dysfunction is associated with thrombogenicity in cardioembolic stroke. Eur Neurol. 2006;56:217-221. [40] SCHAFER A, FLIERL U, BAUERSACHS J. Anticoagulants for stroke prevention in heart failure with reduced ejection fraction. Clin Res Cardiol. 2022;111(1):1-13. [41] HERMANNS N, WROBLEWSKI V, BASCUNANA P, et al. Molecular imaging of the brain-heart axis provides insights into cardiac dysfunction after cerebral ischemia. Basic Res Cardiol. 2022;117(1):52. [42] LIND L, LOADER J, LINDAHL B, et al. A comparison of echocardiographic and circulating cardiac biomarkers for predicting incident cardiovascular disease. PLoS One. 2022;17:e0271835. [43] SUNG PH, CHEN KH, LIN HS, et al. The correlation between severity of neurological impairment and left ventricular function in patients after acute ischemic stroke. J Clin Med. 2019;8(2):190. [44] ROJEK A, GASECKI D, FIJALKOWSKI M, et al. Left ventricular ejection fraction and aortic stiffness are independent predictors of neurological outcome in acute ischemic stroke. J Hypertens. 2016;34:2441-2448. |
| [1] | Li Chen, Liu Ye, Ni Xindi, Zhang Yuang. Simulation analysis of real-time continuous stiffness in muscle fibers and tendons of the triceps surae during multi-joint movement [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7529-7536. |
| [2] | Liu Xuan, Ding Yuqing, Xia Ruohan, Wang Xianwang, Hu Shujuan. Exercise prevention and treatment of insulin resistance: role and molecular mechanism of Keap1/nuclear factor erythroid2-related factor 2 signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7578-7588. |
| [3] | Gong Yuehong, Wang Mengjun, Ren Hang, Zheng Hui, Sun Jiajia, Liu Junpeng, Zhang Fei, Yang Jianhua, Hu Junping. Machine learning combined with bioinformatics screening of key genes for pulmonary fibrosis associated with cellular autophagy and experimental validation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7679-7689. |
| [4] | Han Jie, Pan Chengzhen, Shang Yuzhi, Zhang Chi. Identification of immunodiagnostic biomarkers and drug screening for steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7690-7700. |
| [5] | Fang Yuan, Qian Zhiyong, He Yuanhada, Wang Haiyan, Sha Lirong, Li Xiaohe, Liu Jing, He Yachao, Zhang Kai, Temribagen. Mechanism of Mongolian medicine Echinops sphaerocephalus L. in proliferation and angiogenesis of vascular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7519-7528. |
| [6] | Wang Rongqiang, Yang Liu, Wu Xiangkun, Shang Lilin. Analysis of factors associated with prognosis of osteoporosis patients after hip arthroplasty and construction of Nomogram prediction model [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7137-7142. |
| [7] | Lu Xiuli, Xu Huazhen, Chen Yuxing, Yao Nan, Hu Zixuan, Huang Dane. Mechanism of Jiangu Formula in treating osteoporosis based on osteoclast-osteoblast coupling [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6828-6835. |
| [8] | Yan Laijun, Ge Haiya, Wang Zhengming, Yang Zongrui, Niu Lifeng, Zhan Hongsheng. Mechanism by which Tongdu Huoxue Decoction inhibits macrophage inflammation to delay intervertebral disc degeneration in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6851-6857. |
| [9] | Nigeayi · Aihemaiti, Yilidanna · Dilixiati, An Wei, Maimaitituxun · Tuerdi. Expression of mitochondrial creatine kinase 2 in a rat model of temporomandibular joint osteoarthritis and its role in inflammation progression [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6877-6884. |
| [10] | Wang Ziheng, Wu Shuang. Oxidative stress-related genes and molecular mechanisms after spinal cord injury: data analysis and verification based on GEO database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6893-6904. |
| [11] |
Zhou Rulin, Hu Yuanzheng, Wang Zongqing, Zhou Guoping, Zhang Baochao, Xu Qian, Bai Fanghui.
Exploration of biomarkers for moyamoya disease and analysis of traditional Chinese medicine targets#br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6927-6938.
|
| [12] | Zhao Xuemei, Wang Rui, Ao · Wuliji, Bao Shuyin, Jiang Xiaohua. Effects of Agiophyllum Oligo Saccharides on inflammation and apoptosis of mouse synovial cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6939-6946. |
| [13] | Zhu Jiaping, Gao Bo, Lou Chunbiao, Yang Fengyong, Yang Kun. Monomeric traditional Chinese medicine in the treatment of rheumatoid arthritis: regulation of T cell balance [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6955-6962. |
| [14] | Yao Tingfeng, Liu Lin, Liu Shixuan, Lu Xinyue. Meta-analysis of the effectiveness of dry needling at myofascial trigger points in the treatment of knee disorders [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6989-6996. |
| [15] | Wu Zhenhua, Zhang Xiwei, Wang Yipin, Li Qianqian. Relationship between seven serum lipid traits and osteoarthritis: a large sample analysis of European population in IEU OPEN GWAS database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 7004-7014. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||