Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (31): 5046-5051.doi: 10.12307/2023.569
Previous Articles Next Articles
Correlation between platelet count and lumbar bone mineral density in middle-aged and elderly people
Zhang Jinpeng1, Chen Chang2, Pan Qiuyu3, Mai Chenyao3, Li Yinlong3, Hao Yuxi1, Hu Jun4
- 1Weifang Medical University, Weifang 261053, Shandong Province, China; 2Qilu Hospital of Shandong University, Jinan 250012, Shandong Province, China; 3Tibet University, Lasa 850000, Tibet Autonomous Region, China; 4School of Management, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China
-
Received:2022-08-16Accepted:2022-09-24Online:2023-11-08Published:2023-01-31 -
Contact:Hu Jun, Doctoral supervisor, School of Management, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
About author:Zhang Jinpeng, Master, Weifang Medical University, Weifang 261053, Shandong Province, China
CLC Number:
Cite this article
Zhang Jinpeng, Chen Chang, Pan Qiuyu, Mai Chenyao, Li Yinlong, Hao Yuxi, Hu Jun. Correlation between platelet count and lumbar bone mineral density in middle-aged and elderly people[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(31): 5046-5051.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
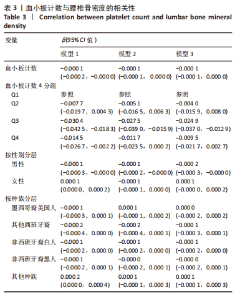
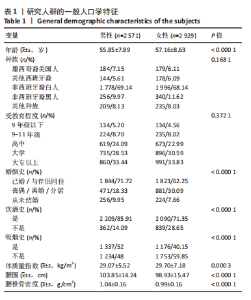
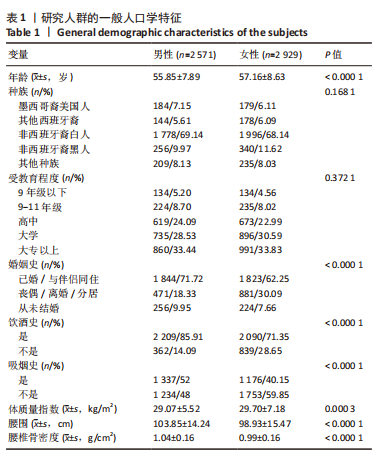
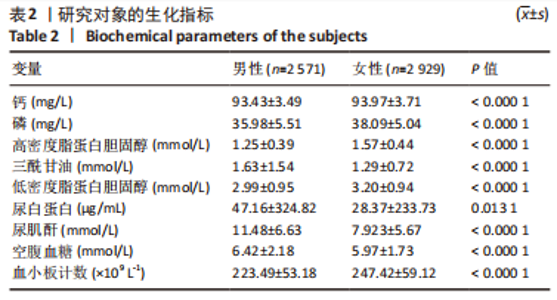
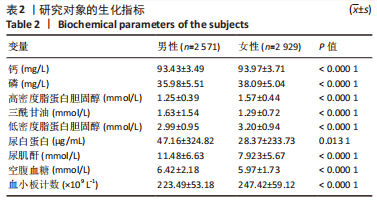
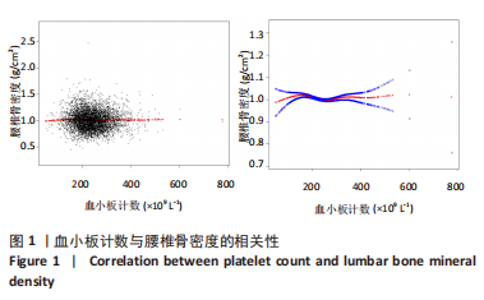
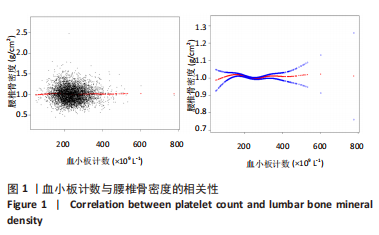
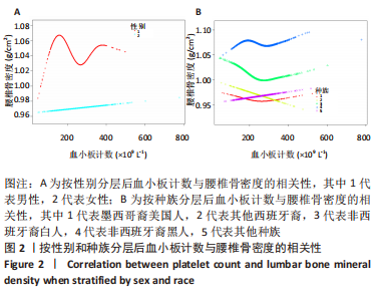
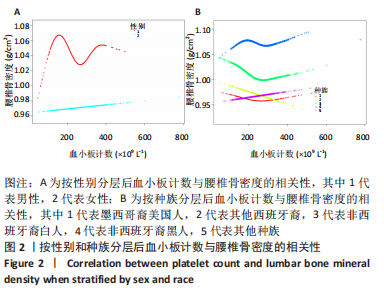
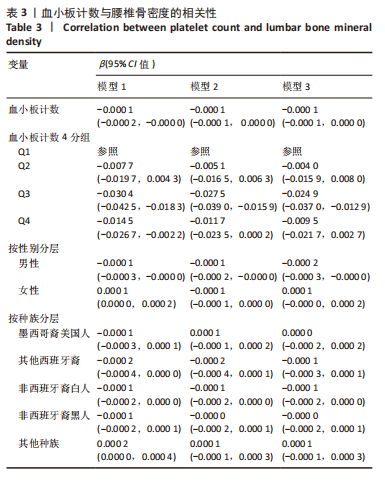
2.4 血小板计数与腰椎骨密度的相关性 用多个回归方程研究血小板计数和腰椎骨密度之间的关系,模型1不调整任何变量,模型2将年龄、性别、种族、受教育程度、婚姻史、体质量指数和腰围纳入协变量,模型3将年龄、性别、种族、受教育程度、婚姻史、体质量指数、腰围、钙、磷、高密度脂蛋白胆固醇、三酰甘油、低密度脂蛋白胆固醇、空腹血糖、尿白蛋白和尿肌酐纳入协变量。 在多个回归方程中,血小板计数与骨密度呈负相关,将尿白蛋白4分组后,每个分组的3个模型均呈现负相关关系;按性别分层后,男性的3个模型呈负相关关系[模型1:β=-0.000 1,95% CI(0.000 3,<-0.000 1);模型2:β=-0.000 1,95%CI(-0.000 2,< -0.000 1);模型3:β=-0.000 2,95% CI(-0.000 3,<-0.000 1)];按种族分层后,只有其他种族美国人的3个模型呈现正相关关系[模型1:β=0.000 2,95% CI(< 0.000 1,0.000 4);模型2:β=0.000 1,95% CI(-0.000 1,0.000 3);模型3:β=0.000 1,95% CI(-0.000 1,0.000 3)],而西班牙裔、非西班牙裔白人和非西班牙裔黑人3个模型呈现负相关关系,详见表3。"
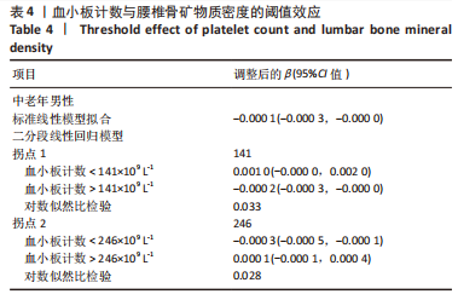
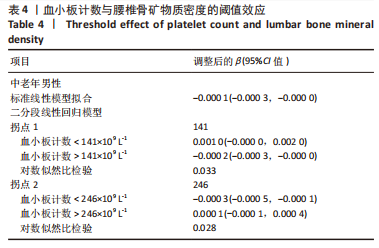
2.6 男性血小板计数与腰椎骨密度的阈值效应分析 由图2可以看出,男性正常范围内的血小板计数与腰椎骨密度的非线性关系存在2个明显的拐点[7],使用二分段线性回归模型分别找出这2个拐点,结果显示2个拐点分别是141×109 L-1和246×109 L-1。 当血小板计数< 141×109 L-1时,β(95% CI)为0.001 0(-0.000 0,0.002 0);当血小板计数> 141×109 L-1时,β(95% CI)为-0.000 2(-0.000 3,-0.000 0);当血小板计数< 246×109 L-1时,β(95% CI)为-0.000 3(-0.000 5,-0.000 1);当血小板计数> 246×109 L-1时,β(95% CI)为0.000 1(-0.000 1,0.000 4);即正常范围内血小板计数< 141×109 L-1时腰椎骨密度与血小板计数正相关,血小板计数在(141-246)×109 L-1时腰椎骨密度与血小板计数负相关,血小板计数> 246×109 L-1时腰椎骨密度与血小板计数正相关,详见表4。"
| [1] 夏维波,章振林,林华,等.原发性骨质疏松症诊疗指南(2017)[J].中国骨质疏松杂志,2019,25(3):281-309. [2] JOHNELL O, KANIS JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17:1726-1733. [3] EASTELL R, PAWEL SZULC P. Use of bone turnover markers in postmenopausal osteoporosis. Lancet Diabetes Endocrinol. 2017;5: 908-923. [4] MURACA M, CAPPARIELLO A. The role of extracellular vesicles (EVs) in the epigenetic regulation of bone metabolism and osteoporosis. Int J Mol Sci. 2020;21:8682. [5] CIUFFI S. Circulating microRNAs as novel biomarkers for osteoporosis and fragility fracture risk: is there a use in assessment risk? Int J Mol Sci. 2020;21:6927. [6] ZHU Z, ZHOU H, WANG Y, et al. Associations between bone turnover markers and bone mineral density in older adults. J Orthop Surg (Hong Kong). 2021;29(1):467-475. [7] SAMOCHA-BONET D, JUSTO D, ROGOWSKI O, et al. Platelet counts and platelet activation markers in obese subjects. Mediators Inflamm. 2008;2008:834153. [8] FAIN JA. NHANES. Diabetes Educ. 2017;43(2):151. [9] AHLUWALIA N, DWYER J, TERRY A, et al. Update on NHANES Dietary Data: Focus on Collection, Release, Analytical Considerations, and Uses to Inform Public Policy. Adv Nutr. 2016;7(1):121-134. [10] FULGONI K, FULGONI VL. Trends in Total, Added, and Natural Phosphorus Intake in Adult Americans, NHANES 1988-1994 to NHANES 2015-2016. Nutrients. 2021;13(7):2249. [11] DARIMONT T, KARAVASILOGLOU N, HYSAJ O, et al. Body weight and self-perception are associated with depression: Results from the National Health and Nutrition Examination Survey (NHANES) 2005-2016. J Affect Disord. 2020;274:929-934. [12] 丛玉隆,金大鸣,王鸿利,等.中国人群血小板各项参数的调查分析[J].中华检验医学杂志,2004,27(6):35-37. [13] LINDEN MD, JACKSON DE. Platelets: Pleiotropic roles in atherogenesis and atherothrombosis. Int J Biochem Cell Biol. 2010;42(11):1762-1766. [14] KHODADI E. Platelet Function in Cardiovascular Disease: Activation of Molecules and Activation by Molecules. Cardiovasc Toxicol. 2020; 20(1):1-10. [15] YIN H, SHI A, WU J. Platelet-Activating Factor Promotes the Development of Non-Alcoholic Fatty Liver Disease. Diabetes Metab Syndr Obes. 2022;15:2003-2030. [16] ELSON A, ANUJ A, BARNEA-ZOHAR M, et al. The origins and formation of bone-resorbing osteoclasts. Bone. 2022;164:116538. [17] YE J, XIAO J, WANG J, et al. The Interaction Between Intracellular Energy Metabolism and Signaling Pathways During Osteogenesis. Front Mol Biosci. 2022;8:807487. [18] CIOVACCO WA, CHENG YH, HOROWITZ MC, et al. Immature and mature megakaryocytes enhance osteoblast proliferation and inhibit osteoclast formation. J Cell Biochem. 2010;109(4):774-781. [19] TAYLOR KA, MAHAUT-SMITH MP. Ion channels and ion homeostasis in the platelet and megakaryocyte. Platelets. 2021;32(7):853-854. [20] RAWISH E, NORDING H, MÜNTE T, et al. Platelets as Mediators of Neuroinflammation and Thrombosis. Front Immunol. 2020;11: 548631. [21] MIYAMOTO K. Osteoclasts are dispensable for hematopoietic stem cell maintenance and mobilization. J Exp Med. 2011;208:2175-2181. [22] WAGNER DD, BURGER PC. Platelets in inflammation and thrombosis. Arterioscler Thromb Vasc Biol. 2003;23(12):2131-2137. [23] WEYRICH AS, ZIMMERMAN GA. Platelets: signaling cells in the immune continuum. Trends Immunol. 2004;25(9):489-495. [24] INTINI G. The use of platelet-rich plasma in bone reconstruction therapy. Biomaterials. 2009;30(28):4956-4966. [25] MAJIDINIA M, SADEGHPOUR A, YOUSEFI B. The roles of signaling pathways in bone repair and regeneration. J Cell Physiol. 2018;233(4): 2937-2948. [26] KHAN FA, PARAYARUTHOTTAM P, ROSHAN G, et al. Platelets and Their Pathways in Dentistry: Systematic Review. J Int Soc Prev Community Dent. 2017;7(Suppl 2):S55-S60. [27] CAMARGO PM, LEKOVIC V, WEINLAENDER M, et al. Platelet-rich plasma and bovine porous bone mineral combined with guided tissue regeneration in the treatment of intrabony defects in humans. J Periodontal Res. 2002;37:300-306. [28] LITVINOVA L, YUROVA K, SHUPLETSOVA V, et al. Gene Expression Regulation and Secretory Activity of Mesenchymal Stem Cells upon In Vitro Contact with Microarc Calcium Phosphate Coating. Int J Mol Sci. 2020;21(20):7682. [29] PARSONS P, BUTCHER A, HESSELDEN K, et al. Platelet-rich concentrate supports human mesenchymal stem cell proliferation, bone morphogenetic protein-2 messenger RNA expression, alkaline phosphatase activity, and bone formation in vitro: A mode of action to enhance bone repair. J Orthop Trauma. 2008;22:595-604. [30] SUMIDA R, MAEDA T, KAWAHARA I, et al. Platelet-rich fibrin increases the osteoprotegerin/receptor activator of nuclear factor-κB ligand ratio in osteoblasts. Exp Ther Med. 2019;18(1):358-365. [31] ZHANG N, WU YP, QIAN SJ, et al. Research progress in the mechanism of effect of PRP in bone deficiency healing. ScientificWorldJournal. 2013;2013:134582. [32] SCHMIDMAIER G, HERRMANN S, GREEN J, et al. Quantitative assessment of growth factors in reaming aspirate, iliac crest, and platelet preparation. Bone. 2006;39(5):1156-1163. [33] GRUBER R, KARRETH F, FISCHER MB, et al. Platelet-released supernatants stimulate formation of osteoclast-like cells through a prostaglandin/RANKL-dependent mechanism. Bone. 2002;30(5):726-732. [34] CARDOSO CL, CURRA C, CURI MM, et al. Treatment of bisphosphonate-related osteonecrosis using platelet-rich plasma: microtomographic, microscopic, and immunohistochemical analyses. Braz Oral Res. 2019; 33:e050. [35] YAO Z, GETTING SJ, LOCKE IC. Regulation of TNF-Induced Osteoclast Differentiation. Cells. 2021;11(1):132. [36] WANG D, WENG Y, GUO S, et al. Platelet-rich plasma inhibits RANKL-induced osteoclast differentiation through activation of Wnt pathway during bone remodeling. Int J Mol Med. 2018;41(2):729-738. [37] LI XS, ZHANG JR, MENG SY, et al. Mean platelet volume is negatively associated with bone mineral density in postmenopausal women. J Bone Miner Metab. 2012;30(6):660-665. [38] AKBAL A, GÖKMEN F, GENCER M, et al. Mean platelet volume and platelet distribution width can be related to bone mineralization. Osteoporos Int. 2014;25:2291-2295. [39] PIRSL F, CURTIS LM, STEINBERG SM, et al. Characterization and risk factor analysis of osteoporosis in a large cohort of patients with chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2016; 22(8):1517-1524. [40] KIM J, KIM HS, LEE HS, et al. The relationship between platelet count and bone mineral density: results from two independent population-based studies. Arch Osteoporos. 2020;15(1):43. [41] KRISTJANSDOTTIR HL, MELLSTRÖM D, JOHANSSON P, et al. High platelet count is associated with low bone mineral density: The MrOS Sweden cohort. Osteoporos Int. 2021;32(5):865-871. [42] WATANABE Y, TSUCHIYA A, TERAI S. The development of mesenchymal stem cell therapy in the present, and the perspective of cell-free therapy in the future. Clin Mol Hepatol. 2021;27(1):70-80. [43] DENG P, YUAN Q, CHENG Y, et al. Loss of KDM4B exacerbates bone-fat imbalance and mesenchymal stromal cell exhaustion in skeletal aging. Cell Stem Cell. 2021;28(6):1057-1073.e7. [44] KIM PG, NIROULA A, SHKOLNIK V, et al. Dnmt3a-mutated clonal hematopoiesis promotes osteoporosis. J Exp Med. 2021;218(12): e20211872. [45] ZHAO X, ZHANG C, CUI X, et al. Interactions of Hematopoietic Stem Cells with Bone Marrow Niche. Methods Mol Biol. 2021;2346:21-34. [46] YANG S, ZHANG F, MA J, et al. Intervertebral disc ageing and degeneration: The antiapoptotic effect of oestrogen. Ageing Res Rev. 2020;57:100978. [47] HIKIJI H, ISHII S, SHINDOU H, et al. Absence of platelet-activating factor receptor protects mice from osteoporosis following ovariectomy. J Clin Invest. 2004;114(1):85-93. |
| [1] | Li Shichao, Xie Guangyue, Sun Zhen, Han Peng, Hou Xiaohua, Sun Xiaowei, Zhang Qidong. Correlation of knee joint alignment correction between valgus stress and postoperative radiography after unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2910-2914. |
| [2] | Zhang Haolin, Wang Yalin, Liu Yafei, Zuo Yanping, Zhang Xiaohuan. Effect of maxillary protraction on temporomandibular joint changes in skeletal class III children: a correlation analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(11): 1641-1646. |
| [3] | Wu Liang, Wang Qiang, Wang Wenbo, Xin Tianwen, Xi Kun, Tang Jincheng, Xu Jingzhi, Chen Liang, Gu Yong. Risk factors for traumatic central cord syndrome underlying with cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1388-1394. |
| [4] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [5] | Zhou Yuanbo, Huang Wenliang, Wang Jindong. Imaging analysis of the correlation between tibial tuberosity-trochlea groove distance and femoral trochlea morphology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4390-4394. |
| [6] | Jiang Lihong, Wu Xiaofeng, Ouyang Lin, Luo Aifang, Huang Li. Computer aided diagnosis of lumbar disc degeneration based on metabolomics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3796-3803. |
| [7] | Wan Huazhe, Chai Guangxin, Xiao Xiaoling, Huang Wenying. Effects of phellinus igniarius crude polysaccharides on sporting ability and free radical metabolism of skeletal muscle in mice suffering passive smoking [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 689-693. |
| [8] | Cao Houran, Deng Peng, Ye Pengcheng, Jie Ke, Zeng Jianchun, Feng Wenjun, Chen Jinlun, Qi Xinyu, Li Jie, Tan Xueqiu, Zhang Haitao, Zeng Yirong. Platelet count as a novel potential predictor of periprosthetic joint infection [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(30): 4795-4801. |
| [9] | Lin Yuan, Xu Bin, Tu Jun, Xu Honggang, Guo Ruipeng. Effect of different femoral tunnel locations on patellofemoral joint during single-bundle anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(14): 2140-2146. |
| [10] | Jian Changchun, Chen Yu, Chen Cheng, Hu Ning, Huang Wei. Anticoagulant effect of low-molecular-weight heparin versus rivaroxaban after arthroplasty assessed by thromboelastography [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 499-504. |
| [11] | Wang Wuhua, Liu Xudong, Hu Ling. Prediction of hip fracture in Parkinson’s disease with the combination of geometric structure of proximal femur and bone mineral density [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(24): 3829-3833. |
| [12] |
Ma Junfeng, Wang Wei, Wang Zikuo, Jiang Zehua, Long Mingxing, Yuan Jianjun, Zhu Rusen, Hu Wei, Zhang Xueli.
Correlation between facet joint effusion in magnetic resonance imaging and lumbar stability after interspinous and degenerative lumbar spondylolisthesis
[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(24): 3845-3851.
|
| [13] | Shan Hong, Wang Jiao-jie, Bie Li-li, Liu Min, Qi Zheng, Duan Yan-li. Improved preparation of buffy-coat-derived platelet concentrates and factors affecting platelet recovery [J]. Chinese Journal of Tissue Engineering Research, 2014, 18(7): 1082-1087. |
| [14] | Zhang Rui-dong, Zhang Lan, Mao Hong-gang, Liu Guo-dong. Apoptosis-related factors in a model of steroid-induced necrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2013, 17(7): 1189-1195. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||