Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1761-1767.doi: 10.12307/2025.123
Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis
Li Liangkui1, 2, Huang Yongcan2, 3, Wang Peng2, 4, Yu Binsheng2, 3
- 1Zhuhai Campus, Zunyi Medical University, Zhuhai 519041, Guangdong Province, China; 2Shenzhen Key Laboratory of Spine Surgery, Department of Spine Surgery of Peking University Shenzhen Hospital, Shenzhen 518036, Guangdong Province, China; 3Institute of Orthopedics, Shenzhen Peking University-Hong Kong University of Science and Technology Medical Center, Shenzhen 518036, Guangdong Province, China; 4Clinical College, Peking University Shenzhen Hospital, Anhui Medical University, Shenzhen 518036, Guangdong Province, China
-
Received:2023-10-07Accepted:2024-01-14Online:2025-03-28Published:2024-10-09 -
Contact:Yu Binsheng, MD, Professor, Chief physician, Master’s supervisor, Shenzhen Key Laboratory of Spine Surgery, Department of Spine Surgery of Peking University Shenzhen Hospital, Shenzhen 518036, Guangdong Province, China; Institute of Orthopedics, Shenzhen Peking University-Hong Kong University of Science and Technology Medical Center, Shenzhen 518036, Guangdong Province, China -
About author:Li Liangkui, Master candidate, Zhuhai Campus, Zunyi Medical University, Zhuhai 519041, Guangdong Province, China; Shenzhen Key Laboratory of Spine Surgery, Department of Spine Surgery of Peking University, Shenzhen Hospital, Shenzhen 518036, Guangdong Province, China -
Supported by:Shenzhen Key Laboratory of Spinal Surgery, No. ZDSYS201505051109056 (to YBS)
CLC Number:
Cite this article
Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

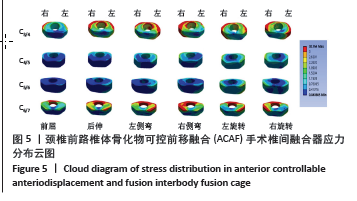
2.2 术前模型和ACAF手术模型后纵韧带骨化物应力值及应力分布 术前模型在前屈、后伸、左侧弯、右侧弯、左旋转、右旋转运动工况下后纵韧带骨化物最大应力分别为10.1,148.6,68.9,74.8,83.8,85.1 MPa。ACAF手术模型骨化物在6个运动状态下最大应力分别为14.5,38.4,26.0,27.5,28.1,27.3 MPa。2个模型骨化物应力主要集中在C4/5节段,除在前屈位ACAF手术模型骨化物应力较术前模型增大(+44.7%),而在其他5个运动方向,ACAF手术模型骨化物应力较术前模型明显降低,其中后伸位下降最明显(-74.1%)。在左侧弯、右侧弯、左旋转、右旋转骨化物应力分别下降了62.2%,63.3%,66.4%,67.9%(图3)。 2.3 内植物应力值及应力分布 2.3.1 钛板、螺钉应力值和应力分布 ACAF手术模型在前屈、后伸、左侧弯、右侧弯、左旋转、右旋转6个工况下钛板、螺钉最大应力分别为43.3,149.5,114.9,95.5,145.0及109.5 MPa,前屈应力最小,后伸应力最大,前屈和后伸应力主要分布于钛板头尾两端各1/4处;左侧弯应力主要分布于钛板右侧一半,右侧弯应力主要分布于钛板左侧一半,左旋转钛板应力呈右手螺旋分布,右旋转钛板应力呈左手螺旋分布(图4)。"

| [1] STAPLETON CJ, PHAM MH, ATTENELLO FJ, et al. Ossification of the posterior longitudinal ligament: genetics and pathophysiology. Neurosurg Focus. 2011;30(3):E6. [2] SASAKI E, ONO A, YOKOYAMA T, et al. Prevalence and symptom of ossification of posterior longitudinal ligaments in the Japanese general population. J Orthop Sci. 2014;19(3):405-411. [3] SHIN J, KIM YW, LEE SG, et al. Cohort study of cervical ossification of posterior longitudinal ligament in a Korean populations: Demographics of prevalence, surgical treatment, and disability. Clin Neurol Neurosurg. 2018;166:4-9. [4] 陈振,孙宇.颈椎后纵韧带骨化的流行病学研究进展[J].中国脊柱脊髓杂志,2017,27(5):460-464. [5] BOODY BS, LENDNER M, VACCARO AR. Ossification of the posterior longitudinal ligament in the cervical spine: a review. Int Orthop. 2019; 43(4):797-805. [6] TSUJI T, CHIBA K, HOSOGANE N, et al. Epidemiological survey of ossification of the posterior longitudinal ligament by using clinical investigation registration forms. J Orthop Sci. 2016;21(3):291-294. [7] ABIOLA R, RUBERY P, MESFIN A. Ossification of the Posterior Longitudinal Ligament: Etiology, Diagnosis, and Outcomes of Nonoperative and Operative Management. Global Spine J. 2016; 6(2):195-204. [8] YANG H, SUN J, SHI J, et al. Anterior Controllable Antedisplacement Fusion (ACAF) for Severe Cervical Ossification of the Posterior Longitudinal Ligament: Comparison with Anterior Cervical Corpectomy with Fusion (ACCF). World Neurosurg. 2018;115:e428-e436 [9] YANG H, SUN J, SHI J, et al. Anterior controllable antedisplacement fusion as a choice for 28 patients of cervical ossification of the posterior longitudinal ligament with dura ossification: the risk of cerebrospinal fluid leakage compared with anterior cervical corpectomy and fusion. Eur Spine J. 2019;28(2):370-379. [10] WANG H, YANG R, LIU H, et al. Comparison of Interventions for Cervical Ossification of Posterior Longitudinal Ligament: A Systematic Review and Network Meta-Analysis. World Neurosurg. 2021;155:1-12. [11] LI S, PENG J, XU R, et al. Comparison of the surgeries for the ossification of the posterior longitudinal ligament-related cervical spondylosis: A PRISMA-compliant network meta-analysis and literature review. Medicine (Baltimore). 2021;100(9):e24900. [12] CHEN Y, SUN J, YUAN X, et al. Comparison of Anterior Controllable Antedisplacement and Fusion With Posterior Laminoplasty in the Treatment of Multilevel Cervical Ossification of the Posterior Longitudinal Ligament: A Prospective, Randomized, and Control Study With at Least 1-Year Follow Up. Spine (Phila Pa 1976). 2020;45(16):1091-1101. [13] ZHANG Y, HUANG Z, XU P, et al. Comparison of Anterior Controllable Antedisplacement and Fusion versus Laminoplasty in the Treatment of Multisegment Ossification of Cervical Posterior Longitudinal Ligament: A Meta-Analysis of Clinical. World Neurosurg. 2023:S1878-8750(23)01859-4. [14] LIU G, BUCHOWSKI JM, BUNMAPRASERT T, et al. Revision surgery following cervical laminoplasty: etiology and treatment strategies. Spine (Phila Pa 1976). 2009;34(25):2760-2768. [15] YANG H, GUO Y, SHI J, et al. Surgical results and complications of anterior controllable antedisplacement fusion as a revision surgery after initial posterior surgery for cervical myelopathy due to ossification of the posterior longitudinal ligament. J Clin Neurosci. 2018;56:21-27. [16] WANG H, SUN J, TAN Y, et al. Anterior Controllable Antedisplacement and Fusion as Revision Surgery After Posterior Decompression Surgery in Patients with Ossification of the Posterior Longitudinal Ligament. World Neurosurg. 2019;123:e310-e317. [17] MIAO J, SUN J, SHI J, et al. A Novel Anterior Revision Surgery for the Treatment of Cervical Ossification of Posterior Longitudinal Ligament: Case Report and Review of the Literature. World Neurosurg. 2018;113:212-216. [18] LI HD, ZHANG QH, XING ST, et al. A novel revision surgery for treatment of cervical ossification of the posterior longitudinal ligament after initial posterior surgery: preliminary clinical investigation of anterior controllable antidisplacement and fusion. J Orthop Surg Res. 2018; 13(1):215. [19] SUN J, SHI J, XU X, et al. Anterior controllable antidisplacement and fusion surgery for the treatment of multilevel severe ossification of the posterior longitudinal ligament with myelopathy: preliminary clinical results of a novel technique. Eur Spine J. 2018;27(6):1469-1478. [20] CHEN Y, SUN J, HAN D, et al. An open-label randomized multi-Centre study to evaluate anterior controllable Antedisplacement and fusion versus posterior Laminoplasty in patients with cervical ossification of the posterior longitudinal ligament: study design and analysis plan (STAR). BMC Musculoskelet Disord. 2021;22(1):765. [21] SUN K, WANG S, SUN J, et al. Surgical Outcomes After Anterior Controllable Antedisplacement and Fusion Compared with Single Open-Door Laminoplasty: Preliminary Analysis of Postoperative Changes of Spinal Cord Displacements on T2-Weighted Magnetic Resonance Imaging. World Neurosurg. 2019;127:e288-e298. [22] SUN K, WANG S, HUAN L, et al. Analysis of the spinal cord angle for severe cervical ossification of the posterior longitudinal ligament: comparison between anterior controllable antedisplacement and fusion (ACAF) and posterior laminectomy. Eur Spine J. 2020;29(5):1001-1012. [23] SUN K, WANG S, SUN J, et al. Analysis of the Correlation Between Cerebrospinal Fluid Space and Outcomes of Anterior Controllable Antedisplacement and Fusion for Cervical Myelopathy Due to Ossification of the Posterior Longitudinal Ligament. World Neurosurg. 2019;22:e358-e366. [24] YANG H, SUN J, SHI J, et al. In Situ Decompression to Spinal Cord During Anterior Controllable Antedisplacement Fusion Treating Degenerative Kyphosis with Stenosis: Surgical Outcomes and Analysis of C5 Nerve Palsy Based on 49 Patients. World Neurosurg. 2018;115:e501-e508. [25] KONG QJ, LUO X, TAN Y, et al. Anterior Controllable Antedisplacement and Fusion (ACAF) vs Posterior Laminoplasty for Multilevel Severe Cervical Ossification of the Posterior Longitudinal Ligament: Retrospective Study Based on a Two-Year Follow-up. Orthop Surg. 2021;13(2):474-483. [26] LUO X, WANG S, SUN K, et al. Anterior Controllable Antedisplacement and Fusion (ACAF) Technique for the Treatment of Multilevel Cervical Spondylotic Myelopathy With Spinal Stenosis (MCSMSS): A Retrospective Study of 54 Cases. Clin Spine Surg. 2021;34(9):322-330. [27] ZHANG B, SUN J, XU X, et al. Skip corpectomy and fusion (SCF) versus anterior controllable antedisplacement and fusion (ACAF): which is better for patients with multilevel cervical OPLL? Arch Orthop Trauma Surg. 2019;139(11):1533-1541. [28] 李广州,欧阳建元,王清,等.枢椎环骨折损伤机制的三维有限元分析[J].中国脊柱脊髓杂志,2022,32(2):160-168. [29] WU TK, MENG Y, WANG BY, et al. Biomechanics following skip-level cervical disc arthroplasty versus skip-level cervical discectomy and fusion: a finite element-based study. BMC Musculoskelet Disord. 2019;20(1):49. [30] SIM O, RYU D, LEE J, et al.Stress Distribution on Spinal Cord According to Type of Laminectomy for Large Focal Cervical Ossification of Posterior Longitudinal Ligament Based on Finite Element Method. Bioengineering (Basel). 2022;9(10):519. [31] PANJABI MM, CRISCO JJ, VASAVADA A, et al. Mechanical properties of the human cervical spine as shown by three-dimensional load-displacement curves. Spine (Phila Pa 1976). 2001;26(24):2692-2700. [32] LIU Q, GUO Q, YANG J, et al. Subaxial Cervical Intradiscal Pressure and Segmental Kinematics Following Atlantoaxial Fixation in Different Angles. World Neurosurg. 2016;87:521-528. [33] 牛陆,李娜,柳茵,等.后纵韧带硬化对颈椎力学影响的三维有限元分析[J].北京生物医学工程,2018,37(1):40-50. [34] 杨健,王贵江,崔晓雅.颈椎后纵韧带骨化椎间盘及后纵韧带应力的有限元分析[J].中国矫形外科杂志,2021,29(1):64-68. [35] KIM KS. Clinical Effectiveness of Posterior Cervical Decompression and Fusion in Terms of Reducing OPLL Growth Versus Cervical Motion Preservation. Neurospine. 2019;16(3):492-493. [36] WANG J, QIAN Z, REN L, et al. Biomechanical comparison of optimal shapes for the cervical intervertebral fusion cage for C5-C6 cervical fusion using the anterior cervical plate and cage (ACPC) fixation system: a finite element analysis. Med Sci Monit. 2019;25:8379-8388. [37] CHEUNG ZB, GIDUMAL S, WHITE S, et al. Comparison of anterior cervical discectomy and fusion with a stand-alone interbody cage versus a conventional cage-plate technique: asystematic review and meta-analysis. Global Spine J. 2019;9(4):446-455. [38] 孔庆捷. ACAF技术的生物力学与临床应用解剖学研究[D].上海:中国人民解放军海军军医大学,2021. [39] WANG Z, ZHAO H, LIU JM, et al. Biomechanics of anterior plating failure in treating distractive flexion injury in the caudal subaxial cervical spine. Clin Biomech (Bristol, Avon). 2017;50:130-138. [40] LI F, LI Z, HUANG X, et al. Comparison of two reconstructive techniques in the surgical management of four-level cervical spondylotic myelopathy. Biomed Res Int. 2015;2015:513906. [41] CHANG SW, KAKARLA UK, MAUGHAN PH, et al. Four-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Neurosurg. 2010;66(4):639-646,646-647. [42] 彭建城,姚晓玲,凌海乾,等.颈前路减压融合后椎间植入物下沉的风险与预防[J].中国组织工程研究,2023,27(27):4408-4413. [43] LIU J, WANG R, WANG H, et al. Biomechanical Comparison of a New Memory Compression Alloy Plate versus Traditional Titanium Plate for Anterior Cervical Discectomy and Fusion: A Finite Element Analysis. Biomed Res Int. 2020;2020:5769293. [44] LEE DH, RIEW KD, CHOI SH, et al. Safety and Efficacy of a Novel Anterior Decompression Technique for Ossification of Posterior Longitudinal Ligament of the Cervical Spine. J Am Acad Orthop Surg. 2020;28(8): 332-341. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [3] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [4] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [5] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [6] | Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904. |
| [7] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [8] | Li Shuai, Liu Hua, Shang Yonghui, Liu Yicong, Zhao Qihang, Liu Wen. Stress distribution on the maxilla when wearing the Twin-block appliance for Class II malocclusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 881-887. |
| [9] | Zhou Zonghao, Luo Siyang, Chen Jiawen, Chen Guangneng, Feng Hongchao. Finite element analysis of bioabsorbable plates versus miniature titanium plates in mandibular fracture fixation in different bone qualities [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 818-826. |
| [10] | Chen Yilong, Zhang Xu, Li Hong. Mechanical analysis of fiber post combined with different crown restorations for endodontically treated non-carious cervical lesions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 866-871. |
| [11] | Yang Yicheng, Zheng Zhizhen, Liang Shuangxue, Wu Chengliang, Du Yunyun. Influence and implications of basketball shoes' functional parameters on human biomechanics [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7620-7628. |
| [12] | Song Xubin, Wu Dou, Zhao Enzhe, Zhang Xingyu, Zhang Xiaolun, Wang Chuheng. Finite element analysis of a new femoral neck spiral blade system to treat femoral intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7041-7047. |
| [13] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| [14] | Xu Xin, Wurikaixi·Aiyiti, Lyu Gang, Maimaiaili·Yushan, Ma Zhiqiang, Ma Chao. Finite element analysis of four different internal fixation methods for complex acetabular double-column fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7063-7071. |
| [15] | Liang Cheng, Zhuo Chuanchuan, Zhang Xiaogang, Wang Guan, Duan Ke, Li Zhong, Lu Xiaobo, Zhuo Naiqiang, Jin Zhongmin. Biomechanical characteristics of a novel sacroiliac lag screw [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7080-7086. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||