Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (17): 4299-4308.doi: 10.12307/2026.130
Previous Articles Next Articles
Preparation and evaluation of an animal model of osteoporosis and osteoarthritis comorbidity in rats
Fu Jingyue1, 2, Zhou Qinfeng2, Li Muzhe2, Ma Yong2, 3, Pan Yalan2, 4, Sun Jie2, Huang Xiangyang2, Guo Yang2
- 1School of Chinese Medicine, 2New Technology Laboratory of Bone Injury Repair and Reconstruction, 4Institute of Integrative Medicine Nursing Research, Nanjing University of Chinese Medicine, Nanjing 210023, Jiangsu Province, China; 3Yancheng Affiliated Hospital of Nanjing University of Chinese Medicine, Yancheng 224002, Jiangsu Province, China
-
Received:2025-04-24Accepted:2025-07-15Online:2026-06-18Published:2025-11-26 -
Contact:Guo Yang, PhD, Associate professor, Master’s supervisor, New Technology Laboratory of Bone Injury Repair and Reconstruction, Nanjing University of Chinese Medicine, Nanjing 210023, Jiangsu Province, China -
About author:Fu Jingyue, MS candidate, School of Chinese Medicine, Nanjing University of Chinese Medicine, Nanjing 210023, Jiangsu Province, China; New Technology Laboratory of Bone Injury Repair and Reconstruction, Nanjing University of Chinese Medicine, Nanjing 210023, Jiangsu Province, China -
Supported by:National Natural Science Foundation of China (General Program), No. 82174411(to MY); Jiangsu Provincial Natural Science Foundation (General Program), No. BK20221351 (to GY); High-Level Key Discipline Construction Project of Traditional Chinese Medicine funded by the National Administration of Traditional Chinese Medicine, No. [2023]85 (to MY); Yancheng Basic Research Program General Project, No. YCBK2024087 (to MY); Jiangsu Provincial Graduate Research Innovation Program, No. KYCX24_2190 (to FJY)
CLC Number:
Cite this article
Fu Jingyue, Zhou Qinfeng, Li Muzhe, Ma Yong, Pan Yalan, Sun Jie, Huang Xiangyang, Guo Yang. Preparation and evaluation of an animal model of osteoporosis and osteoarthritis comorbidity in rats[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(17): 4299-4308.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

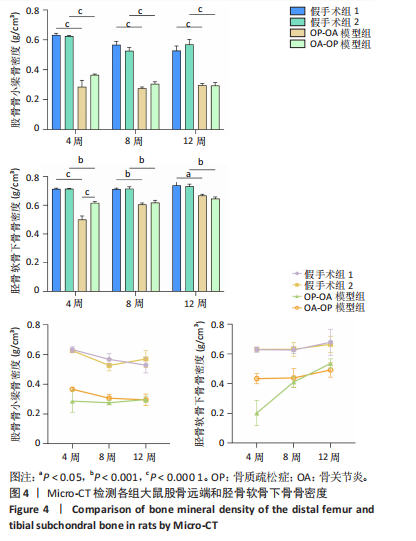
2.1 实验动物数量分析 实验选用60只SD大鼠,造模过程中因麻醉时间较长,骨质疏松症-骨关节炎模型组和骨关节炎-骨质疏松症模型组各死亡1只,造模成功后未出现动物死亡,全部进入后续实验结果分析。 2.2 影像学指标 2.2.1 骨密度 Micro-CT检测分析股骨远端骨密度(图4),与假手术组相比,在术后4,8,12周2个模型组股骨骨密度随时间进展均显著下降(P < 0.000 1),且2个模型组之间无显著差异。 Micro-CT检测分析胫骨平台软骨下骨骨密度(图4),术后4周,2个模型组软骨下骨骨密度较假手术组均显著下降(P < 0.001),且骨质疏松症-骨关节炎模型组下降更显著(P < 0.000 1)。术后8,12周,2个模型组软骨下骨骨密度较假手术组均显著下降(P < 0.05),且2个模型组间软骨下骨骨密度无显著差异。骨质疏松症-骨关节炎模型组术后8,12周较术后4周软骨下骨骨密度显著升高(P < 0.000 1,P < 0.05),骨关节炎-骨质疏松症模型组术后8,12周较术后4周软骨下骨骨密度有所升高,但无显著差异。 2.2.2 软骨下骨微结构 Micro-CT图像二维冠状面显示(图5),假手术组1、假手术组2大鼠膝关节解剖结构清晰可见,软骨下骨板较厚,软骨下骨骨小梁排列紧密且厚度均匀,未见骨赘与骨刺;2个模型组术后8,12周软骨下骨板厚度变薄,软骨下骨骨小梁排列稀疏、间隙变大且连续性破坏,周围可见明显骨赘与骨刺。三维重构图像显示(图5),假手"
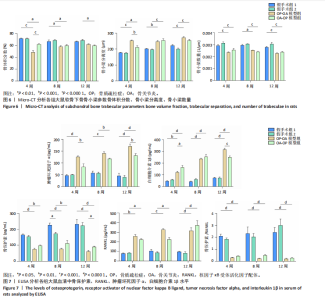
术组1、假手术组2大鼠关节表面光整,未见骨赘或骨刺;2个模型组术后8,12周关节表面粗糙,出现表面不平整及凹陷等损伤退化,可见多处骨赘及骨刺,多角度可见有游离体生成。 软骨下骨骨微结构参数结果显示(图6),与假手术组相比,2个模型组大鼠骨体积分数、骨小梁数量显著降低(P < 0.01),骨小梁分离度显著升高(P < 0.01),表明造模后大鼠软骨下骨骨小梁骨量减少,骨强度下降,骨微结构遭到破坏。术后4周,骨质疏松症-骨关节炎模型组大鼠骨体积分数较骨关节炎-骨质疏松症模型组偏低(P < 0.000 1),骨小梁分离度偏高(P < 0.001),术后8,12周2个模型组之间各指标无统计学差异。 2.3 各组大鼠血清中骨保护素、核因子κB受体活化因子配体、肿瘤坏死因子α、白细胞介素1β 水平变化 如图7所示,与假手术组相比,2个模型组大鼠血清中炎性因子肿瘤坏死因子α、白细胞介素1β水平均显著增加(P < 0.01)。术后4,12周,骨关节炎-骨质疏松症模型组大鼠血清中肿瘤坏死因子α 水平较骨质疏松症-骨关节炎模型组降低(P < 0.01);术后8周,2个模型组血清肿瘤坏死因子α 水平无显著差异。术后4周,骨关节炎-骨质疏松症模型组"
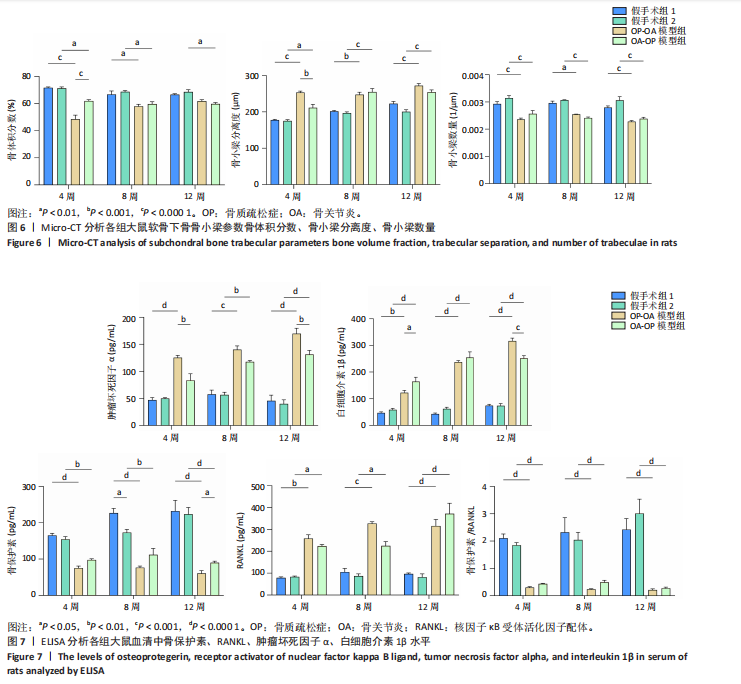
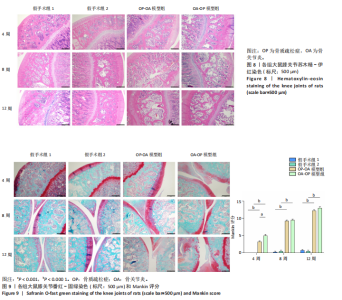
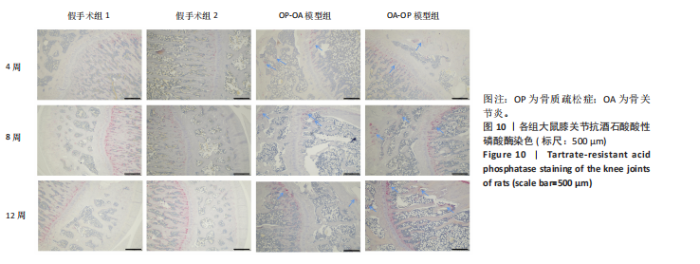
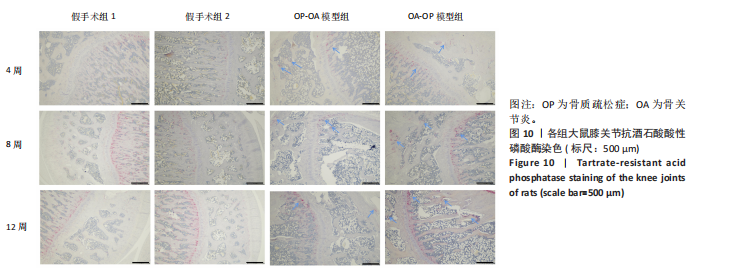
大鼠血清中白细胞介素1β水平较骨质疏松症-骨关节炎模型组升高(P < 0.05);术后8周,2个模型组血清白细胞介素1β水平差异无显著性意义;术后12周,骨关节炎-骨质疏松症模型组大鼠血清中白细胞介素1β水平较骨质疏松症-骨关节炎模型组降低(P < 0.001)。此外,与假手术组相比,2个模型组大鼠血清中骨保护素水平均显著降低(P < 0.01),核因子κB受体活化因子配体水平均显著升高(P < 0.05),骨保护素/核因子κB受体活化因子配体比值均显著降低(P < 0.001),两种造模方式之间无显著差异。 2.4 病理学观察结果 苏木精-伊红染色结果显示(图8),假手术组1、假手术组2关节软骨层4层结构排列紧密、有序,软骨细胞排列整齐,潮线完整连续,软骨下骨骨小梁数量多且厚度适中,排列有序,骨小梁之间连接紧密。术后4周,2个模型组软骨表面不平整,出现轻微的凹凸不平,骨小梁数量减少,排列紊乱,骨髓腔变大且出现大量脂肪空泡;术后8周,2个模型组软骨层明显变薄,表面有缺损浅裂隙,层状结构遭到破坏,潮线中断,软骨下骨骨小梁厚度变薄,断裂多,骨髓腔变大;术后12周,2个模型组软骨损伤进一步加重,骨小梁硬化。 番红-固绿染色结果显示(图9),假手术组1、假手术组2软骨表面平整,软骨细胞分布均匀,潮线清晰。术后4周,2个模型组软骨表面不平整,软骨细胞分布不均;术后8周,关节间隙减小,潮线中断;术后12周,蛋白多糖严重丢失,染色红色信号减弱甚至完全褪色。"

| [1] WHITTY CJM, MACEWEN C, GODDARD A, et al. Rising to the challenge of multimorbidity. BMJ. 2020;368:l6964. [2] THE LANCET. Making more of multimorbidity: an emerging priority. Lancet. 2018;391(10131):1637. [3] GEUSENS PP, VAN DEN BERGH JP. Osteoporosis and osteoarthritis: shared mechanisms and epidemiology. Curr Opin Rheumatol. 2016; 28(2):97-103. [4] CHEN X, TANG H, LIN J, et al. Temporal trends in the disease burden of osteoarthritis from 1990 to 2019, and projections until 2030. PLoS One. 2023;18(7):e0288561. [5] MUÑOZ M, ROBINSON K, SHIBLI-RAHHAL A. Bone Health and Osteoporosis Prevention and Treatment. Clin Obstet Gynecol. 2020; 63(4):770-787. [6] YUE L, BERMAN J. What Is Osteoarthritis? JAMA. 2022;327(13):1300. [7] DAINESE P, WYNGAERT KV, DE MITS S, et al. Association between knee inflammation and knee pain in patients with knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2022; 30(4):516-534. [8] 北京医学会骨科学分会关节外科学组.老年骨关节炎及骨质疏松症诊断与治疗社区管理专家共识(2023版)[J].协和医学杂志, 2023,14(3):484-493. [9] CLAYTON ES, HOCHBERG MC. Osteoporosis and osteoarthritis, rheumatoid arthritis and spondylarthropathies. Curr Osteoporos Rep. 2013;11(4):257-262. [10] 魏戌,刘宁,章轶立,等.骨质疏松症的共病研究与早期筛查[J].中国全科医学,2022,25(35):4369-4374. [11] KIM D, PIRSHAHID AA, LI Y, et al. Prevalence of osteoporosis in osteoarthritis: a systematic review and meta-analysis. Osteoporos Int. 2022;33(8):1687-1693. [12] BULTINK IE, LEMS WF. Osteoarthritis and osteoporosis: what is the overlap? Curr Rheumatol Rep. 2013;15(5):328. [13] 章轶立,黄馨懿,齐保玉,等.老年人共病研究的现实意义、内容方法与前景展望[J].中国循证医学杂志,2023,23(7):862-868. [14] 章轶立,黄馨懿,齐保玉,等.老年人群共病问题现状挑战与应对策略[J].中国全科医学,2022,25(35):4363-4368. [15] WANG D, QI Y, WANG Z, et al. Recent Advances in Animal Models, Diagnosis, and Treatment of Temporomandibular Joint Osteoarthritis. Tissue Eng Part B Rev. 2023;29(1):62-77. [16] KIM JL, MOON CW, SON YS, et al. Combined Effect of Bilateral Ovariectomy and Anterior Cruciate Ligament Transection With Medial Meniscectomy on the Development of Osteoarthritis Model. Ann Rehabil Med. 2016;40(4):583-591. [17] BEI MJ, TIAN FM, XIAO YP, et al. Raloxifene retards cartilage degradation and improves subchondral bone micro-architecture in ovariectomized rats with patella baja-induced - patellofemoral joint osteoarthritis. Osteoarthritis Cartilage. 2020;28(3):344-355. [18] LUGO L, VILLALVILLA A, GÓMEZ R, et al. Effects of PTH [1-34] on synoviopathy in an experimental model of osteoarthritis preceded by osteoporosis. Osteoarthritis Cartilage. 2012;20(12):1619-1630. [19] 方锐,艾力江·阿斯拉,卢勇,等.兔骨性关节炎模型构建及早中晚期的特点[J].中国组织工程研究与临床康复,2010,14(7):1218-1222. [20] 麦聪英,谭峰,李星,等.左归丸对绝经后骨质疏松症合并骨关节炎模型大鼠下丘脑神经肽P物质及其受体的影响[J].中医杂志, 2021,62(14):1259-1265. [21] 刘玲玲,许凌云,王斌.骨质疏松及骨关节炎与雌激素和细胞因子关系的研究进展[J].现代临床医学,2023,49(2):137-139. [22] BUCAY N, SAROSI I, DUNSTAN CR, et al. Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998;12(9):1260-1268. [23] 周逸敏,邱友利,张俐.膝骨关节炎合并骨质疏松症大鼠模型的建立与评估[J].中国中医骨伤科杂志,2017,25(9):1-4. [24] 李楠,王猛,刘永明,等.卵巢切除术构建大鼠骨关节炎合并骨质疏松模型的可行性[J].现代生物医学进展,2015,15(13):2413-2416. [25] TORRENT A, MONTELL E, VERGÉS J, et al. Effect of chondroitin sulphate and glucosamine in combination in an animal model of osteoarthritis and Osteoporosis. Osteoarthritis Cartilage. 2014;22:S351. [26] MA Z, WEI Y, ZHANG L, et al. GCTOF-MS Combined LC-QTRAP-MS/MS Reveals Metabolic Difference Between Osteoarthritis and Osteoporotic Osteoarthritis and the Intervention Effect of Erxian Decoction. Front Endocrinol (Lausanne). 2022;13:905507. [27] PARK S, LEE LR, SEO JH, et al. Curcumin and tetrahydrocurcumin both prevent osteoarthritis symptoms and decrease the expressions of pro-inflammatory cytokines in estrogen-deficient rats. Genes Nutr. 2016;11:2. [28] HU YC, HUANG TC, HUANG LW, et al. S-Equol Ameliorates Menopausal Osteoarthritis in Rats through Reducing Oxidative Stress and Cartilage Degradation. Nutrients. 2024;16(14):2364. [29] ABRAMOFF B, CALDERA FE. Osteoarthritis: Pathology, Diagnosis, and Treatment Options. Med Clin North Am. 2020;104(2):293-311. [30] 邢润麟,王培民,张农山,等.中医“肝肾同源”理论异病同治膝骨关节炎和绝经后骨质疏松症的实验理论基础研究[J].中医正骨,2017,29(1):1-10. [31] HU W, CHEN Y, DOU C, et al. Microenvironment in subchondral bone: predominant regulator for the treatment of osteoarthritis. Ann Rheum Dis. 2021;80(4):413-422. [32] 章家皓,田佳庆,王帅,等.补肾强筋胶囊对膝骨关节炎大鼠膝关节软骨下骨质的影响及其作用机制的实验研究[J].中医正骨, 2024,36(8):19-26. [33] HULLEY PA, PAPADIMITRIOU-OLIVGERI I, KNOWLES HJ. Osteoblast-Osteoclast Coculture Amplifies Inhibitory Effects of FG-4592 on Human Osteoclastogenesis and Reduces Bone Resorption. JBMR Plus. 2020;4(7):e10370. [34] LI Y, LIEM Y, DALL’ARA E, et al. Subchondral bone microarchitecture and mineral density in human osteoarthritis and osteoporosis: A regional and compartmental analysis. J Orthop Res. 2021;39(12):2568-2580. [35] KENKRE JS, BASSETT J. The bone remodelling cycle. Ann Clin Biochem. 2018;55(3):308-327. [36] 司元龙,陈志伟,申建军.基于OPG/RANKL/RANK信号通路探讨中医“血瘀”与膝骨关节炎[J/OL].中医学报,1-9[2025-03-20].http://kns.cnki.net/kcms/detail/41.1411.R.20241127.1424.036.html. [37] BELLIDO M, LUGO L, ROMAN-BLAS JA, et al. Subchondral bone microstructural damage by increased remodelling aggravates experimental osteoarthritis preceded by osteoporosis. Arthritis Res Ther. 2010;12(4):R152. [38] CHU L, LIU X, HE Z, et al. Articular Cartilage Degradation and Aberrant Subchondral Bone Remodeling in Patients with Osteoarthritis and Osteoporosis. J Bone Miner Res. 2020;35(3):505-515. [39] CHE AHMAD TANTOWI NA, LAU SF, MOHAMED S. Ficus deltoidea Prevented Bone Loss in Preclinical Osteoporosis/Osteoarthritis Model by Suppressing Inflammation. Calcif Tissue Int. 2018;103(4):388-399. [40] BULTINK IE, VIS M, VAN DER HORST-BRUINSMA IE, et al. Inflammatory rheumatic disorders and bone. Curr Rheumatol Rep. 2012;14(3):224-230. |
| [1] | Zhang Nan, Meng Qinghua, Bao Chunyu. Characteristics and clinical application of ankle joint finite element models [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2343-2349. |
| [2] | Chen Qiuhan, Yang Long, Yuan Daizhu, Wu Zhanyu, Zou Zihao, Ye Chuan. Peri-knee osteotomy for treatment of knee osteoarthritis: optimization of treatment strategies [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2303-2312. |
| [3] | Zhang Zizheng, Luo Wang, Liu Changlu. Application value of finite element analysis on unicompartmental knee arthroplasty for medial knee compartmental osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2313-2322. |
| [4] | Li Qingbin, Lin Jianhui, Huang Wenjie, Wang Mingshuang, Du Jiankai, Lao Yongqiang. Bone cement filling after enlarged curettage of giant cell tumor around the knee joint: a comparison of subchondral bone grafting and non-grafting [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1896-1902. |
| [5] | Li Linzhen, Jiao Hongzhuo, Chen Weinan, Zhang Mingzhe, Wang Jianlong, Zhang Juntao. Effect of icariin-containing serum on lipopolysaccharide-induced inflammatory damage in human chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1368-1374. |
| [6] | Chen Ju, Zheng Jinchang, Liang Zhen, Huang Chengshuo, Lin Hao, Zeng Li. Effect and mechanism of beta-caryophyllene in mice with osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1341-1347. |
| [7] | Lyu Guoqing, Aizimaitijiang·Rouzi, Xiong Daohai. Irisin inhibits ferroptosis in human articular chondrocytes: roles and mechanisms [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1359-1367. |
| [8] | Zhang Haiwen, Zhang Xian, Xu Taichuan, Li Chao. Bibliometric and visual analysis of the research status and trends of senescence in osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1580-1591. |
| [9] | Li Hao, Tao Hongcheng, Zeng Ping, Liu Jinfu, Ding Qiang, Niu Chicheng, Huang Kai, Kang Hongyu. Mitogen-activated protein kinase signaling pathway regulates the development of osteoarthritis: guiding targeted therapy with traditional Chinese medicine [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1476-1485. |
| [10] | Bu Yangyang, Ning Xinli, Zhao Chen. Intra-articular injections for the treatment of osteoarthritis of the temporomandibular joint: different drugs with multiple combined treatment options [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1215-1224. |
| [11] | Zhang Qian, Huang Dongfeng. Weighted gene co-expression network analysis combined with machine learning to screen and validate biomarkers for osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1096-1105. |
| [12] | Yang Xiao, Bai Yuehui, Zhao Tiantian, Wang Donghao, Zhao Chen, Yuan Shuo. Cartilage degeneration in temporomandibular joint osteoarthritis: mechanisms and regenerative challenges [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 926-935. |
| [13] | Rong Xiangbin, , Zheng Haibo, Mo Xueshen, Hou Kun, Zeng Ping, . Plasma metabolites, immune cells, and hip osteoarthritis: causal inference based on GWAS data from European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1028-1035. |
| [14] | Gu Fucheng, Yang Meixin, Wu Weixin, Cai Weijun, Qin Yangyi, Sun Mingyi, Sun Jian, Geng Qiudong, Li Nan. Effects of Guilu Erxian Glue on gut microbiota in rats with knee osteoarthritis: machine learning and 16S rDNA analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1058-1072. |
| [15] | Chen Yixian, Chen Chen, Lu Liheng, Tang Jinpeng, Yu Xiaowei. Triptolide in the treatment of osteoarthritis: network pharmacology analysis and animal model validation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 805-815. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||