[1] HOANG DM, PHAM PT, BACH TQ, et al. Stem cell-based therapy for human diseases. Signal Transduct Target Ther. 2022;7(1):272.
[2] QU SW, XUE YN, LI P, et al. Advances in the research of stem cell tissue-engineering. Zhonghua Shao Shang Za Zhi. 2020;36(6):510-515.
[3] SALEMI S, PRANGE JA, BAUMGARTNER V, et al. Adult stem cell sources for skeletal and smooth muscle tissue engineering. Stem Cell Res Ther. 2022;13(1):156.
[4] AN G, GUO F, LIU X, et al. Functional reconstruction of injured corpus cavernosa using 3D-printed hydrogel scaffolds seeded with HIF-1α-expressing stem cells. Nat Commun. 2020;11(1):2687.
[5] CHEN J, WANG L, LIU M, et al. Implantation of adipose-derived mesenchymal stem cell sheets promotes axonal regeneration and restores bladder function after spinal cord injury. Stem Cell Res Ther. 2022;13(1):503.
[6] FU Y, ZHANG YL, LIU RQ, et al. Exosome lncRNA IFNG-AS1 derived from mesenchymal stem cells of human adipose ameliorates neurogenesis and ASD-like behavior in BTBR mice. J Nanobiotechnology. 2024; 22(1):66.
[7] GU J, YOU J, LIANG H, et al. Engineered bone marrow mesenchymal stem cell-derived exosomes loaded with miR302 through the cardiomyocyte specific peptide can reduce myocardial ischemia and reperfusion (I/R) injury. J Transl Med. 2024;22(1):168.
[8] ABBÀ C, CROCE S, VALSECCHI C, et al. Circulating Mesenchymal Stromal Cells in Patients with Infantile Hemangioma: Evaluation of Their Functional Capacity and Gene Expression Profile. Cells. 2024;13(3):254.
[9] ZHANG Y, MCNEILL E, TIAN H, et al. Urine derived cells are a potential source for urological tissue reconstruction. J Urol. 2008;180(5):2226-2233.
[10] BHARADWAJ S, LIU G, SHI Y, et al. Multipotential differentiation of human urine-derived stem cells: potential for therapeutic applications in urology. Stem Cells. 2013;31(9):1840-1856.
[11] CHEN CY, RAO SS, REN L, et al. Exosomal DMBT1 from human urine-derived stem cells facilitates diabetic wound repair by promoting angiogenesis. Theranostics. 2018;8(6):1607-1623.
[12] SUN G, DING B, WAN M, et al. Formation and optimization of three-dimensional organoids generated from urine-derived stem cells for renal function in vitro. Stem Cell Res Ther. 2020;11(1):309.
[13] WU C, CHEN L, HUANG YZ, et al. Comparison of the Proliferation and Differentiation Potential of Human Urine-, Placenta Decidua Basalis-, and Bone Marrow-Derived Stem Cells. Stem Cells Int. 2018; 2018:7131532.
[14] LING X, ZHANG G, XIA Y, et al. Exosomes from human urine-derived stem cells enhanced neurogenesis via miR-26a/HDAC6 axis after ischaemic stroke. J Cell Mol Med. 2020;24(1):640-654.
[15] XU Y, ZHANG T, CHEN Y, et al. Isolation and Characterization of Multipotent Canine Urine-Derived Stem Cells. Stem Cells Int. 2020; 2020:8894449.
[16] LIU Y, MA W, LIU B, et al. Urethral reconstruction with autologous urine-derived stem cells seeded in three-dimensional porous small intestinal submucosa in a rabbit model. Stem Cell Res Ther. 2017;8(1):63.
[17] SONG YT, LI YQ, TIAN MX, et al. Application of antibody-conjugated small intestine submucosa to capture urine-derived stem cells for bladder repair in a rabbit model. Bioact Mater. 2021;14:443-455.
[18] ZHAO Z, LIU D, CHEN Y, et al. Ureter tissue engineering with vessel extracellular matrix and differentiated urine-derived stem cells. Acta Biomater. 2019;88:266-279.
[19] CHAN YY, BURY MI, YURA EM, et al. The current state of tissue engineering in the management of hypospadias. Nat Rev Urol. 2020; 17(3):162-175.
[20] JIN Y, ZHAO W, YANG M, et al. Cell-Based Therapy for Urethral Regeneration: A Narrative Review and Future Perspectives. Biomedicines. 2023;11(9):2366.
[21] ABBAS TO, PARANGUSAN H, YALCIN HC, et al. Trilayer composite scaffold for urethral reconstruction:in vitroevaluation of mechanical, biological, and angiogenic properties. Biomed Mater. 2024;19(2). doi: 10.1088/1748-605X/ad1c9c.
[22] CHENG Q, ZHANG L, ZHANG J, et al. Decellularized Scaffolds with Double-Layer Aligned Microchannels Induce the Oriented Growth of Bladder Smooth Muscle Cells: Toward Urethral and Ureteral Reconstruction. Adv Healthc Mater. 2023;12(26):e2300544.
[23] FRY CH, MENG E, YOUNG JS. The physiological function of lower urinary tract smooth muscle. Auton Neurosci. 2010;154(1-2):3-13.
[24] BHARADWAJ S, LIU G, SHI Y, et al. Characterization of urine-derived stem cells obtained from upper urinary tract for use in cell-based urological tissue engineering. Tissue Eng Part A. 2011;17(15-16): 2123-2132.
[25] LANG R, LIU G, SHI Y, et al. Self-renewal and differentiation capacity of urine-derived stem cells after urine preservation for 24 hours. PLoS One. 2013;8(1):e53980.
[26] BENTO G, SHAFIGULLINA AK, RIZVANOV AA, et al. Urine-Derived Stem Cells: Applications in Regenerative and Predictive Medicine. Cells. 2020;9(3):573.
[27] DONG X, ZHANG T, LIU Q, et al. Beneficial effects of urine-derived stem cells on fibrosis and apoptosis of myocardial, glomerular and bladder cells. Mol Cell Endocrinol. 2016;427:21-32.
[28] KIBSCHULL M, NGUYEN TTN, CHOW T, et al. Differentiation of patient-specific void urine-derived human induced pluripotent stem cells to fibroblasts and skeletal muscle myocytes. Sci Rep. 2023;13(1):4746.
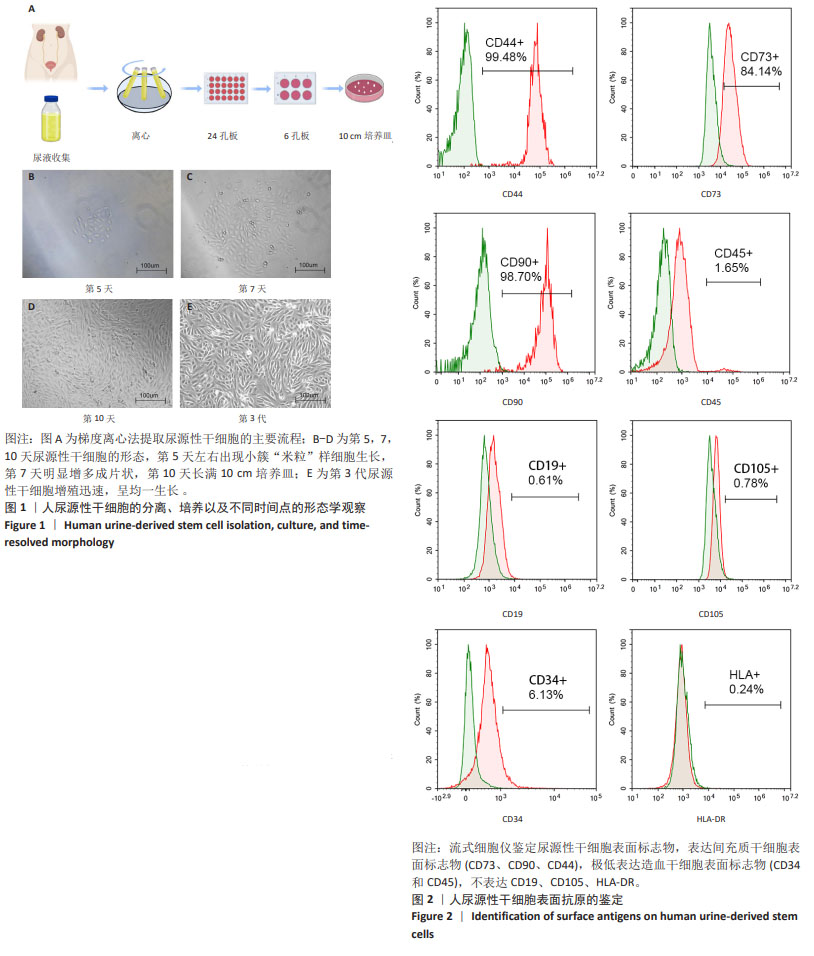
[29] 余胡燕,刘颖,顾秋华,等.健康成人尿源性干细胞的分离、培养与鉴定[J].天津医科大学学报,2021,27(1):1-5+21.
[30] TONG X, XU Y, ZHANG T, et al. Exosomes from CD133+ human urine-derived stem cells combined adhesive hydrogel facilitate rotator cuff healing by mediating bone marrow mesenchymal stem cells. J Orthop Translat. 2023;39:100-112.
[31] 哈木拉提·吐送,赵长辉,买买提艾力·买托合提,等.三种培养基对人尿源性干细胞生长和增殖的影响[J].中国组织工程研究, 2018,22(5):723-728.
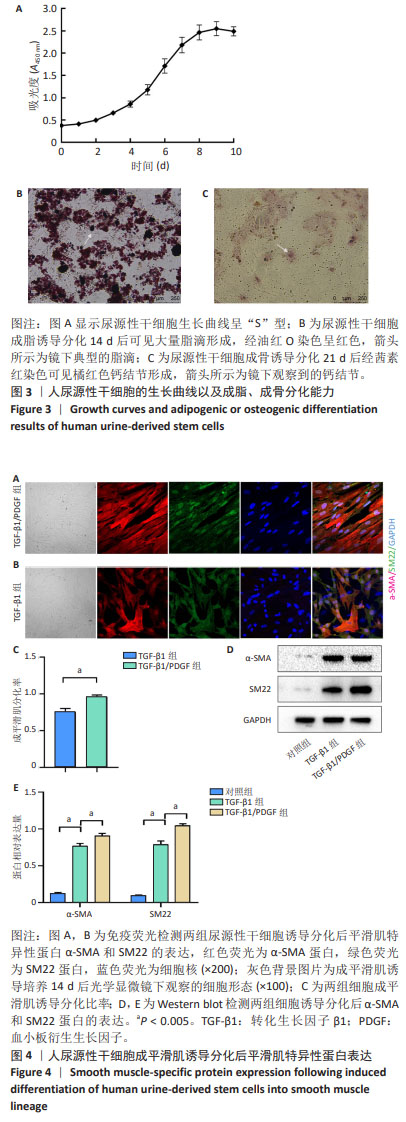
[32] 祝海洲,赵战魁,王鑫哲,等.尿源性干细胞在体外向尿路上皮细胞和平滑肌细胞的分化[J].中国组织工程研究,2020,24(19): 3010-3016.
[33] WU S, LIU Y, BHARADWAJ S, et al. Human urine-derived stem cells seeded in a modified 3D porous small intestinal submucosa scaffold for urethral tissue engineering. Biomaterials. 2011;32(5):1317-1326.
[34] YANG H, CHEN B, DENG J, et al. Characterization of rabbit urine-derived stem cells for potential application in lower urinary tract tissue regeneration. Cell Tissue Res. 2018;374(2):303-315.
[35] GRAFE I, ALEXANDER S, PETERSON JR, et al. TGF-β Family Signaling in Mesenchymal Differentiation. Cold Spring Harb Perspect Biol. 2018; 10(5):a022202.
[36] DONG K, GUO X, CHEN W, et al. Mesenchyme homeobox 1 mediates transforming growth factor-β (TGF-β)-induced smooth muscle cell differentiation from mouse mesenchymal progenitors. J Biol Chem. 2018;293(22):8712-8719.
[37] LIU Y, NIU XH, YIN X, et al. Elevated Circulating Fibrocytes Is a Marker of Left Atrial Fibrosis and Recurrence of Persistent Atrial Fibrillation. J Am Heart Assoc. 2018;7(6):e008083.
[38] KURPINSKI K, LAM H, CHU J, et al. Transforming growth factor-beta and notch signaling mediate stem cell differentiation into smooth muscle cells. Stem Cells. 2010;28(4):734-742.
[39] PENG C, SHAO X, TIAN X, et al. CREG ameliorates embryonic stem cell differentiation into smooth muscle cells by modulation of TGF-β expression. Differentiation. 2022;125:9-17.
[40] ANDRAE J, GALLINI R, BETSHOLTZ C. Role of platelet-derived growth factors in physiology and medicine. Genes Dev. 2008;22(10):1276-1312.
[41] HYE KIM J, GYU PARK S, KIM WK, et al. Functional regulation of adipose-derived stem cells by PDGF-D. Stem Cells. 2015;33(2):542-556.
[42] CIPRIANI P, DI BENEDETTO P, RUSCITTI P, et al. Impaired endothelium-mesenchymal stem cells cross-talk in systemic sclerosis: a link between vascular and fibrotic features. Arthritis Res Ther. 2014;16(5):442.
[43] CHEN Q, SONG H, LIU C, et al. The Interaction of EphA4 With PDGFRβ Regulates Proliferation and Neuronal Differentiation of Neural Progenitor Cells in vitro and Promotes Neurogenesis in vivo. Front Aging Neurosci. 2020;12:7.
[44] SIVARAMAN S, HEDRICK J, ISMAIL S, et al. Generation and Characterization of Human Mesenchymal Stem Cell-Derived Smooth Muscle Cells. Int J Mol Sci. 2021;22(19):10335. |