Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (35): 7649-7655.doi: 10.12307/2025.975
Previous Articles Next Articles
A systematic review of osteoporosis-specific quality-of-life scales
Yan Jing1, 2, Qin Qiujun1, Li Fen3, Zhou Jun1, Ding Yuanyuan1, Jin Chunlin1
- 1Shanghai Health Development Research Center (Shanghai Medical Information Center), Shanghai 200031, China; 2School of Public Health, Fudan University, Shanghai 200032, China; 3Financial Management Affairs Center of Shanghai Municipal Health Commission, Shanghai 200040, China
-
Received:2024-10-21Accepted:2024-12-17Online:2025-12-18Published:2025-05-07 -
Contact:Jin Chunlin, PhD, Professor, Shanghai Health Development Research Center (Shanghai Medical Information Center), Shanghai 200031, China -
About author:Yan Jing, Master candidate, Shanghai Health Development Research Center (Shanghai Medical Information Center), Shanghai 200031, China; School of Public Health, Fudan University, Shanghai 200032, China
CLC Number:
Cite this article
Yan Jing, Qin Qiujun, Li Fen, Zhou Jun, Ding Yuanyuan, Jin Chunlin. A systematic review of osteoporosis-specific quality-of-life scales[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7649-7655.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
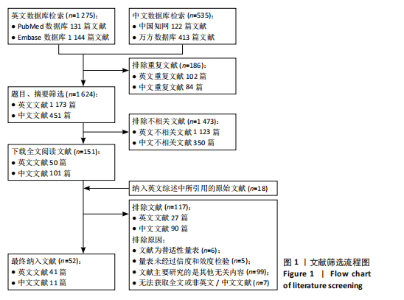
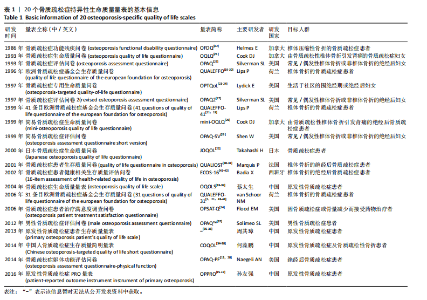
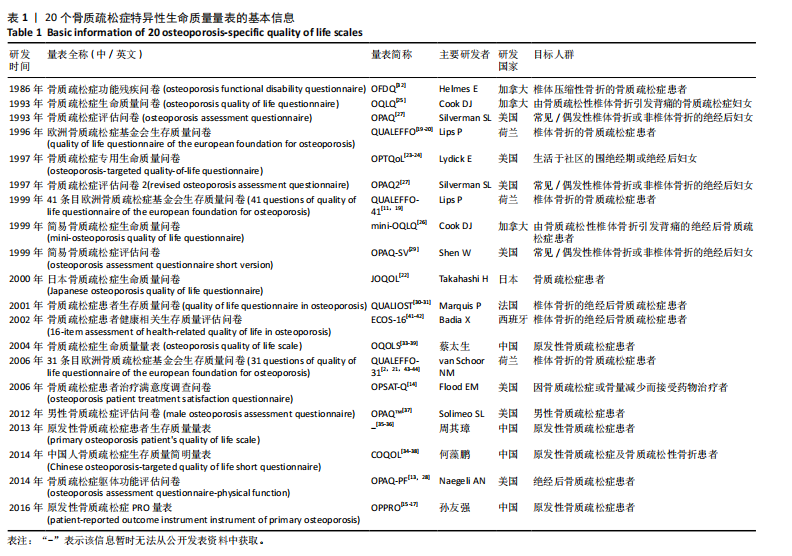
2.1 文献检索结果与量表纳入 文献筛选流程如图1所示。共检出英文综述文献1 275篇,中文文献535篇。剔除重复文献186篇,基于题目与摘要对文献进行初步筛选,保留51篇英文文献和100篇中文文献。进一步阅读文献全文,对其进行再次筛选,并根据英文综述文献中所引用的参考文献,纳入18篇相关文献。最终纳入42篇英文文献和10篇中文文献,共计52篇文献,从中提取54个量表,纳入20个符合此研究纳入标准的骨质疏松症特异性生命质量量表。经过进一步检索,追溯到上述纳入量表所对应的原始研发文献34篇[2,11,13-44],作为综述所提取的信息出处。各量表相对应的原始研发文献数量为1-4篇。 2.2 量表基本信息、发展趋势与目标人群 纳入的20个骨质疏松症特异性生命质量量表的基本信息见表1。20个量表的研发时间跨度约为30年"
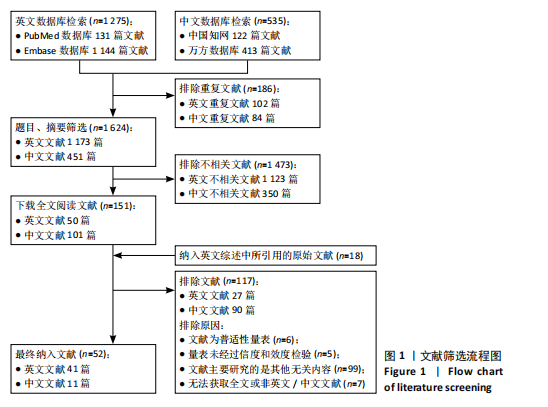
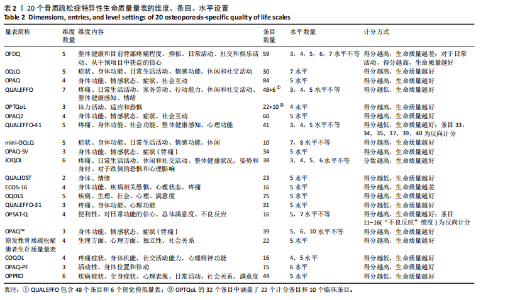
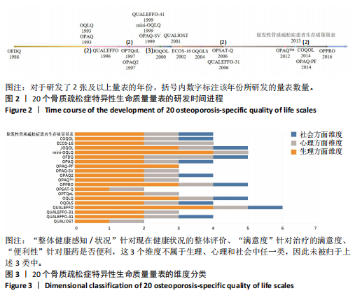
(1986-2016年)(图2),量表主要的研发者集中于美国、加拿大、中国、荷兰这4个国家。从研发时间进程的角度来看,骨质疏松症特异性生命质量量表的研发主要集中于20世纪末、21世纪初。初步起始阶段为20世纪80年代,由加拿大学者率先研发针对骨质疏松症的疾病特异性生命质量量表,骨质疏松症功能残疾问卷(osteoporosis functional disability questionnaire,OFDQ)量表是国际上首个骨质疏松症特异性生命质量量表[32]。此后,从20世纪90年代开始,随着各国学者越发认识到开发疾病特异性量表的重要性,无论是对量表的研发还是对量表信效度的检验均进入快速发展阶段。以美国、荷兰、加拿大等为代表的欧美国家先后研发了10余种量表;此外,日本也研发了适用于日本骨质疏松症患者的日本骨质疏松症生命质量问卷(Japanese osteoporosis quality of life questionnaire,JOQOL)量表[22],这是首个专门为亚洲人群设计的骨质疏松症特异性生命质量量表,其在日本得到了广泛的应用。 自2004年起,蔡太生等[39]首次参照国内外公认的36维健康调查简表(short form 36-item,SF-36)和世界卫生组织生存质量测定量表(100-item World Health Organization quality of life assessment,WHOQOL-100),在文献综述和咨询专家意见的基础上,结合中国国情、原发性骨质疏松症的发病特点等设计了第一个中国骨质疏松症特异性生命质量量表——骨质疏松症生命质量量表(osteoporosis quality of life scale,OQOLS)。此后,原发性骨质疏松症患者生存质量量表[35]、中国人骨质疏松症生存质量简明量表(Chinese osteoporosis-targeted quality of life short questionnaire,COQOL)[34-38]、原发性骨质疏松症PRO量表(patient- reported outcome instrument instrument of primary osteoporosis,OPPRO)等基于中国人群健康偏好的量表被陆续研发[15-17],并且均经过了信效度检验,可以较好地测量中国原发性骨质疏松症患者的生命质量。同时,也有部分国外骨质疏松症特异性生命质量量表经过了汉化,如骨质疏松症患者健康相关生存质量评估问卷(16-item assessment of health-related quality of life in osteoporosis,ECOS-16)[41-42]、31条目欧洲骨质疏松症基金会生存质量问卷(31 questions of quality of life questionnaire of the european foundation for osteoporosis,QUALEFFO-31)[21]、简易骨质疏松症评估问卷(osteoporosis assessment questionnaire short version,OPAQ-SV)[29]、男性骨质疏松症评估问卷(male osteoporosis assessment questionnaire,OPAQ?) [37],使之适用于中国人群。 从量表所针对的目标人群而言,有相当一部分量表对患者的骨折部位做出了限制——20个骨质疏松症特异性生命质量量表中有8个针对椎体骨折的患者而研发;此外,另有3个骨质疏松症评估问卷(osteoporosis assessment questionnaire,OPAQ)系列量表同样适用于椎体骨折患者[29]。同时,有10个量表对患者的性别进行了限制,其中9个量表针对的目标人群为绝经后妇女,仅有1个是专门为男性骨质疏松症患者而研发的[37]。大部分骨质疏松症特异性生命质量量表的目标对象为原发性骨质疏松症患者,且多为绝经后妇女伴/不伴骨质疏松性椎体骨折,这可能与骨质疏松症的临床及流行病学特点有关[7-9]。 2.3 量表维度、条目、水平设置与梳理 对于纳入的20个骨质疏松症特异性生命质量量表的条目、维度及水平设置详见表2。量表的维度数量"
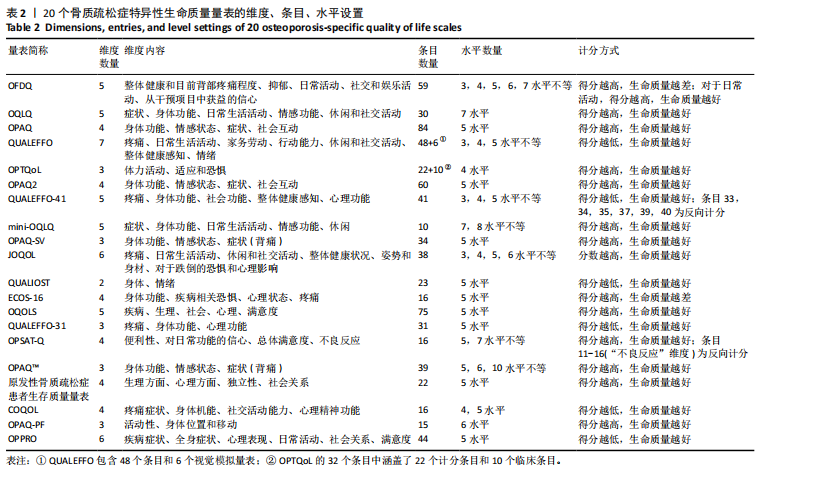
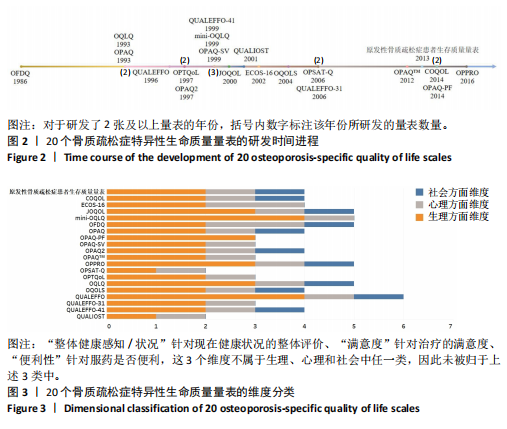
在2-7个之间,半数以上的量表集中于3,4,5个维度,少数为2,6,7个维度。与早期量表相比,后期量表的维度数量呈现减少的趋势。该研究进一步根据WHO对于健康的定义对量表的维度进行了梳理[45],分别将各量表的维度归纳为生理、心理和社会3个方面(图3)。所有量表均设有生理方面的维度,且大部分量表至少包括2个以上生理维度;绝大部分量表均设置了心理维度,只有骨质疏松症躯体功能评估问卷(osteoporosis assessment questionnaire-physical function,OPAQ-PF)是专门针对身体功能研发的量表而未设置心理维度;仅有11个量表设置了社会维度。生理方面维度设置较为多元,可以进一步细分为日常活动、症状(如疼痛)、身体功能、独立性(含移动/行动能力)这4个类别;心理方面维度涵盖了正面情绪(信心)、负面情绪(恐惧、抑郁)这2个方面;而社会方面维度则可归纳为社会关系、社会互动。此外,欧洲骨质疏松症基金会生存质量问卷(quality of life questionnaire of the european foundation for osteoporosis,QUALEFFO)、41条目欧洲骨质疏松症基金会生存质量问卷(41 Questions of Quality of Life Questionnaire of the European Foundation for Osteoporosis,QUALEFFO-41)、JOQOL设置了对于整体健康评价的维度,而OQOLS、骨质疏松症患者治疗满意度调查问卷(osteoporosis patient treatment satisfaction questionnaire,OPSAT-Q)、OPPRO则设置了对于治疗满意度的维度;OPSAT-Q还另设了服药便利性的维度。与早期量表相比,后期量表开始关注成年骨质疏松症患者对于治疗的满意度。 量表条目数量最多者为OPAQ(84条),最少者为mini-OQLQ(10条)。与初始量表相比,后期研发的量表条目数量呈现减少的趋势,如骨质疏松症评估问卷2(revised osteoporosis assessment questionnaire,OPAQ2)、OPAQ-SV、OPAQ?、OPAQ-PF由最初84个条目依次减少为60,34,39,15个条目。此外,少数量表条目设置有特殊之处,例如QUALEFFO除了48个条目,还包含了6个视觉模拟量表;骨质疏松症专用生命质量量表(osteoporosis-targeted quality-of-life questionnaire,OPTQoL)所设置的32个条目中除了22个计分条目(涵盖了体力活动、适应和恐惧这3个维度)外,还设置了10个不计分的临床条目,涉及了与骨质疏松症相关的变化、健康和人口统计学信息。 各量表条目下设水平数量最多者"

为10个水平,最少者为3个水平;以5个水平最为常见,其次是4个水平。同一量表存在设置不同水平的情况,例如OFDQ设置了3-7个水平不等,JOQOL则设置了3-6个水平不等;然而,大部分量表所设置的水平数量只有1种。大部分量表的计分方式较为统一(得分越高,表示生命质量较好/差),但是少数量表存在同一量表内不同条目反向计分的情况,例如OFDQ和QUALEFFO-41。此外,大部分量表的计分方式均为将条目得分先转换为百分制,再根据相应的计分规则对患者的生命质量进行评估。 2.4 量表的构建过程 此研究所纳入大部分量表的构建过程均基于现有资料,同时根据学者或临床医生建议、患者访谈、焦点小组讨论等进行修订。以JOQOL为例,专家委员会基于OPAQ和QUALEFFO-41量表生成条目清单,然后根据信效度检验的结果删减条目,最后由委员会进一步修改量表[22];COQOL则参照了QUALEFFO-41、OPTQoL、OPSAT-Q量表,其构建以QUALEFFO-41问卷为蓝本,补充了OPTQoL问卷中特异性较强的条目如体力活动、适应和恐惧等,以及OPSAT-Q问卷中评估患者对治疗满意度的条目,并在文献综述、专家咨询、中国国情和原发性骨质疏松症的发病特点等基础上设计量表[34-38]。 另有部分量表则既包含了独立设计的条目,也从已有量表中选取了部分条目。例如QUALEFFO,条目内容主要源自于赴门诊就医的骨质疏松症患者所反馈的普遍问题,该量表也从地中海骨质疏松症研究(the Mediterranean osteoporosis study,MEDOS)和欧洲椎骨骨质疏松症研究(the European vertebral osteoporosis study,EVOS)问卷中选择了少数条目[19-20]。 此外,也有少数量表通过构建条目池、根据经典测量理论和项目反应理论筛选条目的方式设计量表,这种构建方式于近年来逐渐兴起[4]。OPPRO就是其中的代表,构建时首先通过问诊及问卷调查等方式收集患者相关信息,构建原发性骨质疏松症患者报告结果的量表数据库;其次,建立研究组,通过文献综述、量表的概念框架构建、条目的搜集、条目的定性采访(专家咨询、由患者组成的核心小组讨论)、模拟小范围测试等方式进行逐一考量;最后,根据经典测量理论和项目反应理论筛选条目。"

| [1] HARALDSTAD K, WAHL A, ANDENÆS R, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. 2019;28(10):2641-2650. [2] ZHOU C, LI Q, HUANG S, et al. Validation of the simplified Chinese version of the quality of life questionnaire of the European foundation for osteoporosis (QUALEFFO-31). Eur Spine J. 2016;25(1):318-324. [3] 陈丕楠,谢诗桐,贺小宁,等.中国普适性生命质量量表系统综述[J].中国卫生事业管理, 2022,39(8):630-635. [4] 谢诗桐,陈丕楠,贺小宁,等.国内外普适性健康效用量表综述研究[J].中国卫生政策研究, 2020,13(8):58-68. [5] 中华医学会骨质疏松和骨矿盐疾病分会.原发性骨质疏松症诊疗指南(2022)[J].中华内分泌代谢杂志,2023,39(5):377-406. [6] SÖZEN T, ÖZIŞIK L, BAŞARAN NÇ. An overview and management of osteoporosis. Eur J Rheumatol. 2017;4(1):46-56. [7] WANG L, YU W, YIN X, et al. Prevalence of Osteoporosis and Fracture in China: The China Osteoporosis Prevalence Study. JAMA Netw Open. 2021;4(8):e2121106. [8] 赵碧仪,孙伟鹏,林青,等.骨质疏松症和关节炎之间的关联:一项两样本双向孟德尔随机化研究[J].暨南大学学报(自然科学与医学版), 2024,45(4):366-377. [9] YU F, XIA W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China. Arch Osteoporos. 2019;14(1):32. [10] GAO S, ZHAO Y. Quality of life in postmenopausal women with osteoporosis: a systematic review and meta-analysis. Qual Life Res. 2023;32(6): 1551-1565. [11] CHOO YW, MOHD TAHIR NA, MOHAMED SAID MS, et al. Health-related quality of life in osteoporosis: a systematic review of measurement properties of the QUALEFFO-41. Osteoporos Int. 2024;35(5):745-757. [12] 何藻鹏,杨德鸿.骨质疏松症专用生存质量量表研究与应用进展[J].中国组织工程研究,2014, 18(48):7862-7866. [13] NAEGELI AN, NIXON A, BURGE R, et al. Development of the Osteoporosis Assessment Questionnaire--physical Function (OPAQ-PF): an osteoporosis-targeted, patient-reported outcomes (PRO) measure of physical function. Osteoporos Int. 2014;25(2):579-588. [14] FLOOD EM, BEUSTERIEN KM, GREEN H, et al. Psychometric evaluation of the Osteoporosis Patient Treatment Satisfaction Questionnaire (OPSAT-Q), a novel measure to assess satisfaction with bisphosphonate treatment in postmenopausal women. Health Qual Life Outcomes. 2006;4:42. [15] 孙友强.原发性骨质疏松症PRO量表的初步研制与评价[D].广州:广州中医药大学,2015. [16] 孙友强,邵敏,何挺,等.原发性骨质疏松症PRO量表的科学性考核[J].中国骨质疏松杂志, 2016,22(8):1008-1011. [17] 孙友强,邵敏,姜涛,等.原发性骨质疏松症PRO量表的初步研制[J].中国骨质疏松杂志, 2016,22(7):799-804. [18] LIPS P, AGNUSDEI D, CAULIN F, et al. The development of a European questionnaire for quality of life in patients with vertebral osteoporosis. Scand J Rheumatol Suppl. 1996;103: 84-85; discussion 86-88. [19] LIPS P, COOPER C, AGNUSDEI D, et al. Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporos Int. 1999;10(2):150-160. [20] LIPS P, COOPER C, AGNUSDEI D, et al. Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis. Osteoporos Int. 1997;7(1):36-38. [21] VAN SCHOOR NM, KNOL DL, GLAS CA, et al. Development of the Qualeffo-31, an osteoporosis-specific quality-of-life questionnaire. Osteoporos Int. 2006;17(4):543-551. [22] KUMAMOTO K, NAKAMURA T, SUZUKI T, et al. Validation of the Japanese Osteoporosis Quality of Life Questionnaire. J Bone Miner Metab. 2010;28(1):1-7. [23] LYDICK E, ZIMMERMAN SI, YAWN B, et al. Development and validation of a discriminative quality of life questionnaire for osteoporosis (the OPTQoL). J Bone Miner Res. 1997;12(3):456-463. [24] CHANDLER JM, MARTIN AR, GIRMAN C, et al. Reliability of an Osteoporosis-Targeted Quality of Life Survey Instrument for use in the community: OPTQoL. Osteoporos Int. 1998;8(2): 127-135. [25] COOK DJ, GUYATT GH, ADACHI JD, et al. Quality of life issues in women with vertebral fractures due to osteoporosis. Arthritis Rheum. 1993;36(6):750-756. [26] COOK DJ, GUYATT GH, ADACHI JD, et al. Development and validation of the mini-osteoporosis quality of life questionnaire (OQLQ) in osteoporotic women with back pain due to vertebral fractures. Osteoporosis Quality of Life Study Group. Osteoporos Int. 1999;10(3):207-213. [27] RANDELL AG, BHALERAO N, NGUYEN TV, et al. Quality of life in osteoporosis: reliability, consistency, and validity of the Osteoporosis Assessment Questionnaire. J Rheumatol. 1998; 25(6):1171-1179. [28] NIXON A, KERR C, DOLL H, et al. Osteoporosis Assessment Questionnaire-Physical Function (OPAQ-PF): a psychometrically validated osteoporosis-targeted patient reported outcome measure of daily activities of physical function. Osteoporos Int. 2014;25(6):1775-1784. [29] SILVERMAN SL. The Osteoporosis Assessment Questionnaire (OPAQ): A reliable and valid disease-targeted measure of health-related quality of life (HRQOL) in osteoporosis. Qual Life Res. 2000;9(Suppl 1):767-774. [30] MARQUIS P, CIALDELLA P, DE LA LOGE C. Development and validation of a specific quality of life module in post-menopausal women with osteoporosis: the QUALIOST. Qual Life Res. 2001; 10(6):555-566. [31] DE LA LOGE C, SULLIVAN K, PINKNEY R, et al. Cross-cultural validation and analysis of responsiveness of the QUALIOST: QUAlity of Life questionnaire In OSTeoporosis. Health Qual Life Outcomes. 2005;3:69. [32] HELMES E, HODSMAN A, LAZOWSKI D, et al. A questionnaire to evaluate disability in osteoporotic patients with vertebral compression fractures. J Gerontol A Biol Sci Med Sci. 1995; 50(2):M91-98. [33] 刘健,蔡太生,吴萍陵,等.原发性骨质疏松症患者生活质量量表的信度与效度研究[J].中国临床心理学杂志,2004,12(2):131-132. [34] 何藻鹏,杨德鸿,李丽.中国人骨质疏松症生存质量简明量表的编制与信效度[J].南方医科大学学报,2014,34(11):1637-1641. [35] 周其璋,高恒,李大刚.原发性骨质疏松症患者生存质量量表的制订及评价[J].中国骨质疏松杂志,2013,19(8):820-822+819. [36] 高恒.原发性骨质疏松症患者生存质量量表的初步制定及评价[D].广州:广州中医药大学, 2009. [37] SOLIMEO SL, SILVERMAN SL, CALDERON AD, et al. Measuring health-related quality of life (HRQOL) in osteoporotic males using the Male OPAQ. Osteoporos Int. 2012;23(3):841-852. [38] 何藻鹏. 中国人骨质疏松症专用生存质量量表的设计与信效度研究[D].广州:南方医科大学, 2014. [39] 蔡太生,刘健,吴萍陵,等.原发性骨质疏松症生活质量量表的编制策略及条目筛选[J].中国行为医学科学,2004,13(2):221-222. [40] 董圣梅.原发性骨质疏松症患者生活质量评价及其影响因素研究[D].长沙:中南大学,2010. [41] BADIA X, DÍEZ-PÉREZ A, LAHOZ R, et al. The ECOS-16 questionnaire for the evaluation of health related quality of life in post-menopausal women with osteoporosis. Health Qual Life Outcomes. 2004;2:41. [42] BADIA X, PRIETO L, ROSET M, et al. Development of a short osteoporosis quality of life questionnaire by equating items from two existing instruments. J Clin Epidemiol. 2002;55(1):32-40. [43] LAI BM, TSANG SW, LAM CL, et al. Validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO-31) in Chinese. Clin Rheumatol. 2010;29(9):965-972. [44] LI WC, CHEN YC, YANG RS, et al. Taiwanese Chinese translation and validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis 31 (QUALEFFO-31). J Formos Med Assoc. 2013;112(10):621-629. [45] LEONARDI F. The Definition of Health: Towards New Perspectives. Int J Health Serv. 2018;48(4): 735-748. [46] 高继红,段智霞,许素琴.中文版ECOS-16问卷在骨质疏松患者中的应用信效度[J].临床与病理杂志,2017,37(9):1926-1931. [47] 赵新爽,刘霖,张洛灵,等.绝经后女性骨质疏松症患者生活质量问卷的汉化及信效度检验[J].中华护理教育,2023,20(6):740-744. [48] 张银萍,韦欢欢,夏茹意,等.女性骨质疏松症生活质量简易评价问卷的本土化研究[J].护理研究,2015,29(34):4245-4249. [49] 张银萍,韦欢欢,夏茹意,等.中文版男性骨质疏松症生命质量评估问卷的信效度检验[J].中国实用护理杂志,2015,31(24):1805-1809. [50] TADIC I, VUJASINOVIC STUPAR N, TASIC L, et al. Validation of the osteoporosis quality of life questionnaire QUALEFFO-41 for the Serbian population. Health Qual Life Outcomes. 2012;10:74. [51] NAGAMMAI T, MOHAZMI M, LIEW SM, et al. Validation of the Malay version of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO-41) in Malaysia. Qual Life Res. 2015;24(8):2031-2037. [52] HUO R, WEI C, HUANG X, et al. Mortality associated with osteoporosis and pathological fractures in the United States (1999-2020): a multiple-cause-of-death study. J Orthop Surg Res. 2024;19(1):568. [53] AMARILLA-DONOSO FJ, LÓPEZ-ESPUELA F, RONCERO-MARTÍN R, et al. Quality of life in elderly people after a hip fracture: a prospective study. Health Qual Life Outcomes. 2020;18(1):71. [54] AMARILLA-DONOSO FJ, RONCERO-MARTIN R, LAVADO-GARCIA JM, et al. Quality of life after hip fracture: a 12-month prospective study. Peer J. 2020;8:e9215. [55] ZARINFAR Y, PANAHI N, HOSSEINPOUR M, et al. The association between osteoporosis and quality of life among older adults in Southern Iran: findings from the Bushehr Elderly Health Program. BMC Geriatr. 2024;24(1):766. [56] FISCHER V, HAFFNER-LUNTZER M. Interaction between bone and immune cells: Implications for postmenopausal osteoporosis. Semin Cell Dev Biol. 2022;123:14-21. |
| [1] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [2] | Ma Chi, Wang Ning, Chen Yong, Wei Zhihan, Liu Fengji, Piao Chengzhe. Application of 3D-printing patient-specific instruments combined with customized locking plate in opening wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1863-1869. |
| [3] | Zhao Jiyu, Wang Shaowei. Forkhead box transcription factor O1 signaling pathway in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1923-1930. |
| [4] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [5] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [6] | Zhao Jiacheng, Ren Shiqi, Zhu Qin, Liu Jiajia, Zhu Xiang, Yang Yang. Bioinformatics analysis of potential biomarkers for primary osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1741-1750. |
| [7] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [8] | Li Yueyao, Zhang Min, Yang Jiaju. Cistanoside A mediates p38/MAPK pathway to inhibit osteoclast activity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1144-1151. |
| [9] | Zheng Lin, Jin Wenjun, Luo Shanshan, Huang Rui, Wang Jie, Cheng Yuting, An Zheqing, Xiong Yue, Gong Zipeng, Liao Jian. Eucommia ulmoides promotes alveolar bone formation in ovariectomized rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1159-1167. |
| [10] |
Huang Xiaobin, Ge Jirong, Li Shengqiang, Xie Lihua, Huang Jingwen, He Yanyan, Xue Lipeng.
Mechanisms of different yin nourishing and kidney tonifying methods on osteoclastysis pathway in ovariectomized rats #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1214-1219.
|
| [11] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [12] | Lan Shuangli, Xiang Feifan, Deng Guanghui, Xiao Yukun, Yang Yunkang, Liang Jie. Naringin inhibits iron deposition and cell apoptosis in bone tissue of osteoporotic rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 888-898. |
| [13] | Wang Dongyang, Yang Qiaohui, Lin Xinchao. Relationship between vitamin D levels and reproductive characteristics and exercise dietary situation in postmenopausal women [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1021-1025. |
| [14] | Zhang Lichuang, Yang Wen, Ding Guangjiang, Li Peikun, Xiao Zhongyu, Chen Ying, Fang Xue, Zhang Teng. Dispersion effect of bone cement after vertebroplasty using individualized unilateral external pedicle approach and bilateral pedicle approach [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 800-808. |
| [15] | Zhang Xiongjinfu, Chen Yida, Cheng Xinyi, Liu Daihui, Shi Qin . Exosomes derived from bone marrow mesenchymal stem cells of young rats to reverse senescence in aged rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7709-7718. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||