Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (33): 7087-7095.doi: 10.12307/2025.857
Previous Articles Next Articles
Finite element analysis and biomechanical validation of revision pedicle screw placement
Ma Shuangshuang1, Gao Dedong1, Shan Zhongshu2, Xu Wenxu3, Lu Zhirui1
- 1College of Mechanical Engineering, 3College of Computer Technology and Application, Qinghai University, Xining 810016, Qinghai Province, China; 2Department of Orthopedics, Qinghai Provincial People’s Hospital, Xining 810016, Qinghai Province, China
-
Received:2024-08-09Accepted:2024-09-29Online:2025-11-28Published:2025-04-12 -
Contact:Gao Dedong, MD, Professor, College of Mechanical Engineering, Qinghai University, Xining 810016, Qinghai Province, China Shan Zhongshu, Chief physician, Department of Orthopedics, Qinghai Provincial People’s Hospital, Xining 810016, Qinghai Province, China -
About author:Ma Shuangshuang, Master candidate, College of Mechanical Engineering, Qinghai University, Xining 810016, Qinghai Province, China -
Supported by:Qinghai Provincial Science and Technology Plan Project, No. 2020-ZJ-T08 (to SZS); Qinghai Provincial Central Guidance Local Science and Technology Development Fund Project, No. 2024ZY032 (to SZS)
CLC Number:
Cite this article
Ma Shuangshuang, Gao Dedong, Shan Zhongshu, Xu Wenxu, Lu Zhirui. Finite element analysis and biomechanical validation of revision pedicle screw placement[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7087-7095.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
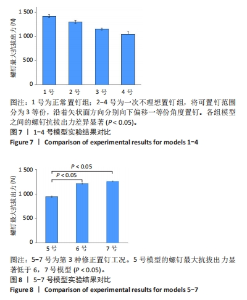
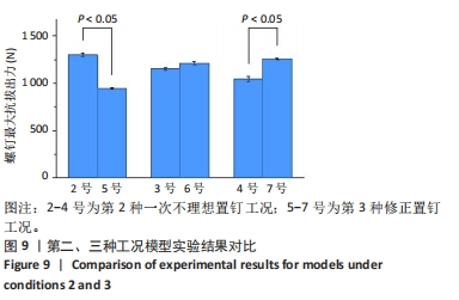
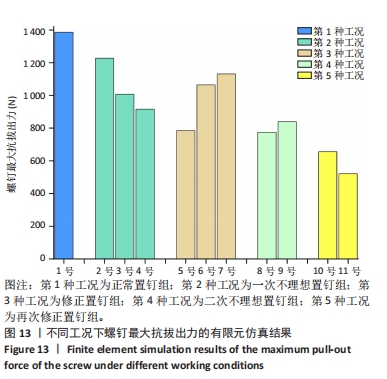
2.1 生物力学实验结果分析 考虑到实验装置中包含多个弹性组件和夹具容器内的轻微滑动,根据KUENY等[18]的方法,实验测得的拔出力数值进行了30%的校正。在正常置钉工况中,1号模型展示了单次正常置钉时的最大抗拔出力为(1 422.63±23.80) N。在一次不理想置钉工况中,2号模型的抗拔出力为(1 300.83±32.08) N,3号模型为(1 153.13±26.75) N,4号模型为(1 048.83±45.66) N。根据图7的数据分析,单次置钉时,1号模型显示出最高的抗拔出力,而随着置钉偏移角度的增大,这一值逐渐减小。各组模型之间的抗拔出力差异显著(P < 0.05),尤其是4号模型的抗拔出力最低。如图8所示,和不理想钉道重合最少的7号模型展示了最高的螺钉最大抗拔出力,为(1 257.43±13.03) N,且随着和不理想钉道重合范围的减小,模型的最大抗拔出力呈现增加趋势。具体来看,6号模型的最大抗拔出力为(1 212.87±30.18) N,略低于7号模型但差异不显著(P > 0.05);而5号模型的最大抗拔出力为(944.77±20.29) N,显著低于6号模型(P < 0.05)。"

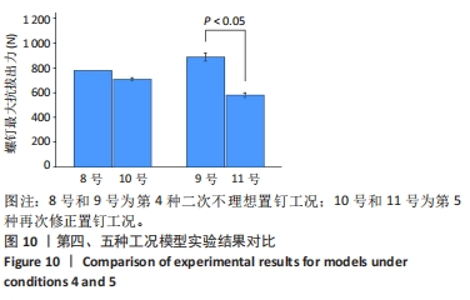
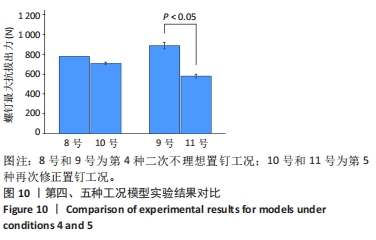
对比第4种工况的二次不理想置钉组和第5种工况的再次修正置钉组,如图10所示,两种工况下8-11号4组模型的抗拔出力分别为(780.73±31.50),(888.07±50.40),(707.70±20.30),(580.07±35.00) N。对比结果显示,当二次不理想置钉偏移角度为8号模型时,重新置钉的10号模型螺钉抗拔出力下降了9%(P > 0.05)。偏移角度进一步增至9号模型时,重新置钉的11号模型抗拔出力显著下降了35%(P < 0.05)。综合以上结果,可以得出结论:随着不理想置钉时留下的钉道数量增加以及前次置钉和拔出对骨组织产生的微裂纹和应力集中的影响,导致重新置钉后螺钉与骨之间的啮合面积减少,骨组织的强度和韧性下降,进而降低了螺钉的抗拔出力,即不更换螺钉情况下不建议进行第3次置钉。"
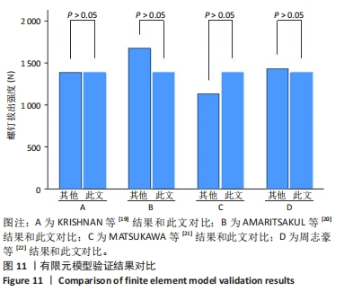
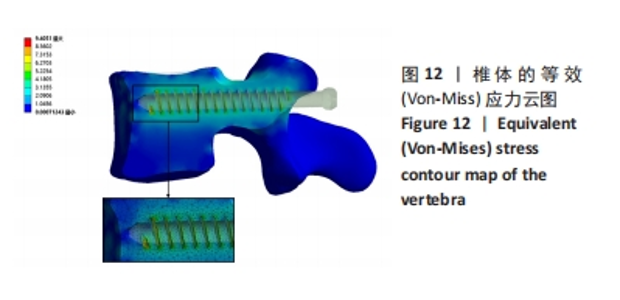
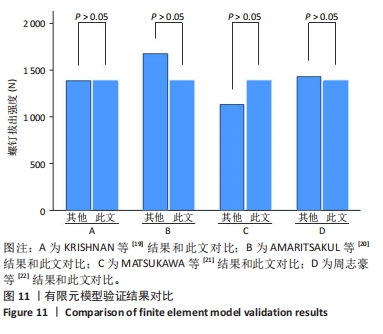
2.2 有限元模拟结果 2.2.1 模型验证 对建立的有限元模型进行有效性验证,将该模型正常置钉情况下得出的结果与KRISHNAN等[19]、AMARITSAKUL等[20]先前发表的生物力学实验结果以及MATSUKAWA等[21]、周志豪等[22]的有限元分析结果进行比较。此文计算模型采用的是基于患者 CT 数据重建的 L4椎体模型,其尺寸形状与参考文献[21]中的模型基本一致都是采用的L4椎体。针对材料参数定义和网格划分,此文皮质骨和松质骨泊松比分别定义未0.3和0.2以及划分了(16-25)×104的实体网格数量,而文献[21]采用的是Hounsfield单位值定义法,泊松比都定义为0.4且划分了实体单元数(80-100)×104个。这些差异可能会导致此文计算结果与参考文献结果存在一定差别。但是,由图11可以看出此文所建立的模型验证结果和前人发表的结果整体趋势还是一致的,数据之间没有显著差异(P > 0.05),由此可以证明模型是合理的。"
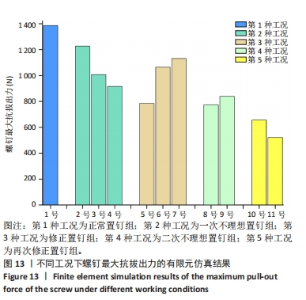
所有有限元仿真结果均基于符合骨密度破坏准则的数据得出。完成一组椎体模型拔出实验的有限元分析需要20-38 h,每次模拟的计算周期数在(40-110)×104之间。在螺钉完全插入情况下,5种工况共计11组模型,有限元仿真结果分别为1 386.1 N(1号模型)、1 227.4 N(2号模型)、1 006.7 N(3号模型)、915.68 N(4号模型)、784.48 N (5号模型)、1 064 N(6号模型)、1 131.1 N(7号模型)、773.89 N(8号模型)、838.98 N(9号模型)、656.01 N(10号模型)、521.07 N(11号模型)。如图13所示:在第一、二种工况下,2-4号模型中由于钉道倾斜,螺钉与椎弓根的接触面积发生了改变。与正常置钉的1号模型相比,2-4号模型的钉道与松质骨的接触面积有所增加,而与皮质骨的接触面积则有所减少。但是,由于松质骨强度较低,因此对螺钉的固定作用有限。此外,钉道倾斜导致螺钉受力方向发生变化,螺钉在松质骨上承受的拉力更大,而与皮质骨的接触面积减少,导致螺钉的固定效果减弱,螺钉的抗拔出力呈现下降趋势;对比第二、三种工况,随着不理想钉道偏移角度的增加,修正置钉后的钉道与不理想钉道重合面积减小,导致螺钉固定效果增强,螺钉的抗拔出力呈上升趋势;对比第四、五种工况,随着不理想钉道数量增加,导致骨钉的啮合面积减少,从而使得螺钉的抗拔出力降低。"
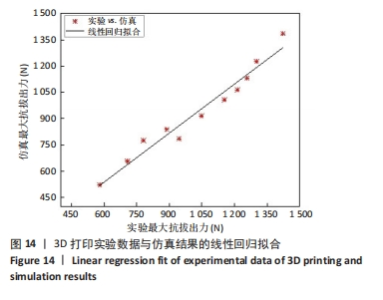
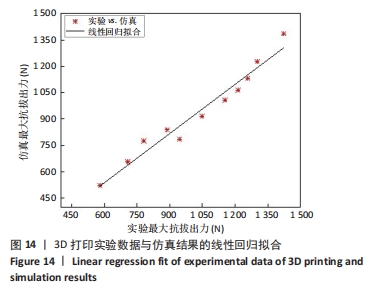
2.2.3 3D打印实验与仿真结果对比 将3D打印实验数据与仿真结果进行线性回归拟合,得到如下回归曲线: Fmax,仿真=-21.84+0.93*Fmax,实验 其中Fmax,仿真为仿真结果的最大拔出强度,Fmax,实验为实验结果的最大拔出强度。如图14所示,实验得出的拔出强度与有限元模拟得出的拔出强度具有较高的相关性,相关系数为ρ=0.98,R2=0.96。由于3D打印实验模型材料参数与有限元模型材料参数存在差异,这可能会对实验结果和数值计算结果的比较造成影响。从回归系数来看,尽管材料参数存在差异,总体上3D打印实验结果和仿真模拟结果有很好的一致性。根据Shapiro-Wilk检验结果(P > 0.05),假设数据的残差为正态分布,并进行配对t检验。结果表明,3D打印实验的螺钉最大拔出强度为(1 027±263) N,仿真结果为(936±256) N,两种方法的结果无显著差异(P > 0.05)。"
| [1] PEI B, XU Y, ZHAO Y, et al. Biomechanical comparative analysis of conventional pedicle screws and cortical bone trajectory fixation in the lumbar spine: An in vitro and finite element study. Front Bioeng Biotechnol. 2023;11:1060059. [2] ROY-CAMILLE R, ROY-CAMILLE M, DEMEULENAERE C. Osteosynthesis of dorsal, lumbar, and lumbosacral spine with metallic plates screwed into vertebral pedicles and articular apophyses. Presse Med (1893). 1970;78(32):1447-1448. [3] LI JC, YANG ZQ, XIE TH, et al. Deterioration of the fixation segment’s stress distribution and the strength reduction of screw holding position together cause screw loosening in ALSR fixed OLIF patients with poor BMD. Front Bioeng Biotechnol. 2022;30;10:922848. [4] ROY-CAMILLE R, SAILLANT G, MAZEL C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;(203): 7-17. [5] YANG JX, LUO L, LIU JH, et al. Incomplete insertion of pedicle screws triggers a higher biomechanical risk of screw loosening: mechanical tests and corresponding numerical simulations. Front Bioeng Biotechnol. 2024;11:1282512. [6] BOKOV A, BULKIN A, ALEYNIK A, et al. Pedicle Screws Loosening in Patients With Degenerative Diseases of the Lumbar Spine: Potential Risk Factors and Relative Contribution. Global Spine J. 2019;9(1):55-61. [7] 吴龙,谢成龙,林仲可.椎弓根螺钉设计与其生物力学稳定性的研究进展[J].脊柱外科杂志,2019,17(6):431-435. [8] SARAF SK, SINGH RP, SINGH V, et al. Pullout strength of misplaced pedicle screws in the thoracic and lumbar vertebrae - A cadaveric study. Indian J Orthop. 2013;47(3):238-243. [9] KANG DG, LEHMAN RA JR, WAGNER SC, et al. Pedicle screw reinsertion using previous pilot hole and trajectory does not reduce fixation strength. Spine. 2014;39(20):1640-1647. [10] GODA Y, HIGASHINO K, TOKI S, et al. The Pullout Strength of Pedicle Screws Following Redirection After Lateral Wall Breach or End-plate Breach. Spine (Phila Pa 1976). 2016;41(15):1218-1223. [11] 杜心如,叶启彬,赵玲秀,等. 腰椎人字嵴顶点椎弓根螺钉进钉方法的解剖学研究[J]. 中国临床解剖学杂志,2002,20(2):86-88. [12] 余世浩,周胜. 3D打印成型方向和分层厚度的优化[J]. 塑性工程学报,2015,22(6):7-10,39. [13] WEISER L, SELLENSCHLOH K, PÜSCHEL K, et al. Cortical threaded pedicle screw improves fatigue strength in decreased bone quality. Eur Spine J. 2021;30(1):128-135. [14] LJUSTINA G, FAGERSTRÖM M, LARSSON R. Rate sensitive continuum damage models and mesh dependence in finite element analyses. Sci World J. 2014;2014:260571. [15] BIANCO RJ, ARNOUX PJ, WAGNAC E, et al. Minimizing Pedicle Screw Pullout Risks: A Detailed Biomechanical Analysis of Screw Design and Placement. Clin Spine Surg. 2017;30(3):226-232. [16] CHATZISTERGOS PE, MAGNISSALIS EA, KOURKOULIS SK. A parametric study of cylindrical pedicle screw design implications on the pullout performance using an experimentally validated finite-element model. Med Eng Phys. 2010;32(2):145-154. [17] WIDMER J, FASSER MR, CROCI E, et al. Individualized prediction of pedicle screw fixation strength with a finite element model. Comput Methods Biomech Biomed Engin. 2020;23(4):155-167. [18] KUENY RA, KOLB JP, LEHMANN W, et al. Influence of the screw augmentation technique and a diameter increase on pedicle screw fixation in the osteoporotic spine: pullout versus fatigue testing. Eur Spine J. 2014;23(10):2196-2202. [19] KRISHNAN V, VARGHESE V, KUMAR GS. Comparative Analysis of Effect of Density, Insertion Angle and Reinsertion on Pull-Out Strength of Single and Two Pedicle Screw Constructs Using Synthetic Bone Model. Asian Spine J. 2016;10(3):414-421. [20] AMARITSAKUL Y, CHAO CK, LIN J. Comparison study of the pullout strength of conventional spinal pedicle screws and a novel design in full and backed-out insertions using mechanical tests. Proc Inst Mech Eng H. 2014;228(3):250-257. [21] MATSUKAWA K, YATO Y, HYNES RA, et al. Comparison of Pedicle Screw Fixation Strength Among Different Transpedicular Trajectories: A Finite Element Study. Clin Spine Surg. 2017;30(7):301-307. [22] 周志豪,阿拉法特·卡哈尔,王轶希,等.传统椎弓根螺钉与改良皮质骨轨迹置钉技术的生物力学性能有限元分析[J].中国组织工程研究,2022,26(18):2789-2794. [23] TANASANSOMBOON T, KITTIPIBUL T, LIMTHONGKUL W, et al. Thoracolumbar Burst Fracture without Neurological Deficit: Review of Controversies and Current Evidence of Treatment. World Neurosurg. 2022;162:29-35. [24] DERINCEK A, WU C, MEHBOD A, et al. Biomechanical comparison of anatomic trajectory pedicle screw versus injectable calcium sulfate graft-augmented pedicle screw for salvage in cadaveric thoracic bone. J Spinal Disord Tech. 2006;19(4):286-291. [25] HSIEH MK, LI YD, LI YC, et al. Improved fixation stability for repairing pedicle screw loosening using a modified cement filling technique in porcine vertebrae. Sci Rep. 2022;12(1):2739. [26] LI YD, LAI PL, HSIEH MK, et al. Influence of various pilot hole profiles on pedicle screw fixation strength in minimally invasive and traditional spinal surgery: a comparative biomechanical study. Front Bioeng Biotechnol. 2024;12:1359883. [27] HU Y, CHEN X, CHU Z, et al. Biomechanical Properties of Novel Porous Scaffold Core and Hollow Lateral Hole Pedicle Screws: A Comparative Study in Bama Pigs. Orthop Surg. 2024;16(7):1718-1725. [28] PATEL PS, SHEPHERD DE, HUKINS DW. The effect of screw insertion angle and thread type on the pullout strength of bone screws in normal and osteoporotic cancellous bone models. Med Eng Phys. 2010;32(8):822-828. [29] TAI CL, CHEN WP, LIU MY, et al. Biomechanical comparison of pedicle screw fixation strength among three different screw trajectories using single vertebrae and one-level functional spinal unit. Front Bioeng Biotechnol. 2022;10:1054738. [30] YE YX, HUANG DG, HAO DJ, et al. Screw Pullout Strength After Pedicle Screw Reposition: A Finite Element Analysis. Spine (Phila Pa 1976). 2023;48(22):382-388. [31] KALEMCI O, KIZMAZOGLU C, OZYORUK S, et al. What is the Effect of Pedicle Screw Reinsertion Through the Same Trajectory on Pullout Strength? Turk Neurosurg. 2022;32(4):635-640. [32] LI YD, LAI PL, HSIEH MK, et al. Influence of various pilot hole profiles on pedicle screw fixation strength in minimally invasive and traditional spinal surgery: a comparative biomechanical study. Front Bioeng Biotechnol. 2024;12:1359883. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Su Lintao, Jiang Jianfeng, Ma Jun, Huang Liangliang, Lei Changyu, Han Yaozheng, Kang Hui. Precise application of O-arm navigation system in thoracolumbar fractures with developmental pedicle stenosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1855-1862. |
| [3] | Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904. |
| [4] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [5] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [6] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [7] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [8] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [9] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [10] | Zhang Debao, Wang Peng, Li Kun, Zhang Shaojie, Li Zhijun, Li Shuwen, Wu Yimin. Epidural fibrous scar formation in rabbits following autologous ligamentum flavum intervention [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1168-1175. |
| [11] | Li Shuai, Liu Hua, Shang Yonghui, Liu Yicong, Zhao Qihang, Liu Wen. Stress distribution on the maxilla when wearing the Twin-block appliance for Class II malocclusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 881-887. |
| [12] | Zhou Zonghao, Luo Siyang, Chen Jiawen, Chen Guangneng, Feng Hongchao. Finite element analysis of bioabsorbable plates versus miniature titanium plates in mandibular fracture fixation in different bone qualities [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 818-826. |
| [13] | Chen Yilong, Zhang Xu, Li Hong. Mechanical analysis of fiber post combined with different crown restorations for endodontically treated non-carious cervical lesions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 866-871. |
| [14] | Song Xubin, Wu Dou, Zhao Enzhe, Zhang Xingyu, Zhang Xiaolun, Wang Chuheng. Finite element analysis of a new femoral neck spiral blade system to treat femoral intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7041-7047. |
| [15] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||