Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (18): 2817-2822.doi: 10.12307/2022.687
Previous Articles Next Articles
3D printed porous titanium alloy fusion cage and autologous iliac bone in the treatment of cervical spondylotic myelopathy
Ji Linsong1, Wang Yanping2, Lu tingsheng1, Jia Yijia1, Luo Chunshan1
- 1Department of Spine Surgery, 2Department of Gastroenterology, Guizhou Orthopedic Hospital, Guiyang 550002, Guizhou Province, China
-
Received:2021-09-06Accepted:2021-10-29Online:2022-06-28Published:2022-01-29 -
Contact:Luo Chunshan, MD, Chief physician, Department of Spine Surgery, Guizhou Orthopedic Hospital, Guiyang 550002, Guizhou Province, China -
About author:Ji Linsong, MD, Associate chief physician, Department of Spine Surgery, Guizhou Orthopedic Hospital, Guiyang 550002, Guizhou Province, China -
Supported by:Guiyang Science and Technology Bureau and Guizhou Provincial Orthopedic Hospitals Large-scale Health Science and Technology Cooperation Project in 2019, No. ZK [2019]9-5-4 (to JLS)
CLC Number:
Cite this article
Ji Linsong, Wang Yanping, Lu tingsheng, Jia Yijia, Luo Chunshan. 3D printed porous titanium alloy fusion cage and autologous iliac bone in the treatment of cervical spondylotic myelopathy[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2817-2822.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

2.4 两组患者颈部脊髓功能比较 使用Shapiro-Wilk test对两组患者手术前后的JOA评分做正态性检验,发现JOA评分均服从正态分布(P > 0.05)。使用Mauchly’s 球形检验分析变量的协方差矩阵是否相等,发现不同时间点的JOA评分满足球形检验(χ2=16.035,P=0.067)、不同分组的JOA评分满足球形检验(χ2=0.000,P=1.000)、不同时间点和测量组的交互满足球形检验(χ2=7.108,P=0.627),无需对结果进行校正。 采用重复测量设计方差分析对两组手术前后的JOA评分做差异性比较,结果显示:组间比较差异无显著性意义(F=1.916,P=0.178),各时间点间比较差异有显著性意义(F=74.094,P < 0.001),组别×时间点交互项差异比较差异无显著性意义(F=0.086,P=0.986);当交互作用统计学差异时,可单独分析主效应的意义,不需将每组拆分。采用LSD两两比较法分析不同测量时间点的差异,结果显示,术后各时间点的JOA评分均高于术前(P < 0.05),术后12个月的JOA评分高于术后6个月(P < 0.05),其余时间点间两两比较差异均无显著性意义(P > 0.05),见表3。"
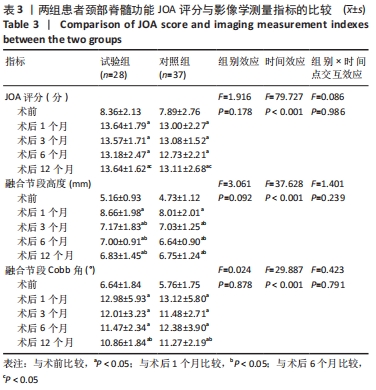

2.5 两组患者影像学测量指标的比较 使用Shapiro-Wilk test对两组手术前后的融合节段高度数据做正态性检验,结果显示融合节段高度数据均服从正态分布(P > 0.05)。使用Mauchly’s 球形检验分析变量的协方差矩阵是否相等,发现不同时间点的融合节段高度满足球形检验(χ2=16.270,P=0.062)、不同分组的融合节段高度满足球形检验(χ2=0.000,P=1.000)、不同时间点和测量组的交互不满足球形检验(χ2=18.454,P=0.031),采用Greenhouse-Geisser统计量对结果进行校正。 采用重复测量设计方差分析对两组手术前后的融合节段高度做差异性比较,结果显示:组间融合节段高度比较差异无显著性意义(F=3.061,P=0.092),各时间点间融合节段高度比较差异有显著性意义(F=37.628,P < 0.001),组别×时间点的交互项的融合节段高度比较差异无显著性意义(F=1.401,P=0.239);而当交互作用无统计学意义差异时,可单独分析主效应的意义,不需将每组拆分。采用LSD两两比较法分析不同测量时间点的差异,结果显示,术后各时间点的融合节段高度均高于术前(P < 0.05),术后3,6,12个月的融合节段高度低于术后1个月(P < 0.05),其余时间点间两两比较差异均无显著性意义(P > 0.05),见表3。 使用Shapiro-Wilk test对两组手术前后的Cobb角数据做正态性检验,发现Cobb角数据均服从正态分布(P > 0.05)。使用Mauchly’s 球形检验分析变量的协方差矩阵是否相等,发现不同时间点的Cobb角不满足球形检验(χ2=34.876,P < 0.001)、不同分组的Cobb角满足球形检验(χ2=0.000,P=1.000)、不同时间点和测量组的交互不满足球形检验(χ2=41.239,P < 0.001),采用Greenhouse-Geisser统计量对结果进行校正。 采用重复测量设计方差分析对两组手术前后的融合节段Cobb角数据做差异性比较,结果显示:组间融合节段Cobb角比较差异无显著性意义(F=0.024,P=0.878),各时间点间融合节段Cobb角比较差异有显著性意义(F=29.887,P < 0.001),组别×时间点的交互项的融合节段Cobb角比较差异无显著性意义(F=0.423,P=0.791);而当交互作用无统计学差异时,可单独分析主效应的意义,不需将每组拆分。采用LSD两两比较法分析不同测量时间点的差异,结果显示,术后各时间点的融合节段Cobb角均高于术前(P < 0.05),术后12个月的合节段Cobb角低于术后1个月(P < 0.05),其余时间点间两两比较差异均无显著性意义(P > 0.05),见表3。 2.6 两组融合材料生物相容性与手术并发症发生情况 术后试验组出现喉部疼痛、吞咽困难症状3例,对照组出现喉部疼痛、吞咽困难症状2例,症状在术后4周消失。两组均未出现钢板断裂、融合器退出及下沉等内固定并发症。对照组中有3例出现植骨块沉降,沉降率为8%。 2.7 典型病例影像资料 见图4,5。"

| [1] MA F, XU S, LIAO Y, et al. Using a mixture of local bone dust and morselized bone as graft materials in single-and double-level ACDF. BMC Musculoskelet Disord. 2021;22(1):1-10. [2] LIU JM, XIONG X, PENG AF, et al. A comparison of local bone graft with PEEK cage versus iliac bone graft used in anterior cervical discectomy and fusion. Clin Neurol Neurosurg. 2017;155:30-35. [3] GODLEWSKI B, STACHURA MK, CZEPKO RA, et al. Analysis of changes in cervical spinal curvature and intervertebral disk space height following ACDF surgery in a group of 100 patients followed up for 12 months. J Clin Neurosci. 2018;52:92-99. [4] GAO Y, OU Y, DENG Q, et al. Comparison between titanium mesh and autogenous iliac bone graft to restore vertebral height through posterior approach for the treatment of thoracic and lumbar spinal tuberculosis. PLoS One. 2017;12(4):e0175567. [5] ARTS M, TORENSMA B, WOLFS J. Porous titanium cervical interbody fusion device in the treatment of degenerative cervical radiculopathy; 1-year results of a prospective controlled trial. Spine J. 2020;20(7): 1065-1072. [6] VAN DEN BRINK W, LAMERIGTS N. Complete osseointegration of a retrieved 3-D printed porous titanium cervical cage. Front Surg. 2020;7:77. [7] LIU X, CHEN Y, YANG H, et al. Expansive open-door laminoplasty versus laminectomy and instrumented fusion for cases with cervical ossification of the posterior longitudinal ligament and straight lordosis. Eur Spine J. 2017;26(4):1173-1180. [8] 李玉伟,王海蛟,崔巍,等.前路颈椎间盘切除3D打印微孔钛合金椎间融合器与聚醚醚酮椎间融合器椎间融合术治疗脊髓型颈椎病的疗效对比[J].中国脊柱脊髓杂志,2021,31(1):16-24. [9] CHEN Y, LÜ G, WANG B, et al. A comparison of anterior cervical discectomy and fusion (ACDF) using self-locking stand-alone polyetheretherketone (PEEK) cage with ACDF using cage and plate in the treatment of three-level cervical degenerative spondylopathy: a retrospective study with 2-year follow-up. Eur Spine J. 2016;25(7): 2255-2262. [10] THOMÉ C, KRAUSS JK, ZEVGARIDIS D. A prospective clinical comparison of rectangular titanium cages and iliac crest autografts in anterior cervical discectomy and fusion. Neurosurg Rev. 2004;27(1):34-41. [11] STEVENSON S, EMERY SE, GOLDBERG VM. Factors affecting bone graft incorporation. Clin Orthop Relat Res. 1996;324:66-74. [12] YIN S, ZHANG W, ZHANG Z, et al. Recent advances in scaffold design and material for vascularized tissue‐engineered bone regeneration. Adv Healthc Mater. 2019;8(10):1801433. [13] FITZPATRICK V, MARTÍN-MOLDES Z, DECK A, et al. Functionalized 3D-printed silk-hydroxyapatite scaffolds for enhanced bone regeneration with innervation and vascularization. Biomaterials. 2021; 276:120995. [14] WENG Y, WANG Z, SUN J, et al. Engineering of axially vascularized bone tissue using natural coral scaffold and osteogenic bone marrow mesenchymal stem cell sheets. J Stomatol Oral Maxillofac Surg. 2021; 122(4):397-404. [15] KONDA SR, LITTLEFIELD CP, CARLOCK KD, et al. Autogenous iliac crest bone grafting for tibial nonunions revisited: does approach matter? Arch Orthop Trauma Surg. 2021. doi: 10.1007/s00402-020-03735-6. [16] YEE TJ, SWONG K, PARK P. Complications of anterior cervical spine surgery: a systematic review of the literature. J Spine Surg. 2020;6(1): 302. [17] NOORDHOEK I, KONING M, VLEGGEERT-LANKAMP C. Evaluation of bony fusion after anterior cervical discectomy: a systematic literature review. Eur Spine J. 2019;28(2):386-399. [18] LEE JC, JANG HD, AHN J, et al. Comparison of cortical ring allograft and plate fixation with autologous iliac bone graft for anterior cervical discectomy and fusion. Asian Spine J. 2019;13(2):258. [19] IUNES EA, BARLETTA EA, BELSUZARRI TAB, et al. Correlation between different interbody grafts and pseudarthrosis after anterior cervical discectomy and fusion compared with control group: systematic review. World Neurosurg. 2020;134:272-279. [20] PARK JS, PARK SJ, LEE CS, et al. Is allograft a more reliable treatment option than autograft in 2-level anterior cervical discectomy and fusion with plate fixation? Medicine (Baltimore). 2019;98(32):e16621. [21] KADAM A, MILLHOUSE PW, KEPLER CK, et al. Bone substitutes and expanders in spine surgery: a review of their fusion efficacies. Int J Spine Surg. 2016;10:33. [22] PARK HW, LEE JK, MOON SJ, et al. The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine J. 2009; 34(17):E591-E595. [23] RAO PJ, PELLETIER MH, WALSH WR, et al. Spine interbody implants: material selection and modification, functionalization and bioactivation of surfaces to improve osseointegration. Orthop Surg. 2014;6(2):81-89. [24] ZHU C, HE M, MAO L, et al. Titanium-interlayer mediated hydroxyapatite coating on polyetheretherketone: a prospective study in patients with single-level cervical degenerative disc disease. J Transl Med. 2021;19(1):1-8. [25] CAMPBELL PG, CAVANAUGH DA, NUNLEY P, et al. PEEK versus titanium cages in lateral lumbar interbody fusion: a comparative analysis of subsidence. Neurosurg Focus. 2020;49(3):E10. [26] ADL AMINI D, OKANO I, OEZEL L, et al. Evaluation of cage subsidence in standalone lateral lumbar interbody fusion: novel 3D-printed titanium versus polyetheretherketone (PEEK) cage. Eur Spine J. 2021;30(8): 2377-2384. [27] LU T, LIU C, YANG B, et al. Single-level anterior cervical corpectomy and fusion using a new 3D-printed anatomy-adaptive titanium mesh cage for treatment of cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: a retrospective case series study. Med Sci Monit. 2017;23:3105. [28] WU J, LUO D, YE X, et al. Anatomy-related risk factors for the subsidence of titanium mesh cage in cervical reconstruction after one-level corpectomy. Int J Clin Exp Med. 2015;8(5):7405. [29] LU T, GAO Z, LI J, et al. Construction of a new cervical anatomically adaptive titanium mesh cage based on measurements of cervical geometry: A morphological and cadaveric study. Exp Ther Med. 2021; 22(5):1-9. [30] WANG Y, ZHAN Y, YANG H, et al. A novel anatomic titanium mesh cage for reducing the subsidence rate after anterior cervical corpectomy: a finite element study. Sci Rep. 2021;11(1):1-9. [31] HUR JW, RYU KS, AHN S, et al. Comparative analysis of 2 different types of titanium mesh cage for single-level anterior cervical corpectomy and fusion in terms of postoperative subsidence and sagittal alignment. Clin Spine Surg. 2020;33(1):E8-E13. [32] WEN Z, LU T, WANG Y, et al. Anterior cervical corpectomy and fusion and anterior cervical discectomy and fusion using titanium mesh cages for treatment of degenerative cervical pathologies: a literature review. Med Sci Monit. 2018;24:6398. [33] LU T, LIANG H, LIU C, et al. Effects of titanium mesh cage end structures on the compressive load at the endplate interface: a cadaveric biomechanical study. Med Sci Monit. 2017;23:2863. [34] CHOY WJ, PARR WCH, PHAN K, et al. 3-dimensional printing for anterior cervical surgery: a review. J Spine Surg. 2018;4(4):757. [35] SCHULZ C, MAUER UM, MATHIEU R. Clinical and Radiological Results after Anterior Cervical Corpectomy with Cage Fusion-a Retrospective Comparison of PEEK vs. Titanium Cages. Z Orthop Unfall. 2017;155(2): 201-208. [36] WOO JB, SON DW, LEE SH, et al. Risk factors of allogenous bone graft collapse in two-level anterior cervical discectomy and fusion. J Korean Neurosurg Soc. 2019;62(4):450. [37] FANG T, ZHANG M, YAN J, et al. Comparative Analysis of 3D-Printed Artificial Vertebral Body Versus Titanium Mesh Cage in Repairing Bone Defects Following Single-Level Anterior Cervical Corpectomy and Fusion. Med Sci Monit. 2021;27:e928022-928021. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [3] | Yang Jun, Yang Qun, Zhang Rui, Jiang Chang. A novel slidable pedicle screw-rod system for lumbar tuberculosis: promoting bone graft fusion by producing stress stimulation to fused segment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 914-918. |
| [4] | Li Jian, Bao Zhengqi, Zhou Pinghui, Zhu Ruizhi, Li Zhixiang, Wang Jinzi. Effects of posterior single open-door laminoplasty and anterior cervical corpectomy fusion on cervical sagittal balance parameters in the treatment of multilevel cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 949-953. |
| [5] | Zhang Qi, Xiong Yang, Yu Xing, Yang Yongdong, Song Jiawei, Qiu Ziye, Ma Yukun, Jiang Guozheng, Feng Ningning, Wang Shuyang. Mobi-C combined with ROI-C fusion cage versus ROI-C fusion cage alone for the treatment of two-level cervical spondylosis: midterm efficacy follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 397-402. |
| [6] | Deng Bowen, Li Xiaoye, Jiang Shengyuan, Liu Gan, Zhao Yi, Zhang Houjun, He Feng, Mu Xiaohong. Mechanisms of Huangqi Guizhi Wuwu Decoction in the treatment of cervical spondylosis and anxiety disorder based on the principle of “treating different diseases with the same method”: a network pharmacology analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(23): 3650-3656. |
| [7] | Xiong Yang, Yang Yingli, Gao Yushan, Wang Xiumei, Yang Yongdong, Zhao Dingyan, Zhao He, Li Chuanhong, Yang Kaitan, Yu Xing. Histological changes of cervical disc tissue and underlying ossification mechanism in patients with cervical degenerative ossification [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2868-2873. |
| [8] | Liu Zhengpeng, Wang Yahui, Zhang Yilong, Ming Ying, Sun Zhijie, Sun He. Application of 3D printed interbody fusion cage for cervical spondylosis of spinal cord type: half-year follow-up of recovery of cervical curvature and intervertebral height [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 849-853. |
| [9] | Wei Haoxin, Wang Caiping, Deng Qian, Song Yan, Wang Xiaowen, Wang Jinwu. Design and clinical application of personalized cervical spine correction pillow with three-dimensional printing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5741-5746. |
| [10] | Zhao Lingtong, Hu Bing. Modified open-door laminoplasty with preserved posterior cervical musculo-ligamentous complex in the treatment of cervical spondylotic myelopathy: neurological function and axial symptoms [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(33): 5345-5350. |
| [11] | Zhang Chunlin, Zhao Xiao, Yan Xu, Ning Yongming, Cao Zhengming. Cervical microendoscopic laminoplasty and intervertebral disc resorption after conservative treatment assessed with three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4774-4780. |
| [12] | Wang Shuguang, Cai Tongchuan, Feng Xinmin, Nan Liping, Wang Feng, Zhu Lei, Chen Dong, Zhang Liang. Meta-analysis of adverse events between anterior and posterior fusion surgery for multiple-level cervical spondylosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4907-4914. |
| [13] | Zhao Hongshun, A Jiancuo, Wang Deyuan, Xu Zhihua, Gao Shunhong. Factors affecting the height of early intervertebral space after lumbar interbody fusion via lateral approach [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3332-3336. |
| [14] | Chen Jiang, Li Jinyu, Zheng Chenying, Bai Chunxiao, Zhang Fan, Liu Chuyin, Zhao Xueqian, Yuan Qiaomei, Di Xueshi, Kang Shengqian, Jia Yusong . Changes in sagittal parameters of cervical spine after double-segment artificial cervical disc replacement and anterior cervical discectomy and fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2341-2346. |
| [15] | Ma Long, Tan Xiaoxin, Sun Guoshao. A 5-year follow-up on sagittal alignment and radiological outcomes of consecutive three-level anterior cervical discectomy and fusion and hybrid surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1879-1885. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||