Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (11): 1671-1676.doi: 10.3969/j.issn.2095-4344.0161
Previous Articles Next Articles
Efficacy of elastic intramedullary nail versus locking plate fixation in the treatment of middle clavicle fracture
Peng Lin-bo, Chen Xiao-bin, Zhang Jian-zheng, Wang Xiao-wei, Sun Tian-sheng
- Department of Orthopedics, Army General Hospital, Second Medical College, Southern Medical University, Beijing 100010, China
-
Online:2018-04-18Published:2018-04-18 -
Contact:Sun Tian-sheng, Professor, Doctoral supervisor, Department of Orthopedics, Army General Hospital, Second Medical College, Southern Medical University, Beijing 100010, China -
About author:Peng Lin-bo, Master candidate, Department of Orthopedics, Army General Hospital, Second Medical College, Southern Medical University, Beijing 100010, China -
Supported by:the Applied Basic Research Project of the Health Bureau of the Military Commission's Logistics Support Department, No. 16CXZ002
CLC Number:
Cite this article
Peng Lin-bo, Chen Xiao-bin, Zhang Jian-zheng, Wang Xiao-wei, Sun Tian-sheng. Efficacy of elastic intramedullary nail versus locking plate fixation in the treatment of middle clavicle fracture [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(11): 1671-1676.
share this article
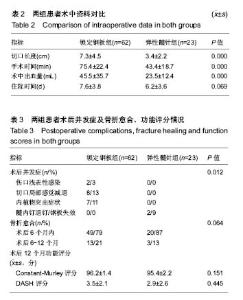
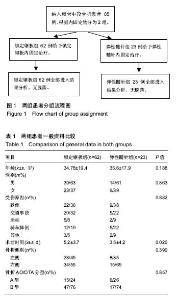
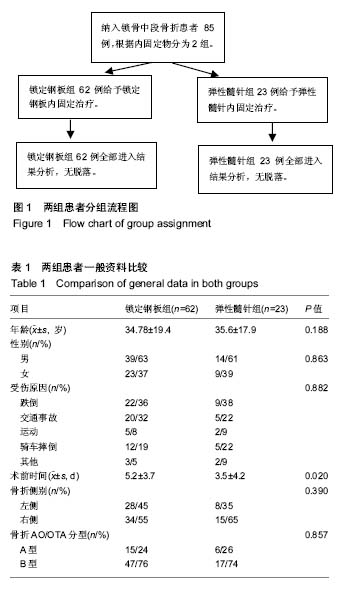
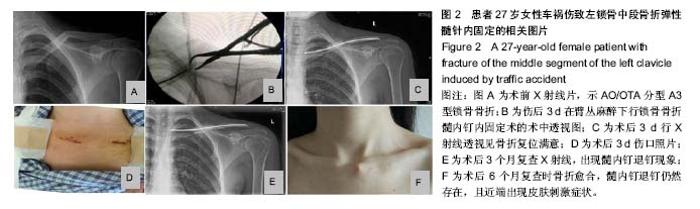
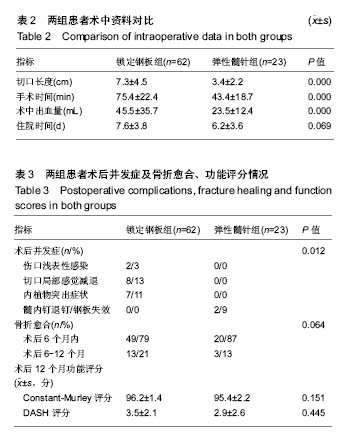
2.3 术中资料对比 弹性髓针组术前时间少于锁定钢板组(P < 0.05),见表1。弹性髓针组患者在切口长度、手术时间、出血量方面均优于锁定钢板组,差异有显著性意义(P < 0.05);弹性髓针组患者住院时间低于锁定钢板组,但差异无显著性意义(P > 0.05),见表2。 2.4 患者术后并发症及骨折愈合、功能评分对比 结果见表3。 弹性髓针组术后并发症远低于锁定钢板组,差异有显著性意义(P < 0.05)。锁定钢板组有2例(3%)患者出现术后切口浅表性感染,弹性髓针组无术后感染发生;锁定钢板组中8例(13%)患者主诉术后出现切口周围皮肤感觉减退,弹性髓针组患者未出现切口周围皮肤感觉减退症状;锁定钢板组有7例(11%)患者术后主诉内植物突出不适感,弹性髓针组未有患者主诉内植物突出感;弹性髓针组有2例(9%)患者出现髓针退钉及相应的皮肤刺激症状,锁定钢板组无内固定移位及失效等相关并发症。 术后6个月复查时锁定钢板组有49例(79%)患者影像学上骨折愈合,而弹性髓针组有20例(87%)的患者影像学上骨折愈合;术后6-12个月间锁定钢板组有9例(15%)患者影像学上骨折愈合,而同期弹性髓针组有3例(13%)的患者骨折愈合。弹性髓针组术后骨折愈合率高于锁定钢板组,但差异无显著性意义(P > 0.05)。 术后12个月随访时DASH评分及Constant-Murley评分,2组患者差异无显著性意义(P > 0.05)。"
| [1] Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002; 11:452-456.[2] Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994:127-132.[3] Govindasamy R, Kasirajan S, Meleppuram JJ, et al. A retrospective study of titanium elastic stable intramedullary nailing in displaced mid-shaft clavicle fractures. Rev Bras Ortop. 2016 ;52(3):270-277. [4] Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44.[5] van der Meijden OA, Houwert RM, Hulsmans M, et al. Operative treatment of dislocated midshaft clavicular fractures: plate or intramedullary nail fixation? A randomized controlled trial. J Bone Joint Surg. 2015; 97:613-619.[6] Angst F, Schwyzer HK, Aeschlimann A, et al. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res. 2011; 63 Suppl 11:S174-188.[7] Ebrahimzadeh MH, Moradi A, Vahedi E, et al. Validity and Reliability of the Persian Version of Shortened Disabilities of the Arm, Shoulder and Hand Questionnaire (Quick-DASH). Int J Prev Med. 2015;6:59. [8] Constant CR, Gerber C, Emery RJ, et al. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008; 17:355-361.[9] Yao M, Yang L, Cao ZY, et al. Chinese version of the Constant-Murley questionnaire for shoulder pain and disability: a reliability and validation study. Health Qual Life Outcomes. 2017; 15:178.[10] Chachan S, Tudu B, Sahu B. Ultrasound monitoring of fracture healing: is this the end of radiography in fracture follow-ups? J Orthop Trauma. 2015; 29:e133-138.[11] Litrenta J, Tornetta P 3rd, Mehta S, et al. Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma. 2015; 29:516-520.[12] Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg. 1997;79:537-539.[13] Khan LA, Bradnock TJ, Scott C, et al. Fractures of the clavicle. J Bone Joint Surg. 2009;91:447-460.[14] Roy JS, MacDermid JC, Woodhouse LJ. A systematic review of the psychometric properties of the Constant-Murley score. J Shoulder Elbow Surg. 2010; 19:157-164.[15] Ledger M, Leeks N, Ackland T, et al. Short malunions of the clavicle: an anatomic and functional study. J Shoulder Elbow Surg. 2005; 14:349-354.[16] Golish SR, Oliviero JA, Francke EI, et al. A biomechanical study of plate versus intramedullary devices for midshaft clavicle fixation. J Orthop Surg Res. 2008; 3:28.[17] Onstenk R, Malessy MJ, Nelissen RG. Brachial plexus injury due to unhealed or wrongly healed clavicular fracture. Ned Tijdschr Geneeskd. 2001;145(50):2440-2443.[18] Bernstein J. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. J Bone Joint Surg. 2007; 89:1866; author reply 1866-1867.[19] Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma.1997; 43:778-783.[20] Chen YF, Wei HF, Zhang C, et al. Retrospective comparison of titanium elastic nail (TEN) and reconstruction plate repair of displaced midshaft clavicular fractures. J Shoulder Elbow Surg. 2012; 21:495-501.[21] Poigenfurst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: results of 122 operations. Injury. 1992; 23:237-241.[22] Giddie J, Fisher R, White A. A rare anatomical variant: transosseous supraclavicular nerve identified during clavicle fracture fixation. J Surg Case Rep. 2017;2017(11):rjx230.[23] Strauss EJ, Egol KA, France MA, et al. Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures. J Shoulder Elbow Surg. 2007; 16:280-284.[24] Eickhoff A, Fischer M, Gebhard F, et al. Complications after intramedullary stabilization of clavicle fractures. Der Unfallchirurg. 2018.[25] Liu HH, Chang CH, Chia WT, et al. Comparison of plates versus intramedullary nails for fixation of displaced midshaft clavicular fractures. J Trauma. 2010; 69:E82-87.[26] Jorgensen A, Troelsen A, Ban I. Predictors associated with nonunion and symptomatic malunion following non-operative treatment of displaced midshaft clavicle fractures--a systematic review of the literature. Int Orthop. 2014; 38: 2543-2549.[27] van der V, Timmers TK, Broeders I, et al. Displaced clavicle fractures in cyclists: return to athletic activity after anteroinferior plate fixation. Clin J Sport Med. 2017.[28] Andrade-Silva FB, Kojima KE, Joeris A, et al. Single, superiorly placed reconstruction plate compared with flexible intramedullary nailing for midshaft clavicular fractures: a prospective, randomized controlled trial. J Bone Joint Surg. 2015; 97:620-626.[29] Duan X, Zhong G, Cen S, et al. Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2011; 20:1008-1015.[30] Houwert RM, Wijdicks FJ, Steins Bisschop C, et al. Plate fixation versus intramedullary fixation for displaced mid-shaft clavicle fractures: a systematic review. Int Orthop. 2012; 36: 579-585.[31] 张峻玮,聂伟志,陈玲玲,等. 髓内钉与接骨板治疗锁骨中段骨折的前瞻性随机对照研究[J]. 中华创伤骨科杂志, 2016,18(7): 558-563. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [5] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [6] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [7] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [8] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [9] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [10] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [11] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [12] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [13] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [14] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [15] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||