Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (28): 6146-6160.doi: 10.12307/2025.469
Meta-analysis of wearable device interventions to promote physical activity in older adults
Wang Jinfu, Yang Guan
- School of Physical Education, South China University of Technology, Guangzhou 510641, Guangdong Province, China
-
Received:2024-05-08Accepted:2024-07-08Online:2025-10-08Published:2024-12-09 -
Contact:Yang Guan, PhD, Associate professor, Master’s supervisor, School of Physical Education, South China University of Technology, Guangzhou 510641, Guangdong Province, China -
About author:Wang Jinfu, Master candidate, School of Physical Education, South China University of Technology, Guangzhou 510641, Guangdong Province, China -
Supported by:Guangdong Provincial Philosophy and Social Science Joint Construction Project, No. GD22XTY01 (to YG); Guangzhou City Philosophy and Social Science Joint Construction Topic, No. 2023GZGJ327 (to YG); General Project of Guangzhou City Science and Technology Bureau, No. 2023A04J1822 (to YG)
CLC Number:
Cite this article
Wang Jinfu, Yang Guan. Meta-analysis of wearable device interventions to promote physical activity in older adults[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 6146-6160.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
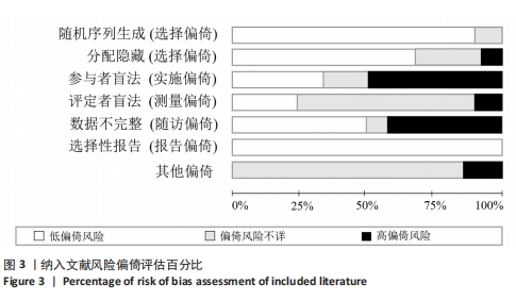
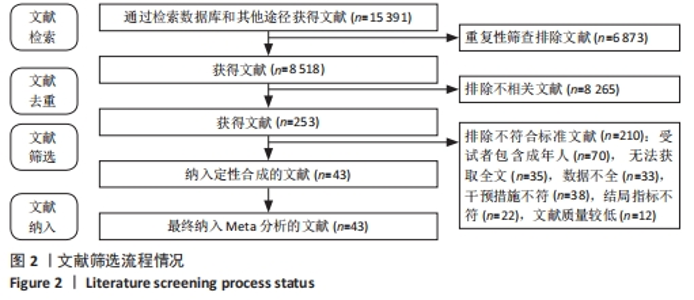
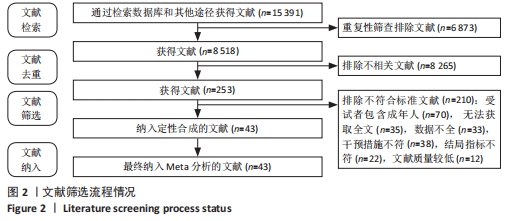
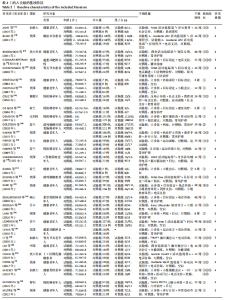
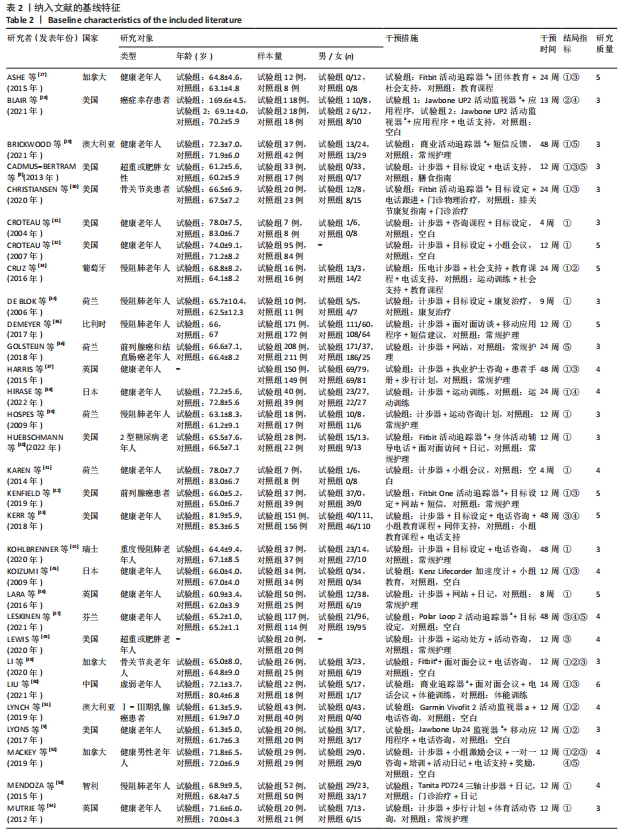
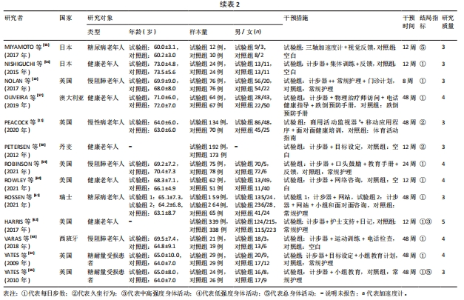
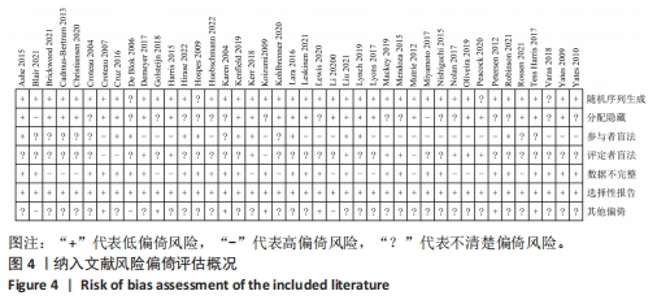
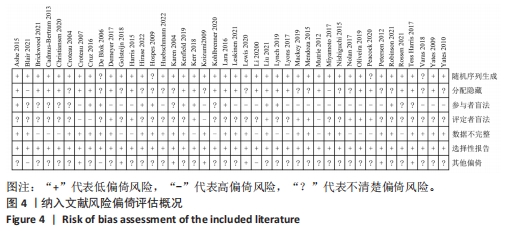
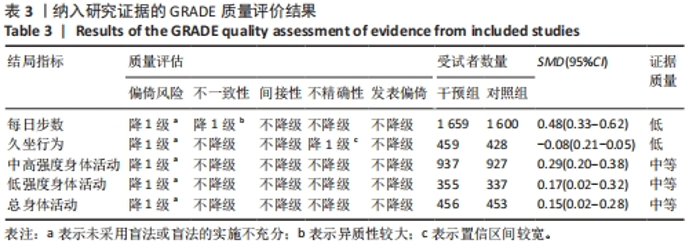
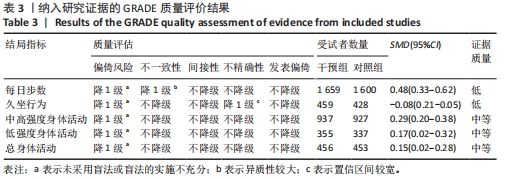
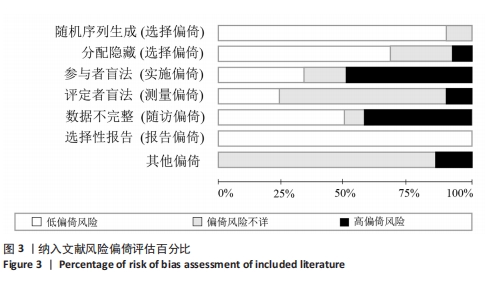
2.3 文献质量评价结果 纳入的43项研究均对参与者的基线情况进行报道,均提及“随机分配”,其中39项研究报告具体的随机方法(包括计算机生成的随机数字、信封)[8-10,27-33,35-38,40-62,64-65],23项研究描述具体的分配隐藏方案[8-9,11,27,29-30,32-33,35,37,42-43,45-47,49-51,54,57,61-62,64],11项研究对受试者实施盲法[27,33-34,38-39,42-43,46,50-51,59],9项研究对试验人员和结果评估人员实施盲法[10-11,35,37,43,50,52-53,57],28项研究数据报告完整[27-28,31-35,38-42,44,46-48,50,52-53,55-56,58-60,62-65],均对缺失结果数据或缺失原因进行描述,42项研究均无失实报道[8-11,27-65]。 根据Cochrane偏倚风险评估工具的文献质量评分,9项研究为高质量文献[27,32-33,35,42-43,46,50,62],34项研究为中等质量文献[8-11,28-31,34,36-41,44-45,47-49,51-61,63-65],见图3,4。Cohen’s kappa检验表明,2位评价者在文献质量评价结果上具有较好一致性,Cohen’s kappa系数为0.84。"
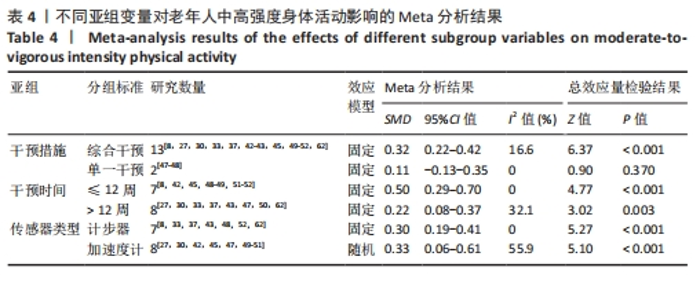
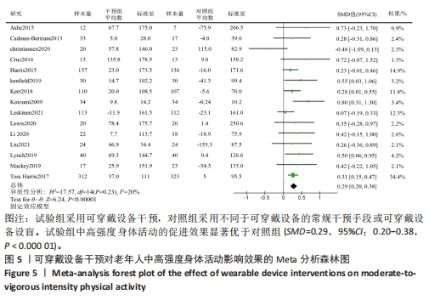
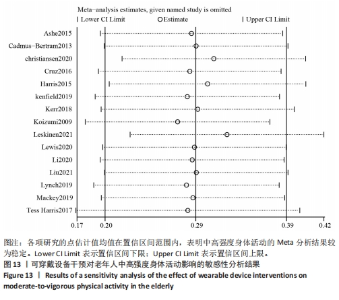
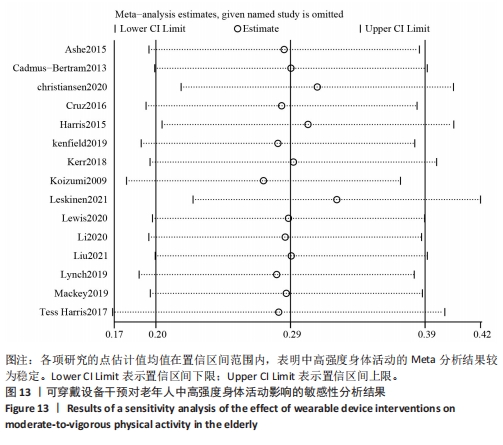
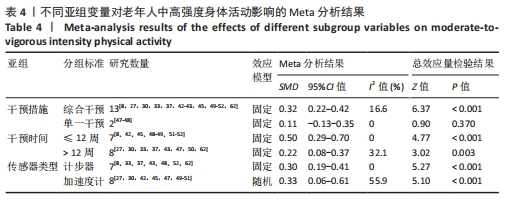
2.5 亚组分析结果 为进一步探究可穿戴设备对老年人身体活动表现的最佳设计策略,根据已有相关研究,选择干预措施、干预时间以及可穿戴设备的传感器类型[24,66],对老年人中高强度身体活动、低强度身体活动、总身体活动和每日步数4个身体活动指标进行亚组分析,而久坐行为由于所有亚组结果均无显著意义,因此没有进行深入分析。 2.5.1 两组中高强度身体活动差异的亚组Meta分析结果 将干预措施分为综合干预和单一干预2个亚组。综合干预定义为可穿戴设备作为联合人工(如团体信息会议、咨询、电话支持等)的组成部分;单一干预定义为独立于人工进行基于可穿戴设备的干预[24]。亚组分析结果显示(表4)。与单一干预相比(SMD=0.11,95%CI:-0.13-0.35,P=0.37),综合干预(SMD=0.32,95%CI:0.22-0.42,P < 0.001)对老年人中高强度身体活动有更加显著的促进效果。将干预时间分为干预时间≤12周和> 12周2个亚组,结果显示,与对照组相比,干预时间≤12周(SMD=0.50,95%CI:0.29-0.70,P < 0.001)或> 12周(SMD=0.22,95%CI:0.08-0.37,P=0.003)均能显著增加老年人的中高强度身体活动水平。将传感器类型分为加速度计和计步器2个亚组。计步器定义为用于记录个体所走的步数的一种便携式电子设备;加速度计定义为通过使用算法测量加速度力,可以用于准确检测个体身体活动的周期和强度的电子追踪器[67]。结果显示,与对照组相比,使用加速度计干预(SMD=0.33,95%CI:0.06-0.61,P < 0.001)或计步器干预(SMD=0.30,95%CI:0.19-0.41,P < 0.001)均能显著增加老年人中高强度身体活动水平。"
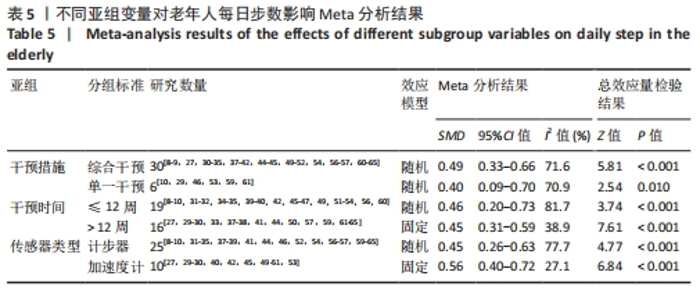
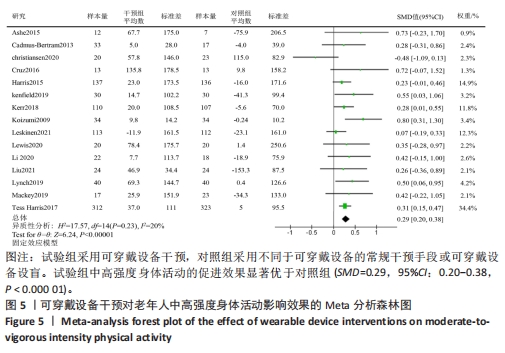
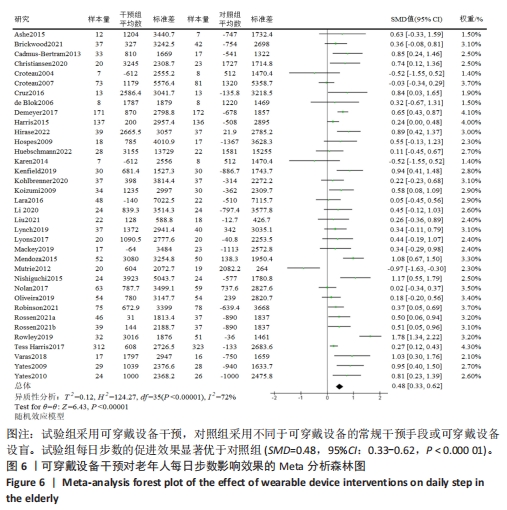
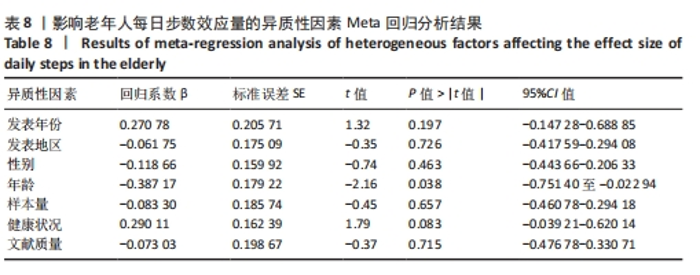
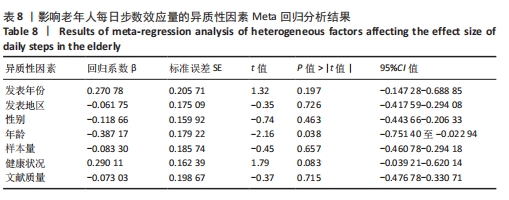
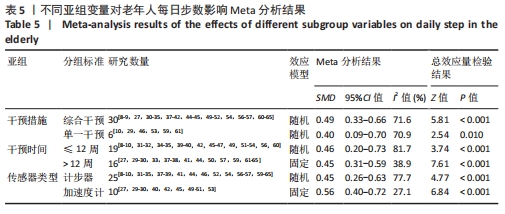
2.5.2 两组每日步数差异的亚组Meta分析结果 亚组分析结果显示(表5),对于干预措施,综合干预(SMD=0.49,95%CI:0.33-0.66,P < 0.001)或单一干预(SMD=0.40,95%CI:0.09-0.70,P=0.01)均能显著促进老年人的每日步数;对于干预时间,干预时间≤12周(SMD=0.46,95%CI:0.20-0.73,P < 0.001)或> 12周(SMD=0.45,95%CI:0.31-0.59,P < 0.001)均能显著促进老年人的每日步数;对于传感器类型,使用加速度计干预(SMD=0.56,95%CI:0.40-0.72,P < 0.001)或计步器干预(SMD=0.45,95%CI: 0.26-0.63,P < 0.001)均能显著增加老年人的每日步数。"
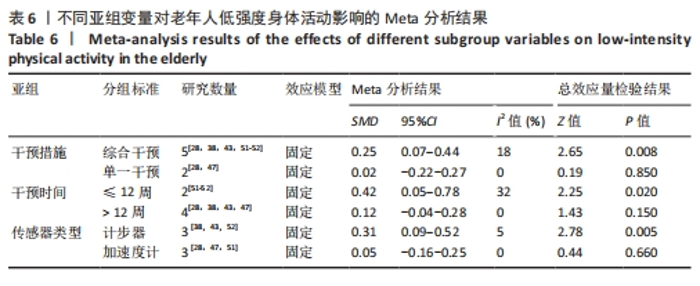
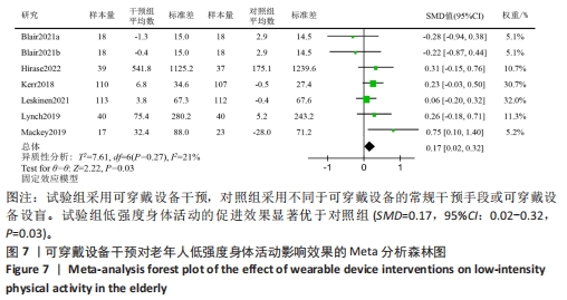
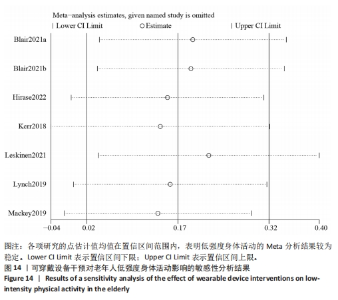
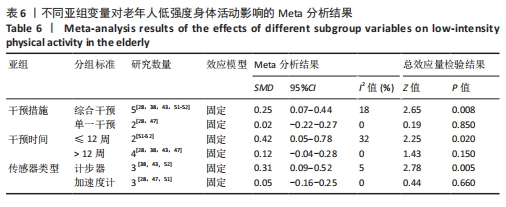
2.5.3 两组低强度身体活动差异的亚组Meta分析结果 亚组分析结果显示(表6),对于干预措施,与单一干预相比(SMD=0.02,95%CI:-0.22-0.27,P=0.850),综合干预(SMD=0.25,95%CI:0.07-0.44, P=0.008)对老年人低强度身体活动有更显著促进效果;对于干预时间,与干预时间> 12周相比(SMD=0.12,95%CI:-0.04-0.28,P=0.15),干预时间≤12周(SMD=0.42,95%CI:0.05-0.78,P=0.02)对老年人低强度身体活动有更显著促进效果;对于传感器类型,与加速度计相比(SMD=0.05,95%CI:-0.16-0.25,P=0.66),计步器(SMD=0.31,95%CI:0.09-0.52,P=0.005)干预对老年人低强度身体活动有更显著促进效果。"
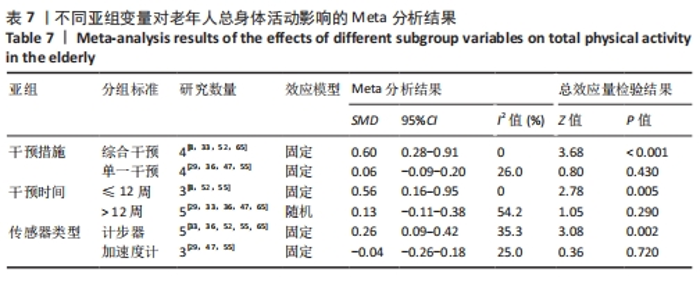
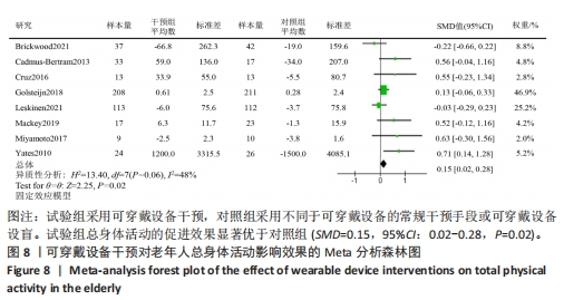
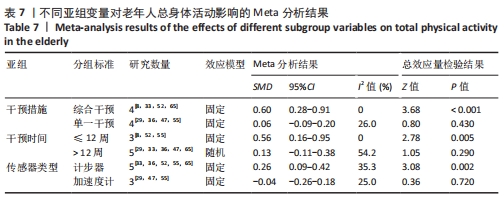
2.5.4 两组总身体活动差异的亚组Meta分析结果 亚组分析结果显示(表7),对于干预措施,与单一干预相比(SMD=0.06,95%CI:-0.09-0.20,P=0.43),综合干预(SMD=0.60,95%CI:0.28-0.91,P < 0.001)对老年人总身体活动有更加显著的促进效果;对于干预时间,与干预时间> 12周相比(SMD=0.13,95%CI:-0.11-0.38,P=0.29),干预时间≤12周(SMD=0.56,95%CI:0.16-0.95,P=0.005)对老年人总身体活动有更加显著的促进效果;对于传感器类型,与加速度计相比(SMD=-0.04,95%CI:-0.26-0.18,P=0.72),计步器(SMD=0.26,95%CI:0.09-0.42,P=0.002)干预对老年人总身体活动有更显著促进效果。"
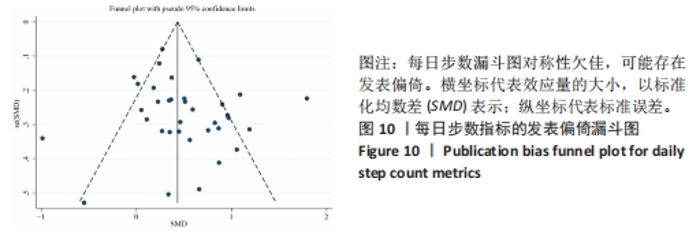
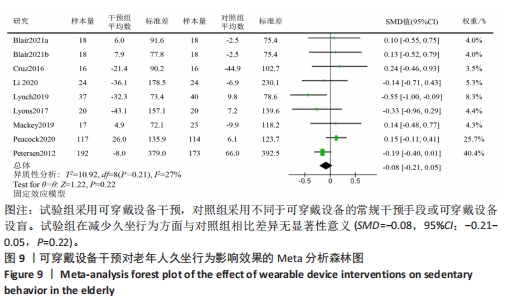
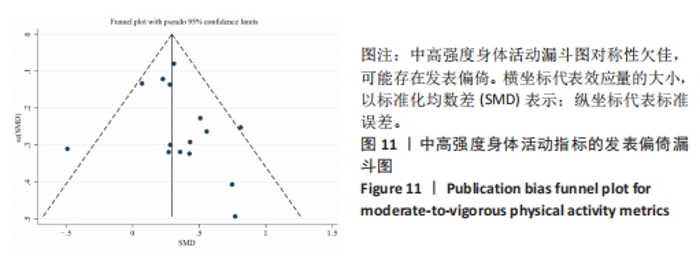
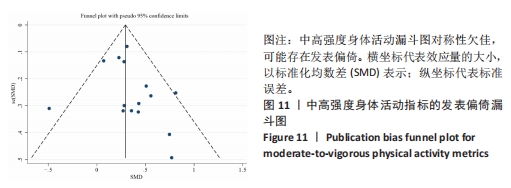
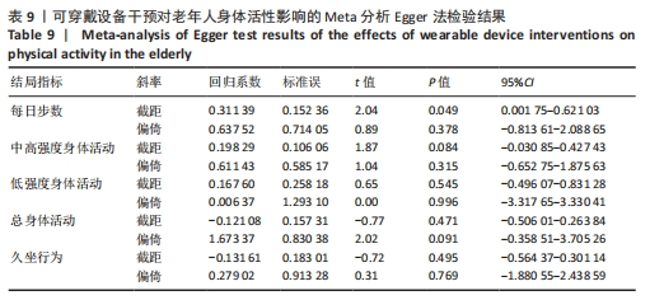
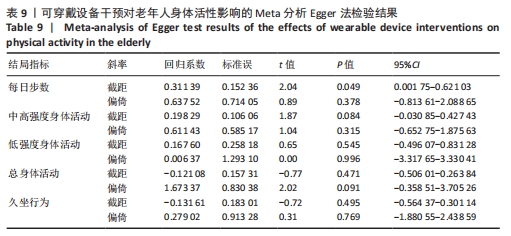
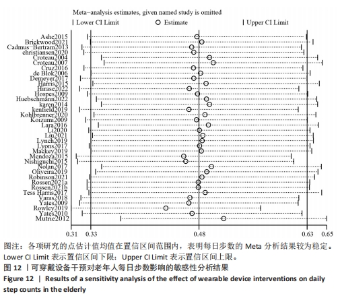
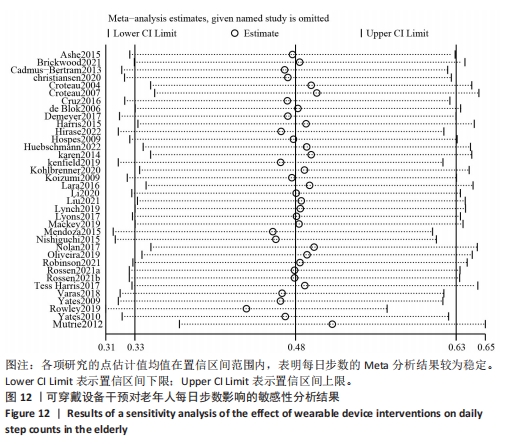
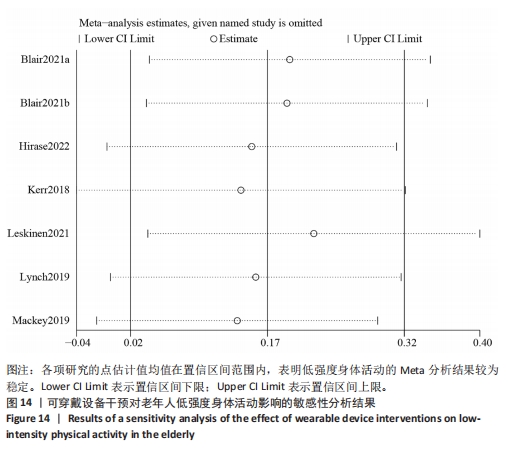
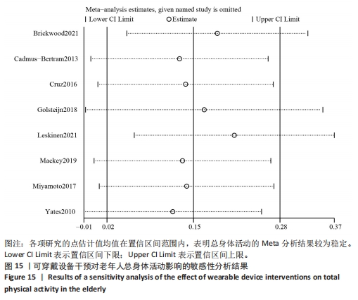
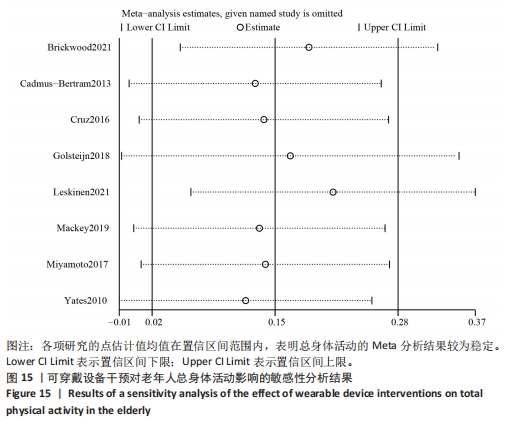
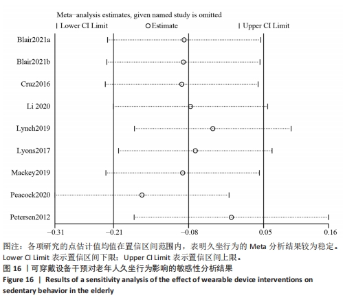
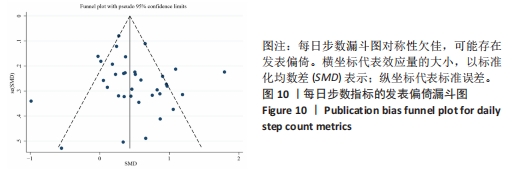
2.6 发表偏倚评价和敏感性分析结果 采用定量和定性的方法对纳入文献的发表偏倚进行评估。依据先前的研究经验,绘制漏斗图至少需10项研究数据,并且仅通过直观检查漏斗图可能得出错误的结论[69]。因此,文章联合使用Egger检验对纳入研究的发表偏倚进行定量分析,具体而言,针对报告每日步数和中高强度身体活动的研究,同时进行了Egger检验和漏斗图分析;针对低强度身体活动、总身体活动和久坐行为的研究,则仅执行了Egger检验。分析结果显示,每日步数和中高强度身体活动的漏斗图对称性欠佳,提示可能存在发表偏倚,见图10,11。然而Egger检验结果显示,所有指标P > 0.05,见表9,表明纳入的所有研究不存在发表偏倚。"
| [1] AMUTHAVALLI THIYAGARAJAN J, MIKTON C, HARWOOD RH, et al. The UN Decade of healthy ageing: strengthening measurement for monitoring health and wellbeing of older people. Age Ageing. 2022;51(7):afac147. [2] CHEN X, GILES J, YAO Y, et al. The path to healthy ageing in China: a Peking University-Lancet Commission. Lancet. 2022;400(10367):1967-2006. [3] STENSEL DJ. How can physical activity facilitate a sustainable future? Reducing obesity and chronic disease. Proc Nutr Soc. 2023;82(3):286-297. [4] D’ONOPRIO G, KIRSCHNER J, PRATHER H, et al. Musculoskeletal exercise: Its role in promoting health and longevity. Prog Cardiovasc Dis. 2023;77(4):25-36. [5] GOMES M, FIGUEIREDO D, TEIXEIRA L, et al. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing. 2017;46(1):71-79. [6] ZHOU Y, WU J, ZHANG S, et al. Prevalence and risk factors of physical inactivity among middle-aged and older Chinese in Shenzhen: a cross-sectional study. BMJ Open. 2018;8(10):e019775. [7] LEWIS ZH, LYONS EJ, JARVIS JM, et al. Using an electronic activity monitor system as an intervention modality: A systematic review. BMC Public Health. 2015;15(6):585-600. [8] CADMUS-BERTRAM L, WANG JB, PATTERSON RE, et al. Web-based self-monitoring for weight loss among overweight/obese women at increased risk for breast cancer: the HELP pilot study. Psycho-Oncol. 2013; 22(8):1821-1829. [9] LYONS EJ, SWARTZ MC, LEWIS ZH, et al. Feasibility and Acceptability of a Wearable Technology Physical Activity Intervention With Telephone Counseling for Mid-Aged and Older Adults: A Randomized Controlled Pilot Trial. JMIR Mhealth Uhealth. 2017; 5(3):e28. [10] NOLAN CM, MADDOCKS M, CANAVAN JL, et al. Pedometer Step Count Targets during Pulmonary Rehabilitation in Chronic Obstructive Pulmonary Disease. A Randomized Controlled Trial. Am J Respir Crit Care Med. 2017;195(10):1344-1352. [11] PEACOCK OJ, WESTERN MJ, BATTERHAM AM, et al. Effect of novel technology-enabled multidimensional physical activity feedback in primary care patients at risk of chronic disease-The MIPACT study: A randomised controlled trial. Int J Behav Nutr Phys Act. 2020;17(1):156-172. [12] BLOUNT DS, MCDONOUGH DJ, GAO Z. Effect of Wearable Technology-Based Physical Activity Interventions on Breast Cancer Survivors’ Physiological, Cognitive, and Emotional Outcomes: A Systematic Review. J Clin Med. 2021;10(9):2015-2034. [13] GAL R, MAY AM, VAN OVERMEEREN EJ, et al. The Effect of Physical Activity Interventions Comprising Wearables and Smartphone Applications on Physical Activity: a Systematic Review and Meta-analysis. Sports Med Open. 2018;4(1):42-48. [14] CHEATHAM SW, STULL KR, FANTIGRASSI M, et al. The efficacy of wearable activity tracking technology as part of a weight loss program: a systematic review. J Sports Med Phys Fitness. 2018;58(4):534-548. [15] OLIVEIRA J, SHERRINGTON C, ZHENG E, et al. Effect of interventions using physical activity trackers on physical activity in people aged 60 years and over: a systematic review and meta-analysis. Br J Sports Med. 2020;54(20):1188-1194. [16] COOPER C, GROSS A, BRINKMAN C, et al. The impact of wearable motion sensing technology on physical activity in older adults. Exp Gerontol. 2018;112(1):9-19. [17] PALUCH AE, BAJPAI S, BASSETT DR, et al. Daily steps and all-cause mortality: a meta-analysis of 15 international cohorts. Lancet Public health. 2022;7(3):e219-e228. [18] FISHMAN EI, STEEVES JA, ZIPUNNUKOV V, et al. Association between Objectively Measured Physical Activity and Mortality in NHANES. Med Sci Sports Exerc. 2016; 48(7):1303-1311. [19] BALLIN M, NORDSTROM P, NIKLASSON J, et al. Associations of Objectively Measured Physical Activity and Sedentary Time with the Risk of Stroke, Myocardial Infarction or All-Cause Mortality in 70-Year-Old Men and Women: A Prospective Cohort Study. Sports Med. 2021;51(2):339-349. [20] HIGGINS JP, ALTMAN DG, GØTZSCHE PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [21] GUYATT GH, OXMAN AD, SCHüNEMANN HJ, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4): 380-382. [22] 吴洋,王宇,李柏辰,等.疏肝解郁法治疗冠心病合并抑郁的Meta分析及GRADE评价[J].中西医结合心脑血管病杂志,2024,22(9):1547-1554. [23] WAN X, WANG W, LIU J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135-148. [24] BRICKWOOD KJ, WATSON G, O’BRIEN J, et al. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth. 2019;7(4):e11819. [25] HIGGINS JP, THOMPSON SG, DEEKS JJ, et al. Measuring inconsistency in Meta-analyse. BMJ. 2003;327:557-560. [26] MCHUGH ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276-282. [27] ASHE MC, WINTERS M, HOPPMANN CA, et al. “Not just another walking program”: Everyday Activity Supports You (EASY) model-a randomized pilot study for a parallel randomized controlled trial. Pilot Feasibility Stud. 2015;1(1):367-379. [28] BLAIR CK, HARDING E, WIGGINS C, et al. A home-based mobile health intervention to replace sedentary time with light physical activity in older cancer survivors: Randomized controlled pilot trial. JMIR Cancer. 2021;7(2):281-295. [29] BRICKWOOD KJ, AHUJA KDK, WATSON G, et al. Effects of activity tracker use with health professional support or telephone counseling on maintenance of physical activity and health outcomes in older adults: Randomized controlled trial. JMIR Mhealth Uhealth. 2021;9(1):369-382. [30] CHRISTIANSEN MB, THOMA LM, MASTER H, et al. Feasibility and Preliminary Outcomes of a Physical Therapist-Administered Physical Activity Intervention After Total Knee Replacement. Arthritis Care Res. 2020; 72(5):661-668. [31] CROTEAU KA, RICHESON NE, VINES SW, et al. Effects of a Pedometer-Based Physical Activity Program on Older Adults’ Mobility-Related Self-Efficacy and Physical Performance. Act Adapt Aging. 2004;28(2):19-33. [32] CROTEAU KA, RICHESON NE, FARMER BC, et al. Effect of a pedometer-based intervention on daily step counts of community-dwelling older adults. Res Q Exerc Sport. 2007;78:401-406. [33] CRUZ J, BROOKS D, MARQUES A. Walk2Bactive: A randomized controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary disease. Chron Respir Dis. 2016; 13(1):57-66. [34] DE BLOK BM, DE GREEF MHG, TEN HACKEN NHT, et al. The effects of a lifestyle physical activity counseling program with feedback of a pedometer during pulmonary rehabilitation in patients with COPD: a pilot study. Patient Educ Couns. 2006;61(1):48-55. [35] DEMEYER H, LOUVARIS Z, FREI A, et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: a multicentre randomised controlled trial. Thorax. 2017; 72(5):415-423. [36] GOLSTEIJN RHJ, BOLMAN C, VOLDERS E, et al. Short-term efficacy of a computer-tailored physical activity intervention for prostate and colorectal cancer patients and survivors: a randomized controlled trial. Int J Behav Nutr Phys Act. 2018;15(1):106. [37] HARRIS T, KERRY SM, VICTOR CR, et al. A primary care nurse-delivered walking intervention in older adults: PACE (pedometer accelerometer consultation evaluation)-Lift cluster randomised controlled trial. PLoS Med. 2015;12(2):e1001783. [38] HIRASE T, INOKUCHI S, KOSHIKAWA S, et al. Preventive effect of an intervention program with increased physical activity on the development of musculoskeletal pain in community-dwelling older adults: A randomized controlled trial. Pain Med (Malden, Mass). 2022;28(3):581-593. [39] HOSPES G, BOSSENBROEK L, TEN HACKEN NHT, et al. Enhancement of daily physical activity increases physical fitness of outclinic COPD patients: results of an exercise counseling program. Patient Educ Couns. 2009;75(2):274-281. [40] HUEBSCHMANN AG, GLASGOW RE, LEAVITT IM, et al. Integrating a physical activity coaching intervention into diabetes care: a mixed-methods evaluation of a pilot pragmatic trial. Transl Behav Med. 2022; 12(4):601-610. [41] KAREN AC, NANCY ER, SUSAN WV, et al. Effects of a pedometer-based physical activity program on older adults’ mobility-related self-efficacy and physical performance. Act Adapt Aging. 2004;28:2. [42] KENFIELD SA, VAN BLARIGAN EL, AMELI N, et al. Feasibility, Acceptability, and Behavioral Outcomes from a Technology-enhanced Behavioral Change Intervention (Prostate 8): A Pilot Randomized Controlled Trial in Men with Prostate Cancer. Eur Urol. 2019;75(6):950-958. [43] KERR J, ROSENBERG D, MILLSTEIN RA, et al. Cluster randomized controlled trial of a multilevel physical activity intervention for older adults. Int J Behav Nutr Phys Act. 2018;15(1):32-47. [44] KOHLBRENNER D, SIEVI NA, SENN O, et al. Long-term effects of pedometer-based physical activity coaching in severe copd: A randomized controlled trial. Int J COPD. 2020;15:2837-2846. [45] KOIZUMI D, ROGERS NL, ROGERS ME, et al. Efficacy of an accelerometer-guided physical activity intervention in community-dwelling older women. J Phys Act Health. 2009;6(4):467-474. [46] LARA J, O’BRIEN N, GODFREY A, et al. Pilot randomised controlled trial of a web-based intervention to promote healthy eating, physical activity and meaningful social connections compared with usual care control in people of retirement age recruited from workplaces. PLoS One. 2016;11(7):292-308. [47] LESKINEN T, SUORSA K, TUOMINEN M, et al. The Effect of Consumer-based Activity Tracker Intervention on Physical Activity among Recent Retirees-An RCT Study. Med Sci Sports Exerc. 2021;53(8):1756-1765. [48] LEWIS ZH, OTTENBACHER KJ, FISHER SR, et al. Effect of electronic activity monitors and pedometers on health: Results from the TAME health pilot randomized pragmatic trial. Int J Environ Res Public Health. 2020;17:18. [49] LI LC, FEEHAN LM, XIE H, et al. Effects of a 12-Week Multifaceted Wearable-Based Program for People With Knee Osteoarthritis: Randomized Controlled Trial. JMIR Mhealth Uhealth. 2020;8(7):e19116. [50] LIU JYW, KWAN RYC, YIN YH, et al. Enhancing the physical activity levels of frail older adults with a wearable activity tracker-based exercise intervention: A pilot cluster randomized controlled trial. Int J Environ Res Public Health. 2021;18(19):781-795. [51] LYNCH BM, NGUYEN NH, MOORE MM, et al. A randomized controlled trial of a wearable technology-based intervention for increasing moderate to vigorous physical activity and reducing sedentary behavior in breast cancer survivors: The ACTIVATE Trial. Cancer. 2019;125(16):2846-2855. [52] MACKEY DC, PERKINS AD, TAI K H, et al. Men on the move: A randomized controlled feasibility trial of a scalable, choice-based, physical activity and active transportation intervention for older men. J Aging Phys Act. 2019;27(4):489-502. [53] MENDOZA L, HORTA P, ESPINOZA J, et al. Pedometers to enhance physical activity in COPD: A randomised controlled trial. Eur Respir J. 2015;45(2):347-354. [54] MUTRIE N, DOOLIN O, FITZSIMONS CF, et al. Increasing older adults’ walking through primary care: results of a pilot randomized controlled trial. Fam Pr. 2012;29(6):633-642. [55] MIYAMOTO T, FUKUDA K, OSHIMA Y, et al. Non-locomotive physical activity intervention using a tri-axial accelerometer reduces sedentary time in type 2 diabetes. Phys Sportsmed. 2017;45(3):245-251. [56] NISHIGUCHI S, YAMADA M, TANIGAWA T, et al. A 12-Week Physical and Cognitive Exercise Program Can Improve Cognitive Function and Neural Efficiency in Community-Dwelling Older Adults: A Randomized Controlled Trial. J Am Geriatr Soc. 2015;63(7):1355-1363. [57] OLIVEIRA JS, SHERRINGTON C, PAUL SS, et al. A combined physical activity and fall prevention intervention improved mobility-related goal attainment but not physical activity in older adults: a randomised trial. J Physiother. 2019;65(1):16-22. [58] PETERSEN CB, SEVERIN M, HANSEN AW, et al. A population-based randomized controlled trial of the effect of combining a pedometer with an intervention toolkit on physical activity among individuals with low levels of physical activity or fitness. Prev Med. 2012;54:125-130. [59] ROBINSON SA, COOPER JAJR, GOLDSTEIN RL, et al. A randomised trial of a web-based physical activity self-management intervention in COPD. ERJ Open Res. 2021; 7(3):461-472. [60] ROWLEY TW, LENZ EK, SWARTZ AM, et al. Efficacy of an individually tailored, Internet-mediated physical activity intervention in older adults: A randomized controlled trial. J Appl Gerontol. 2019;38:1011-1022. [61] ROSSEN J, HAGSTROMER M, YNGVE A, et al. Process evaluation of the Sophia Step Study- a primary care based three-armed randomized controlled trial using self-monitoring of steps with and without counseling in prediabetes and type 2 diabetes. BMC Public Health. 2021;21(1):1191-1203. [62] HARRIS T, KERRY SM, LIMB ES, et al. Effect of a primary care walking intervention with and without nurse support on physical activity levels in 45- to 75-year-olds: The pedometer and consultation evaluation (PACE-UP) cluster randomised clinical trial. Plos Med. 2017;14:e1002210. [63] VARAS AB, CORDOBA S, RODRIGUEZ-ANDONAEGUI I, et al. Effectiveness of a community-based exercise training programme to increase physical activity level in patients with chronic obstructive pulmonary disease: A randomized controlled trial. Physiother Res Int. 2018;23(4):e1740. [64] YATES T, DAVIES M, GORELY T, et al. Effectiveness of a pragmatic education program designed to promote walking activity in individuals with impaired glucose tolerance: a randomized controlled trial. Diabetes Care. 2009;32(8):1404-1410. [65] YATES T, DAVIES MJ, GORELY T, et al. The effect of increased ambulatory activity on markers of chronic low-grade inflammation: evidence from the PREPARE programme randomized controlled trial. Diabet Med. 2010;27(11):1256-1263. [66] LI C, CHEN X, BI X. Wearable activity trackers for promoting physical activity: A systematic meta-analytic review. Int J Med Inform. 2021;152(5):104487-104498. [67] WU S, LI G, DU L, et al. The effectiveness of wearable activity trackers for increasing physical activity and reducing sedentary time in older adults: A systematic review and meta-analysis. Digit Health. 2023;9: 1-13. [68] 王从江.体育锻炼对我国普通大学生抑郁症影响的Meta分析[J].成都体育学院学报,2014,40(3):75-79. [69] DEBRAY TPA, MOONS KGM, RILEY RD. Detecting small-study effects and funnel plot asymmetry in meta-analysis of survival data: A comparison of new and existing tests. Res Synth Methods. 2018; 9(1):41-50. [70] ROBERTS AL, FISHER A, SMITH L, et al. Digital health behaviour change interventions targeting physical activity and diet in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2017;11(6): 704-719. [71] SAINT-MAURICE PF, TROIANO RP, BASSETT DRJR, et al. Association of Daily Step Count and Step Intensity With Mortality Among US Adults. JAMA. 2020;323(12):1151-1160. [72] D’AMORE C, REID JC, CHAN M, et al. Interventions Including Smart Technology Compared With Face-to-face Physical Activity Interventions in Older Adults: Systematic Review and Meta-analysis. J Med Internet Res. 2022;24(10):e36134. [73] LIU JY, KOR PP, CHAN CP, et al. The effectiveness of a wearable activity tracker (WAT)-based intervention to improve physical activity levels in sedentary older adults: A systematic review and meta-analysis. Arch Gerontol Geriatr. 2020;91:104211-104230. [74] EKELUND U, TARP J, FAGERLAND MW, et al. Joint associations of accelero-meter measured physical activity and sedentary time with all-cause mortality: a harmonised meta-analysis in more than 44 000 middle-aged and older individuals. Br J Sports Med. 2020;54(24):1499-1506. [75] MEH K, SEMBER V, SORIC M, et al. The dilemma of physical activity questionnaires: Fitter people are less prone to over reporting. PLos One. 2023;18(8):e0285357. [76] MICHIE S, RICHARDSON M, JOHNSTON M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81-95. [77] GAO Z, RYU S, ZHOU W, et al. Effects of personalized exercise prescriptions and social media delivered through mobile health on cancer survivors’ physical activity and quality of life. J Sport Health Sci. 2023; 12(6):705-714. [78] ISLAM KF, AWAL A, MAZUMDER H, et al. Social cognitive theory-based health promotion in primary care practice: A scoping review. Heliyon. 2023;9(4):e14889. [79] ZUBALA A, MACGILLIVRAY S, FROST H, et al. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS One. 2017;12(7):e0180902 [80] AUERSWALD T, MEYER J, VON HOLDT K, et al. Application of Activity Trackers among Nursing Home Residents-A Pilot and Feasibility Study on Physical Activity Behavior, Usage Behavior, Acceptance, Usability and Motivational Impact. Int J Environ Res Public Health. 2020;17(18):6683-6704. [81] HODKINSON A, KONTOPANTELIS E, ADENIJI C, et al. Interventions Using Wearable Physical Activity Trackers Among Adults With Cardiometabolic Conditions: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(7):e2116382. [82] LARSEN RT, CHRISTENSEN J, JUHL CB, et al. Physical activity monitors to enhance amount of physical activity in older adults - a systematic review and meta-analysis. Eur Rev Aging Phys Act. 2019;16(1):7. [83] STOCLWELL S, SCHOFIELD P, FISHER A, et al. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: A systematic review and meta-analysis. Exp Gerontol. 2019;120:68-87. |
| [1] | Zhang Xinxin, Gao Ke, Xie Shidong, Tuo Haowen, Jing Feiyue, Liu Weiguo. Network meta-analysis of non-surgical treatments for foot and ankle ability and dynamic balance in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1931-1944. |
| [2] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [3] | Zhang Yuxin, Yu Cong, Zhang Cui, Ding Jianjun, Chen Yan. Differences in postural control ability between older adults with mild cognitive impairment and those with normal cognition under different single-task and dual-task conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1643-1649. |
| [4] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [5] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [6] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [7] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [8] | Li Huijun, Li Huangyan, Zhang Yeting. Physical activity and cognition in older adults: research hotspot and topic evolution [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1073-1080. |
| [9] | Li Zhe, Li Ping, Zhang Chao, Guo Guangling. A network meta-analysis of efficacy of mesenchymal stem cells from different sources in treatment of premature ovarian failure animal models [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7898-7908. |
| [10] | Wang Kaigang, Hao Dongsheng, Ma Pei, Zhou Shuo, Li Ruimin. Comparison of efficacy of different biological scaffolds for pulp regeneration therapy in immature permanent teeth: a Bayesian network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7447-7460. |
| [11] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [12] | Wang Jianlei, He Peiliang, Sun Yongjian. A meta-analysis of clinical efficacy and safety of intravenous glucocorticoids before lower limb joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 599-607. |
| [13] | Li Jia, Liu Qianru, Xing Mengnan, Chen Bo, Jiao Wei, Meng Zhaoxiang. A network meta-analysis on therapeutic effect of different types of exercise on knee osteoarthritis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 609-616. |
| [14] | Zhou Yanjie, Cao Chunfeng, Zhang Zhongzu, Niu Xiong, Wang Xin, Yang Zaihai, Zhou Liang, Li Bo. Meta-analysis of anterior cervical decompression and fusion ROI-CTM self-locking system in treatment of degenerative cervical spondylosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 617-627. |
| [15] | Jiang Siqi, Huang Huanhuan, Yu Xinyu, Peng Ying, Zhou Wei, Zhao Qinghua. Meta-analysis of dose-effect of exercise on improving muscle health in community-dwelling older adults with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6295-6304. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||