Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (23): 4907-4914.doi: 10.12307/2025.086
Previous Articles Next Articles
Construction of tissue engineered urethra by combining acellular matrix with exosomes in small intestinal submucosa
Wang Dan, Zhu Xiaojun, Li Zhicheng, Li Na
- Department of Urology, Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, Inner Mongolia Autonomous Region, China
-
Received:2023-12-21Accepted:2024-05-20Online:2025-08-18Published:2024-09-28 -
Contact:Zhu Xiaojun, MD, Professor, Chief physician, Department of Urology, Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, Inner Mongolia Autonomous Region, China -
About author:Wang Dan, MD, Attending physician, Department of Urology, Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, Inner Mongolia Autonomous Region, China -
Supported by:National Natural Science Foundation of China, No. 81960131 (to WD)
CLC Number:
Cite this article
Wang Dan, Zhu Xiaojun, Li Zhicheng, Li Na. Construction of tissue engineered urethra by combining acellular matrix with exosomes in small intestinal submucosa[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 4907-4914.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
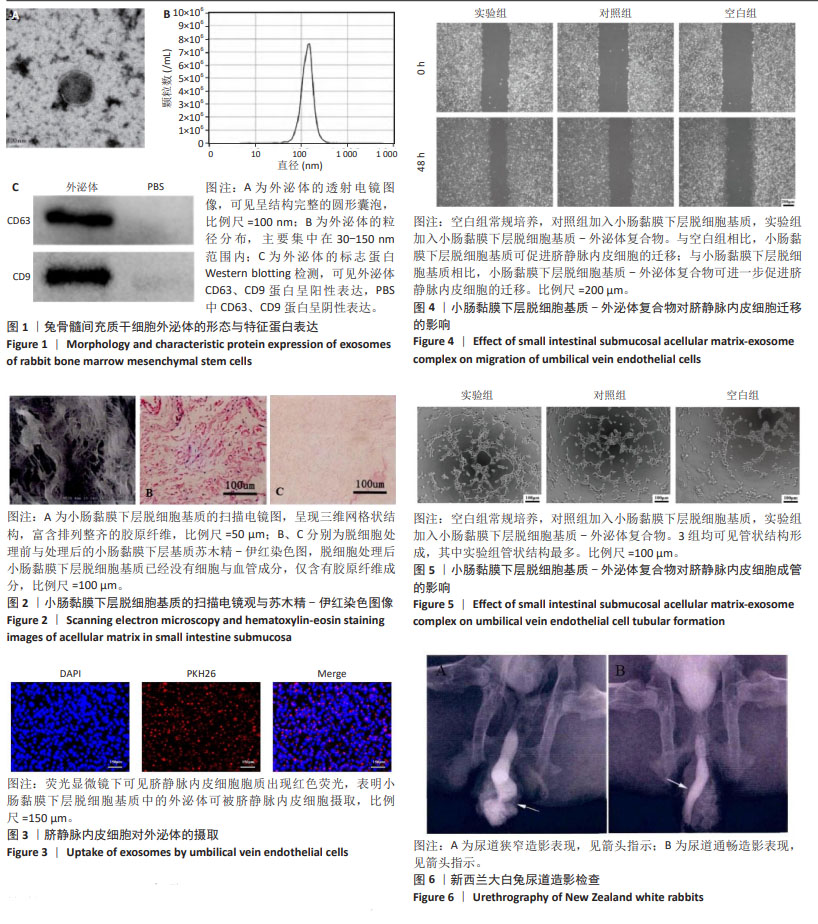
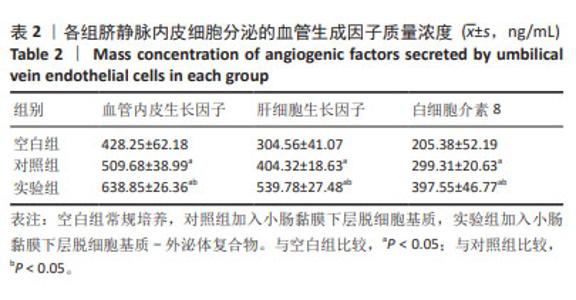
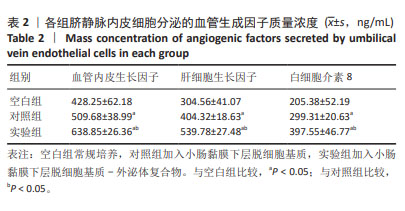
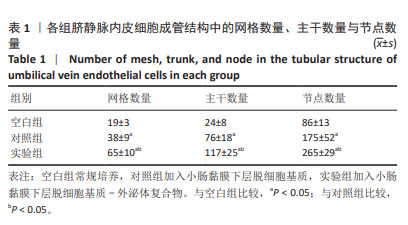
2.1 外泌体的形态与特征蛋白表达 透射电镜下可见提取的外泌体呈结构完整的圆形囊泡,符合外泌体的形态特征(图1A),纳米粒子跟踪分析囊泡直径大小主要集中在30-150 nm范围内(图1B),Western blotting检测显示提取的外泌体CD63、CD9蛋白呈阳性表达,PBS中CD63、CD9蛋白呈阴性表达(图1C)。 2.2 小肠黏膜下层脱细胞基质的形态 扫描电镜下可见小肠黏膜下层脱细胞基质呈现三维网格状结构,富含排列整齐的胶原纤维(图2A),苏木精-伊红染色显示相较于脱细胞处理前(图2B),小肠黏膜下层脱细胞基质已经没有细胞与血管成分,仅含有胶原纤维成分(图2C)。 2.3 小肠黏膜下层脱细胞基质-外泌体复合物的体外促血管生成作用 2.3.1 外泌体示踪实验 荧光显微镜下可见脐静脉内皮细胞胞质出现红色荧光(图3),表明小肠黏膜下层脱细胞基质中的外泌体可被脐静脉内皮细胞摄取,进而发挥其生物学效应。 2.3.2 脐静脉内皮细胞迁移实验 划痕实验显示,与空白组相比,小肠黏膜下层脱细胞基质可促进脐静脉内皮细胞的迁移;与小肠黏膜下层脱细胞基质相比,小肠黏膜下层脱细胞基质-外泌体复合物可进一步促进脐静脉内皮细胞的迁移(图4)。定量分析结果显示,空白组、对照组、实验组伤口闭合面积分别为(16.28±2.06)%,(25.78±6.52)%,(45.38±8.12)%,3组间比较差异有显著性意义(F=36.214,P=0.015)。 2.3.3 脐静脉内皮细胞成管实验 3组细胞的管状结构显微镜图片见图5,均可见管状结构形成,其中小肠黏膜下层脱细胞基质-外泌体复合物组管状结构最多。利用Image J软件测量管状结构中的网格数量、主干数量与节点数量,见表1,实验组网格数量、主干数量与节点数量均多于对照组、空白组(P < 0.05)。"
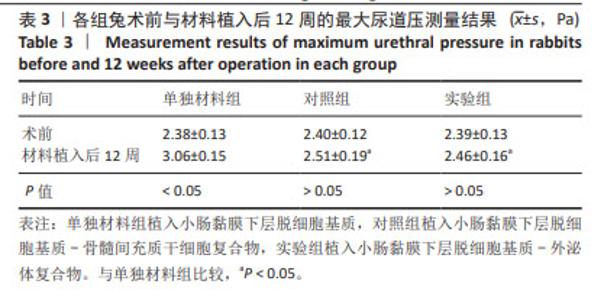
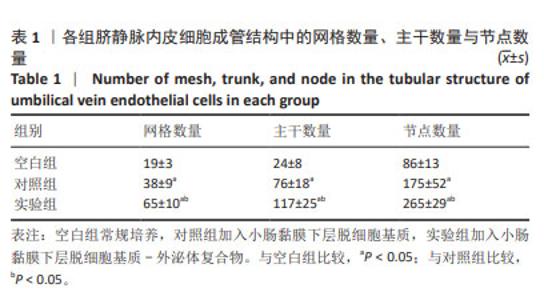
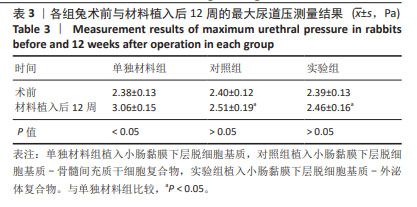
2.4 小肠黏膜下层脱细胞基质-外泌体复合物修复兔尿道缺损实验 2.4.1 实验动物数量分析 30只兔全部进入结果分析。 2.4.2 尿道造影与尿动力学检查 尿道造影检查显示,空白组10只兔均出现尿道狭窄(图6A),对照组10只兔有2只出现尿道狭窄、8只尿道通畅,实验组10只兔均无尿道狭窄发生(图6B)。 尿动力学检查结果显示,实验组、对照组兔手术前后的最大尿道压比较差异无显著性意义(P > 0.05),单独材料组兔术前与材料植入后12周的最大尿道压比较差异有显著性意义(P < 0.05),3组兔术前的最大尿道压比较差异无显著性意义(P > 0.05);实验组与对照组兔材料植入后12周的最大尿道压比较差异无显著性意义(P > 0.05),该两组兔材料植入后12周的最大尿道压均低于单独材料组(P < 0.05),见表3。"

2.4.3 重建尿道苏木精-伊红与Masson染色 苏木精-伊红与Masson染色结果显示,单独材料组可见明显的再生上皮层、少量的皮下平滑肌与血管,以纤维组织增生为主,并且伴有明显的炎性细胞浸润(图中星号标记部位);对照组可见较完整的再生上皮与少量的胶原,可见大量的皮下血管与平滑肌,伴有炎性细胞浸润(图中星号标记部位);实验组可见完整的再生上皮层与大量的皮下血管、平滑肌,未见明显的炎性细胞浸润(图7)。 2.4.4 重建尿道免疫组化染色 免疫组化染色结果显示,单独材料组、实验组上皮组织内AE1/AE3阳性表达面积大于对照组(P < 0.05),实验组ɑ-平滑肌肌动蛋白、CD31阳性染色面积均大于对照组(P < 0.05),对照组ɑ-平滑肌肌动蛋白、CD31阳性染色面积均大于单独材料组(P < 0.05),见图8。"

| [1] ABBASI B, SHAW NM, LUI JL, et al. Posterior urethral stenosis: a comparative review of the guidelines. World J Urol. 2022;40(11): 2591-2600. [2] CASTELLANI D, ANTONUCCI M, SIGNORETTI M, et al. Urethral and bladder neck stenosis after thulium laser enucleation of the prostate: Analysis of risk factors in a series of 1003 patients. Andrologia. 2022; 54(9):e14523. [3] LUMEN N, OOSTERLINCK W, HOEBEKE P. Urethral reconstruction using buccal mucosa or penile skin grafts: systematic review and meta-analysis. Urol Int. 2012;89(4):387-394. [4] WANG Z, ZENG X, CHEN R, et al. Free bladder mucosa graft harvested by water-jet: A novel, minimally invasive technique for urethral reconstruction. Exp Ther Med. 2018;16(3):2251-2256. [5] FERDOWSI KHOSROSHAHI A, SOLEIMANI RAD J, et al. Adipose tissue-derived stem cells upon decellularized ovine small intestine submucosa for tissue regeneration: An optimization and comparison method. J Cell Physiol. 2020;235(2):1556-1567. [6] SHI L, RONFARD V. Biochemical and biomechanical characterization of porcine small intestinal submucosa (SIS): a mini review. Int J Burns Trauma. 2013;3(4):173-179. [7] LUO JC, CHEN W, CHEN XH, et al. A multi-step method for preparation of porcine small intestinal submucosa (SIS). Biomaterials. 2011;32(3):706-713. [8] YEUM CE, PARK EY, LEE SB, et al. Quantification of MSCs involved in wound healing: use of SIS to transfer MSCs to wound site and quantification of MSCs involved in skin wound healing. J Tissue Eng Regen Med. 2013;7(4):279-291. [9] LIU Y, MA W, LIU B, et al. Urethral reconstruction with autologous urine-derived stem cells seeded in three-dimensional porous small intestinal submucosa in a rabbit model. Stem Cell Res Ther. 2017;8(1):63. [10] WANG D, DING X, XUE W, et al. A new scaffold containing small intestinal submucosa and mesenchymal stem cells improves pancreatic islet function and survival in vitro and in vivo. Int J Mol Med. 2017; 39(1):167-173. [11] ZOU J, YANG W, CUI W, et al. Therapeutic potential and mechanisms of mesenchymal stem cell-derived exosomes as bioactive materials in tendon-bone healing. J Nanobiotechnology. 2023;21(1):14. [12] LAI JJ, CHAU ZL, CHEN SY, et al. Exosome Processing and Characterization Approaches for Research and Technology Development. Adv Sci (Weinh). 2022;9(15):e2103222. [13] KALLURI R, LEBLEU VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478):eaau6977. [14] LIU W, LI L, RONG Y, et al. Hypoxic mesenchymal stem cell-derived exosomes promote bone fracture healing by the transfer of miR-126. Acta Biomater. 2020;103:196-212. [15] BASKARAN S, PANNER SELVAM MK, AGARWAL A. Exosomes of male reproduction. Adv Clin Chem. 2020;95:149-163. [16] WANG S, LI F, YE T, et al. Macrophage-tumor chimeric exosomes accumulate in lymph node and tumor to activate the immune response and the tumor microenvironment. Sci Transl Med. 2021;13(615): eabb6981. [17] LIN Z, WU Y, XU Y, et al. Mesenchymal stem cell-derived exosomes in cancer therapy resistance: recent advances and therapeutic potential. Mol Cancer. 2022;21(1):179. [18] HARRELL CR, VOLAREVIC V, DJONOV V, et al. Therapeutic Potential of Exosomes Derived from Adipose Tissue-Sourced Mesenchymal Stem Cells in the Treatment of Neural and Retinal Diseases. Int J Mol Sci. 2022;23(9):4487. [19] KANG K, MA R, CAI W, et al. Exosomes Secreted from CXCR4 Overexpressing Mesenchymal Stem Cells Promote Cardioprotection via Akt Signaling Pathway following Myocardial Infarction. Stem Cells Int. 2015;2015:659890. [20] ZHANG L, JIAO G, REN S, et al. Exosomes from bone marrow mesenchymal stem cells enhance fracture healing through the promotion of osteogenesis and angiogenesis in a rat model of nonunion. Stem Cell Res Ther. 2020;11(1):38. [21] DORIN RP, POHL HG, DE FILIPPO RE, et al. Tubularized urethral replacement with unseeded matrices: what is the maximum distance for normal tissue regeneration? World J Urol. 2008;26:323-326. [22] LI CL, LIAO WB, YANG SX, et al. Urethral reconstruction using bone marrow mesenchymal stem cell- and smooth muscle cell-seeded bladder acellular matrix. Transplant Proc. 2013;45(9):3402-3407. [23] WAGNER MEH, KAMPMANN A, SCHUMANN-MOOR K, et al. Cell seeding accelerates the vascularization of tissue engineering constructs in hypertensive mice. Hypertens Res. 2021;44(1):23-35. [24] YAN C, CHEN J, WANG C, et al. Milk exosomes-mediated miR-31-5p delivery accelerates diabetic wound healing through promoting angiogenesis. Drug Deliv. 2022;29(1):214-228. [25] SUN J, SHEN H, SHAO L, et al. HIF-1α overexpression in mesenchymal stem cell-derived exosomes mediates cardioprotection in myocardial infarction by enhanced angiogenesis. Stem Cell Res Ther. 2020; 11(1):373. [26] ZHANG Y, HAO Z, WANG P, et al. Exosomes from human umbilical cord mesenchymal stem cells enhance fracture healing through HIF-1α-mediated promotion of angiogenesis in a rat model of stabilized fracture. Cell Prolif. 2019;52(2):e12570. [27] QIU S, XIE L, LU C, et al. Gastric cancer-derived exosomal miR-519a-3p promotes liver metastasis by inducing intrahepatic M2-like macrophage-mediated angiogenesis. J Exp Clin Cancer Res. 2022;41(1):296. [28] LI Z, YAN-QING W, XIAO Y, et al. Exosomes secreted by chemoresistant ovarian cancer cells promote angiogenesis. J Ovarian Res. 2021;14(1):7. [29] HUANG Y, HE B, WANG L, et al. Bone marrow mesenchymal stem cell-derived exosomes promote rotator cuff tendon-bone healing by promoting angiogenesis and regulating M1 macrophages in rats. Stem Cell Res Ther. 2020;11(1):496. [30] GONG M, YU B, WANG J, et al. Mesenchymal stem cells release exosomes that transfer miRNAs to endothelial cells and promote angiogenesis. Oncotarget. 2017;8(28):45200-45212. |
| [1] | Lai Pengyu, Liang Ran, Shen Shan. Tissue engineering technology for repairing temporomandibular joint: problems and challenges [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Jin Kai, Tang Ting, Li Meile, Xie Yuan. Effects of conditioned medium and exosomes of human umbilical cord mesenchymal stem cells on proliferation, migration, invasion, and apoptosis of hepatocellular carcinoma cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1350-1355. |
| [3] | Aikepaer · Aierken, Chen Xiaotao, Wufanbieke · Baheti. Osteogenesis-induced exosomes derived from human periodontal ligament stem cells promote osteogenic differentiation of human periodontal ligament stem cells in an inflammatory microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1388-1394. |
| [4] | Lyu Liting, Yu Xia, Zhang Jinmei, Gao Qiaojing, Liu Renfan, Li Meng, Wang Lu. Bibliometric analysis of research process and current situation of brain aging and exosomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1457-1465. |
| [5] | Li Jialin, Zhang Yaodong, Lou Yanru, Yu Yang, Yang Rui. Molecular mechanisms underlying role of mesenchymal stem cell secretome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1512-1522. |
| [6] | Cao Yue, Ye Xinjian, Li Biyao, Zhang Yining, Feng Jianying. Effect of extracellular vesicles for diagnosis and therapy of oral squamous cell carcinoma [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1523-1530. |
| [7] | Guo Zhao, Zhuang Haoyan, Shi Xuewen. Role of exosomes derived from mesenchymal stem cells in treatment of colorectal cancer [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7872-7879. |
| [8] | Shui Jing, He Yu, Jiang Nan, Xu Kun, Song Lijuan, Ding Zhibin, Ma Cungen, Li Xinyi. Astrocytes regulate remyelination in central nervous system [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7889-7897. |
| [9] | Ma Weibang, Xu Zhe, Yu Qiao, Ouyang Dong, Zhang Ruguo, Luo Wei, Xie Yangjiang, Liu Chen. Screening and cytological validation of cartilage degeneration-related genes in exosomes from osteoarthritis synovial fluid [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7783-7789. |
| [10] | Zhang Min, Zhang Nini, Huang Guilin, Li Zhuangzhuang, Wang Xue, Wang Huike. Human amniotic mesenchymal stem cell exosomes repair radiation-induced submandibular gland damage in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7804-7815. |
| [11] | Guo Jia, Ren Yafeng, Li Bing, Huang Jing, Shang Wenya, Yang Yike, Liu Huiyao. Action mechanism of mesenchymal stem cell-derived exosomes carrying miRNAs in improving spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7827-7838. |
| [12] | Zhou Yang, Liu Kexin, Wang Deli, Sun Zhang. Regenerative effects of engineered extracellular vesicles on repairing bone defects [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7839-7847. |
| [13] | Zheng Yitong, Wang Yongxin, Liu Wen, Amujite, Qin Hu. Action mechanism of intrathecal transplantation of human umbilical cord mesenchymal stem cell-derived exosomes for repair of spinal cord injury under neuroendoscopy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7743-7751. |
| [14] | Zhang Xiongjinfu, Chen Yida, Cheng Xinyi, Liu Daihui, Shi Qin . Exosomes derived from bone marrow mesenchymal stem cells of young rats to reverse senescence in aged rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7709-7718. |
| [15] | Sima Xinli, Liu Danping, Qi Hui. Effect and mechanism of metformin-modified bone marrow mesenchymal stem cell exosomes on regulating chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7728-7734. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||