Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (8): 1626-1633.doi: 10.12307/2025.347
Previous Articles Next Articles
Prognosis of deep lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophy
Jing Ruyi, Chen Yingxin, Cao Lei
- General Hospital of Northern Theater Command, Shenyang 110000, Liaoning Province, China
-
Received:2024-03-04Accepted:2024-04-30Online:2025-03-18Published:2024-07-05 -
Contact:Chen Yingxin, Assoicate chief physician, General Hospital of Northern Theater Command, Shenyang 110000, Liaoning Province, China -
About author:Jing Ruyi, Master, Physician, General Hospital of Northern Theater Command, Shenyang 110000, Liaoning Province, China
CLC Number:
Cite this article
Jing Ruyi, Chen Yingxin, Cao Lei . Prognosis of deep lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophy[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1626-1633.
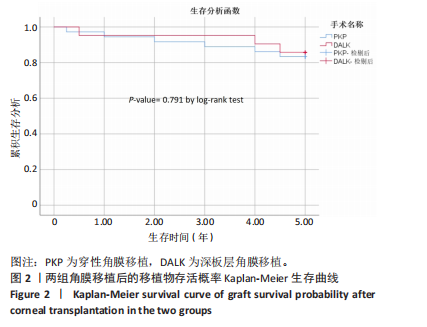
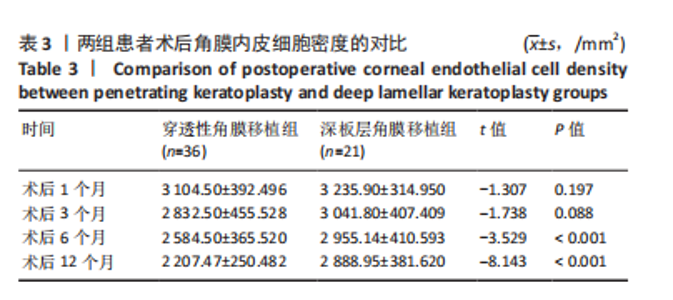
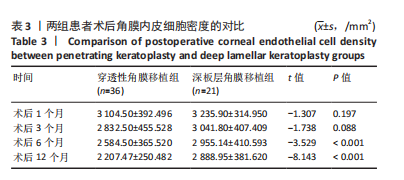
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
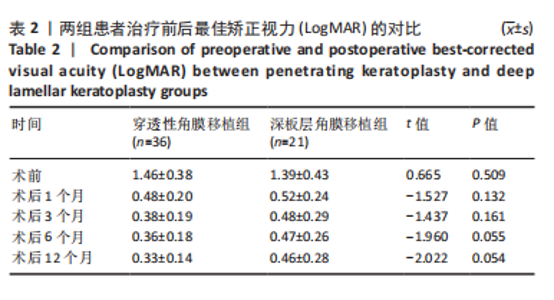
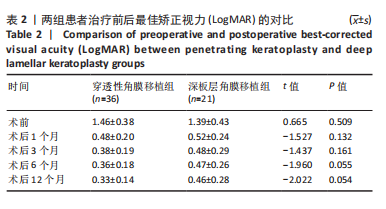
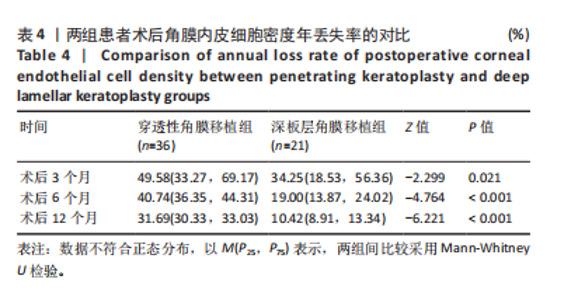
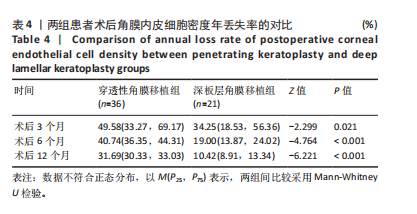
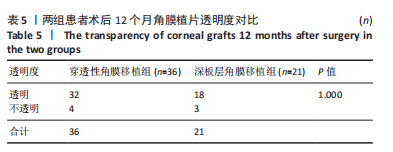
术后12个月,穿透性角膜移植组小数最佳矫正视力提高达0.3以上者22眼(61%,脱残率),深板层角膜移植组小数最佳矫正视力提高达0.3以上者12眼(57%,脱残率)。 2.5 两组患者术后角膜内皮细胞密度的比较 由于角膜混浊及角膜瘢痕,大部分患者在术前未获得角膜内皮细胞密度记录,此次研究中只对所有患者术后角膜内皮细胞密度进行了记载。应用非接触性角膜内皮镜在术后不同时间观察角膜内皮细胞密度,以术后1个月角膜内皮细胞密度为参考,对比术后3,6,12个月角膜内皮细胞的丢失率。复查期间平均内皮细胞年丢失率=[(术后1个月内皮细胞密度-复查时内皮细胞密度)×12/术后1个月内皮细胞密度]/复查间隔月份。 两组患者术后角膜内皮细胞密度及角膜内皮细胞年丢失率均随时间的延长逐渐降低。穿透性角膜移植组患者术后6,12个月的角膜内皮细胞密度均低于深板层角膜移植组(P < 0.001),两组患者术后1,3个月的角膜内皮细胞密度比较差异无显著性意义(P > 0.05),见表3。"
| [1] WEISS JS, MOLLER HU, ALDAVE AJ, et al. IC3D classification of corneal dystrophies--edition 2. Cornea. 2015;34(2):117-159. [2] CONSTANTIN C. Corneal dystrophies: pathophysiological, genetic, clinical, and therapeutic considerations. Rom J Ophthalmol. 2021; 65(2):104-108. [3] SALMAN M, VERMA A, SINGH VK, et al. New Frontier in the Management of Corneal Dystrophies: Basics, Development, and Challenges in Corneal Gene Therapy and Gene Editing. Asia Pac J Ophthalmol (Phila). 2022;11(4):346-359. [4] DOUGHTY MJ, JONUSCHEIT S. Corneal structure, transparency, thickness and optical density (densitometry), especially as relevant to contact lens wear-a review. Cont Lens Anterior Eye. 2019;42(3):238-245. [5] ASHENA Z, NIESTRATA M, TAVASSOLI S. Management of Stromal Corneal Dystrophies; Review of the Literature with a Focus on Phototherapeutic Keratectomy and Keratoplasty. Vision (Basel). 2023; 7(1):22. [6] KEMER AB, YILDIRIM Y, SONMEZ O, et al. Phototherapeutic Keratectomy in Macular and Granular Dystrophy: Two-year Results. Semin Ophthalmol. 2020;35(3):182-186. [7] SHIELDS M, CRAIG JE, SOUZEAU E, et al. Bilateral phototherapeutic keratectomy for corneal macular dystrophy in an adolescent: case report and review of the literature. Ophthalmic Genet. 2020;41(4): 368-372. [8] SAUVAGEOT P, JULIO G, BOLANOS JV, et al. Recurrence and Visual Outcomes of Phototherapeutic Keratectomy in Lattice Corneal Dystrophy: A Cohort Study. J Refract Surg. 2022;38(1):43-49. [9] NAGPAL R, MAHARANA PK, ROOP P, et al. Phototherapeutic keratectomy. Surv Ophthalmol. 2020;65(1):79-108. [10] YIN J. Advances in corneal graft rejection. Curr Opin Ophthalmol. 2021; 32(4):331-337. [11] Ahmed Reda. 深板层角膜移植与穿透性角膜移植治疗基质性角膜营养不良(英文)[J].国际眼科杂志,2020,20(7):1118-1125. [12] 北京同仁医院防盲办公室.《临床低视力学》一书出版[J]. 国际眼科纵览,2016,40(3):205. [13] 中华医学会眼科学分会角膜病学组.我国角膜移植术专家共识(2015年)[J].中华眼科杂志,2015,51(12):888-891. [14] 郭滨,程钧,孙亚杰,等.增视性角膜移植术后角膜植片透明率及影响因素[J].国际眼科杂志,2012,12(4):636-638. [15] SHIMAZAKI J, SHIMMURA S, ISHIOKA M, et al. Randomized clinical trial of deep lamellar keratoplasty vs penetrating keratoplasty. Am J Ophthalmol. 2002;134(2):159-165. [16] MOHAMED A, CHAURASIA S, RAMAPPA M, et al. Outcomes of keratoplasty in lattice corneal dystrophy in a large cohort of Indian eyes. Indian J Ophthalmol. 2018;66(5):666-672. [17] ALIÓ JL. Visual improvement after late debridement of residual stroma after anterior lamellar keratoplasty. Cornea. 2008;27:871-873. [18] 文丰,王骥,许玲俐,等.深板层角膜移植术后角膜植床厚度与角膜透明度相关性的观察[J].实用防盲技术,2019,14(1):3-5. [19] REDDY JC, MURTHY SI, VADDAVALLI PK, et al. Clinical outcomes and risk factors for graft failure after deep anterior lamellar keratoplasty and penetrating keratoplasty for macular corneal dystrophy. Cornea. 2015;34(2):171-176. [20] MANDAL S, MAHARANA PK, KAWERI L, et al. Management and prevention of corneal graft rejection. Indian J Ophthalmol. 2023;71(9): 3149-3159. [21] KU BI, HSIEH YT, HU FR, et al. Endothelial cell loss in penetrating keratoplasty, endothelial keratoplasty, and deep anterior lamellar keratoplasty. Taiwan J Ophthalmol. 2017;7(4):199-204. [22] LIU M, HONG J. Risk Factors for Endothelial Decompensation after Penetrating Keratoplasty and Its Novel Therapeutic Strategies. J Ophthalmol. 2018;2018:1389486. [23] SUN BJ, HONG J. [The changes and influencing factors of corneal endothelial cell density after endothelial keratoplasty]. Zhonghua Yan Ke Za Zhi. 2018;54(12):954-960. [24] PANDA A, BAGESHWAR LM, RAY M, et al. Deep lamellar keratoplasty versus penetrating keratoplasty for corneal lesions. Cornea. 1999; 18(2):172-175. [25] BAHAR I, KAISERMAN I, SRINIVASAN S, et al. Comparison of three different techniques of corneal transplantation for keratoconus. Am J Ophthalmol. 2008;146(6):905-912. [26] 魏玮,李志国,姚玉峰.深板层角膜移植治疗圆锥角膜术后角膜内皮细胞变化的观察[J].现代实用医学,2016,28(10):1326-1327. [27] YÜKSEL B, KUSBECI T, GUMUS F, et al. Long-Term Endothelial Cell Viability After Deep Anterior Lamellar Versus Penetrating Keratoplasty for Keratoconus. Exp Clin Transplant. 2023;21(7):599-606. [28] ALARAJ A, ALAMEER A, AL-SWAILEM S. Medium-Term Clinical Outcomes of Deep Anterior Lamellar Keratoplasty versus Penetrating Keratoplasty for Macular Corneal Dystrophy. Clin Ophthalmol. 2021;15:3139-3145. [29] REINHART WJ, MUSCH DC, JACOBS DS, et al. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the american academy of ophthalmolog. Ophthalmology. 2011; 118(1):209-218. [30] KODAVOOR SK, RATHI N, DANDAPANI R. Complications in deep anterior lamellar keratoplasty - A retrospective interventional analysis in a large series. Indian J Ophthalmol. 2022;70(10):3501-3507. [31] KODAVOOR SK, DEB B, RAMAMURTHY D. Deep anterior lamellar keratoplasty outcomes in macular and granular corneal dystrophy - A comparative cross-sectional study. Indian J Ophthalmol. 2019; 67(11):1830-1833. [32] STEVENSON LJ, ABELL RG, MCGUINNESS MB, et al. Comparative Evaluation Of Clinical Characteristics And Visual Outcomes Of Traumatic And Non-Traumatic Graft Dehiscence Following Corneal Transplantation Surgery. Clin Ophthalmol. 2019;13:2243-2249. [33] CHENG J, QI X, ZHAO J, et al. Comparison of penetrating keratoplasty and deep lamellar keratoplasty for macular corneal dystrophy and risk factors of recurrence. Ophthalmology. 2013;120(1):34-39. [34] UNAL M, ARSLAN OS, ATALAY E, et al. Deep anterior lamellar keratoplasty for the treatment of stromal corneal dystrophies. Cornea. 2013;32(3):301-305. [35] AL-SWAILEM SA, AL-RAJHI AA, WAGONER MD. Penetrating keratoplasty for macular corneal dystrophy. Ophthalmology. 2005;112(2):220-224. [36] SHREE N, GANDHI M, DAVE A, et al. Incidence and risk factors for post-penetrating keratoplasty glaucoma. Indian J Ophthalmol. 2022; 70(4):1239-1245. [37] SHARMA A, SHARMA S, PANDAV SS, et al. Post penetrating keratoplasty glaucoma: cumulative effect of quantifiable risk factors. Indian J Ophthalmol. 2014;62(5):590-595. [38] AKOVA YA, KIRKNESS CM, MCCARTNEY AC, et al. Recurrent macular corneal dystrophy following penetrating keratoplasty. Eye (Lond). 1990; 4(Pt 5):698-705. [39] MATHUR V, PARIHAR JK, SRIVASTAVA VK, et al. Clinical evaluation of Deep Anterior Lamellar Keratoplasty (DALK) for stromal corneal opacities. Med J Armed Forces India. 2013;69(1):21-26. [40] ROBIN AL, GREEN WR, LAPSA TP, et al. Recurrence of macular corneal dystrophy after lamellar keratoplasty. Am J Ophthalmol. 1977;84(4): 457-461. [41] MEYER HJ. [Prognosis of keratoplasty in hereditary stromal dystrophies]. Klin Monbl Augenheilkd. 1996;208(6):446-449. [42] BISCHOFF-JUNG M, FLOCKERZI E, HASENFUS A, et al. Recurrence of macular corneal dystrophy on the graft 50 years after penetrating keratoplasty. GMS Ophthalmol Cases. 2020;10:Doc34. [43] BOHRINGER D, REINHARD T, SPELSBERG H, et al. Influencing factors on chronic endothelial cell loss characterised in a homogeneous group of patients. Br J Ophthalmol. 2002;86(1):35-38. |
| [1] | Zheng Xuying, Hu Hongcheng, Xu Libing, Han Jianmin, Di Ping. Stress magnitude and distribution in two-piece cement-retained zirconia implants under different loading conditions and with varying internal connection shapes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1979-1987. |
| [2] | Xu Hao, Ding Lu, Li Xiao. Mechanical effect of mechanical wear of abutment screws on the Morse taper connection implant system: a three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1375-1383. |
| [3] | Liao Long, Zhao Zepeng, Li Zongyuan, Yu Qinglong, Zhang Tao, Tang Jinyuan, Ye Nan, Xu Han, Shi Bo. Establishment and validation of a model for femoral head necrosis after internal fixation of femoral neck fracture using logistic regression and SHAP analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 626-633. |
| [4] | Xue Hui, Li Dongnan, Zhao Yadi, Chen Chao, Xie Zongyuan. Relationship between BCR/ABL gene expression and recurrence before and after allogeneic transplantation in Ph chromosome positive acute lymphoblastic leukemia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 139-144. |
| [5] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [6] | Wang Rongqiang, Yang Liu, Wu Xiangkun, Shang Lilin. Analysis of factors associated with prognosis of osteoporosis patients after hip arthroplasty and construction of Nomogram prediction model [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7137-7142. |
| [7] | Jiang Zehua, Du Wenjun, Ren Zhishuai, Cui Haojun, Zhu Rusen. Percutaneous vertebroplasty via Kambin's triangle for treatment of osteoporotic compression fractures: evaluation of safety and effectiveness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7181-7188. |
| [8] | Liang Jiachang, Guan Hua, Feng Enhui, Chen Pu, Huang Weiming, He Jianbo, Xie Jiewei. Ilizarov technique for treatment of congenital brachymetatarsia of the fourth: subgroup analysis of prolongation ratio [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7217-7222. |
| [9] | Zhao Yihan, Sun Xuhang, Zhao Lin, Jiang Shiqing. Effects and mechanisms of exosomal miRNA in treatment of multiple myeloma [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6743-6752. |
| [10] | Shi Lei, Shi Song, Lu Yue, Tao Ran, Ma Hongdong. Comparison of unicondylar knee arthroplasty and high tibial osteotomy in treatment of medial knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 503-509. |
| [11] | Niu Yanyan, Zhang Qi, Fan Mingxing. Research and development trends and hot spots of spinal surgical robots for treatment of spinal diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4612-4620. |
| [12] | Luo Yuncai, Meng Maohua, , Li Ying, , Wang Huan, Lu Jing, Shu Jiayu, Li Wenjie, Sun Jinyi, Dong Qiang, . Copper influences the occurrence and development of diabetic complications [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3641-3649. |
| [13] | Chen Guangneng, Luo Siyang, Wang Mei, Ye Bin, Chen Jiawen, Liu Yin, Zuo Yuwen, He Xianyu, Shen Jiajin, Ma Minxian. Finite element analysis of various root shield thicknesses in maxillary central incisor socket-shield technique [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(10): 2052-2060. |
| [14] | Du Changling, Shi Hui, Zhang Shoutao, Meng Tao, Liu Dong, Li Jian, Cao Heng, Xu Chuang. Efficacy and safety of different applications of tranexamic acid in high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1409-1413. |
| [15] | Wang Ruoyu, Zhang Zhifeng, Huang Jian. Application and prospect of robotic-assisted total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(30): 4889-4895. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||