Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (24): 5212-5223.doi: 10.12307/2025.703
Previous Articles Next Articles
Effect of different stimulation modalities of non-invasive brain stimulation on cognitive function in patients with Parkinson’s disease: a network Meta-analysis
Zhao Yuxin1, Zhang Deqi1, Bi Hongyan2
- 1College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 2Department of Rehabilitation, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250012, Shandong Province, China
-
Received:2024-07-27Accepted:2024-09-04Online:2025-08-28Published:2025-02-05 -
Contact:Bi Hongyan, MS, Chief physician, Department of Rehabilitation, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250012, Shandong Province, China -
About author:Zhao Yuxin, Master’s candidate, College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
Supported by:Shandong Province Scientific Program for Traditional Chinese Medicine, No. 2022090T (to BHY)
CLC Number:
Cite this article
Zhao Yuxin, Zhang Deqi, Bi Hongyan. Effect of different stimulation modalities of non-invasive brain stimulation on cognitive function in patients with Parkinson’s disease: a network Meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5212-5223.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

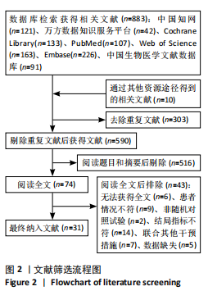
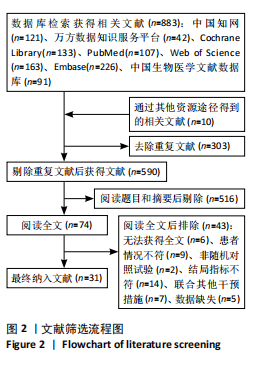
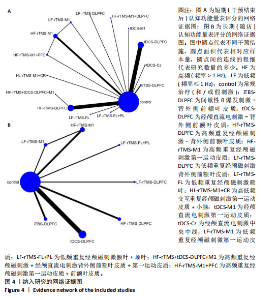
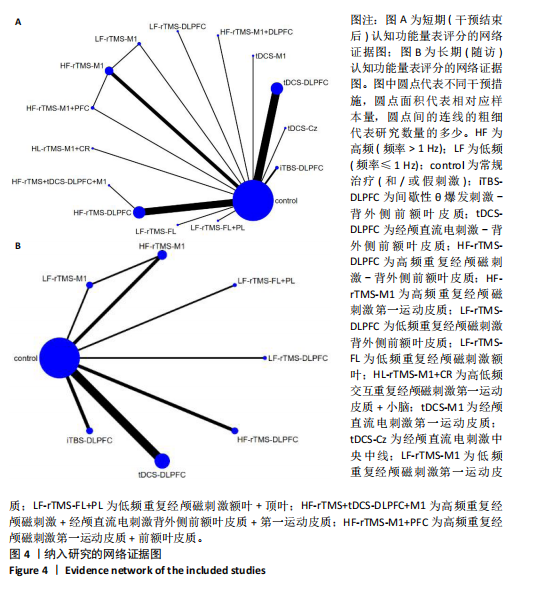
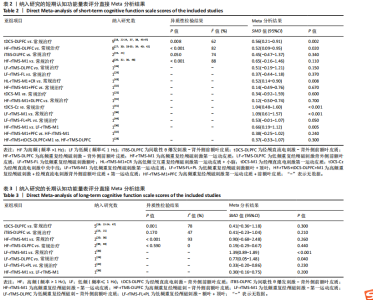
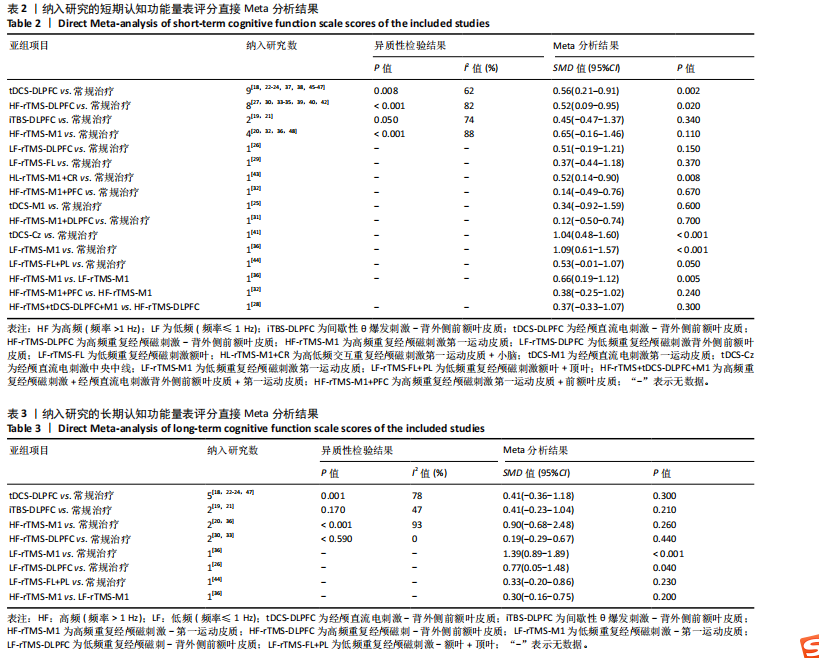
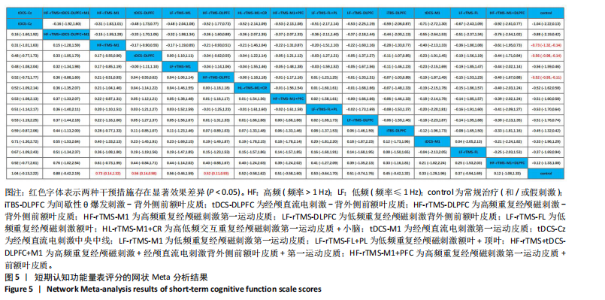
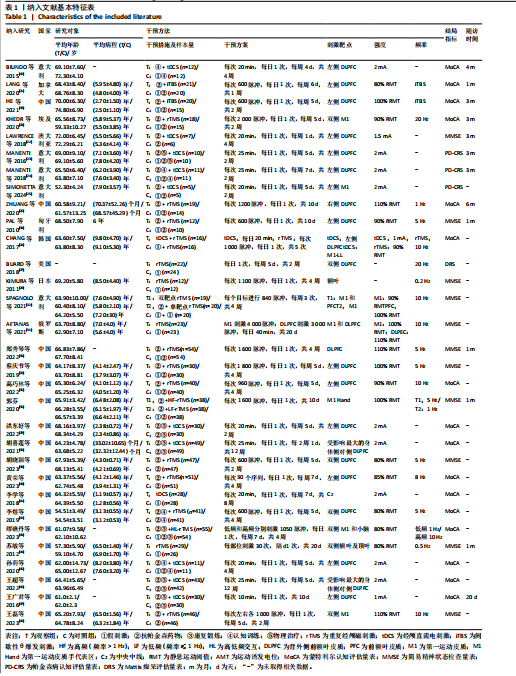
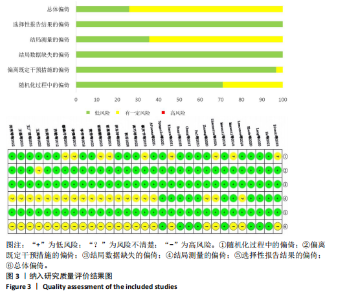
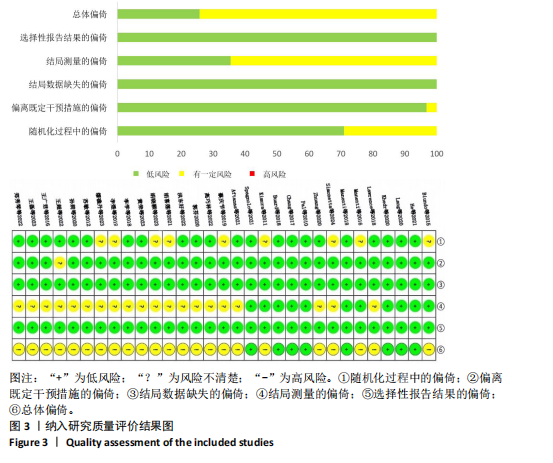
2.2 纳入文献基本特征 共纳入31篇文献,涉及1 670例帕金森病患者,其中试验组共873例,对照组共797例。帕金森病患者年龄多在52-75岁;病程为1-9年;干预周期最短为1周,最长为12周。31项研究均报告了短期认知功能评分[18-48]。有13项研究报告了长期认知功能评分[18-24,26,30,33,36,44,47]。纳入研究共涉及14种非侵入性脑刺激的不同治疗方式,其中间歇性θ爆发刺激背外侧前额叶皮质(intermittent theta burst stimulation-dorsolateralprefrontal cortex,iTBS-DLPFC)2项[19,21]、经颅直流电刺激背外侧前额叶皮质(transcranial direct current stimulation-dorsolateralprefrontal cortex,tDCS- DLPFC)9项[18,22-24,37-38,45-47]、高频重复经颅磁刺激背外侧前额叶皮质(high- frequency repetitive transcranial magnetic stimulation-dorsolateralprefrontal cortex,HF-rTMS-DLPFC)9项[27-28,30,33-35,39-40,42]、高频重复经颅磁刺激第一运动皮质(high-frequency repetitive transcranial magnetic stimulation-primary motor cortex,HF-rTMS-M1)4项[20,32,36,48]、低频重复经颅磁刺激背外侧前额叶皮质(low-frequency repetitive transcranial magnetic stimulation-dorsolateralprefrontal cortex,LF-rTMS-DLPFC)[26]、低频重复经颅磁刺激额叶(low-frequency repetitive transcranial magnetic stimulation-frontal lobe,LF-rTMS-FL)[29]、高低频交互重复经颅磁刺激第一运动皮质+小脑(high and low frequency repetitive transcranial magnetic stimulation-primary motor cortex+cerebellar region,HL-rTMS-M1+CR)[43]、经颅直流电刺激第一运动皮质(transcranial direct current stimulation-primary motor cortex,tDCS-M1)[25]、经颅直流电刺激中央中线(transcranial direct current stimulation-Central zero,tDCS-Cz)[41]、低频重复经颅磁刺激第一运动皮质(low-frequency repetitive transcranial magnetic stimulation-primary motor cortex,LF-rTMS-M1)[36]、低频重复经颅磁刺激额叶+顶叶(low-frequency repetitive transcranial magnetic stimulation-frontal lobe+parietal lobe,LF-rTMS-FL+PL)[44]、高频重复经颅磁刺激+经颅直流电刺激背外侧前额叶皮质+第一运动皮质(high-frequency repetitive transcranial magnetic stimulation+ transcranial direct current stimulation-dorsolateralprefrontal cortex+ primary motor cortex,HF-rTMS+tDCS-DLPFC+M1)[28]、高频重复经颅磁刺激第一运动皮质+前额叶皮质(high-frequency repetitive transcranial magnetic stimulation-primary motor cortex+prefrontal cortex,HF-rTMS-M1+PFC)各1项[32]。 此外,需要说明的是定义刺激频率 > 1 Hz为高频,低频为刺激频率≤1 Hz。文献基本特征见表1。 2.3 纳入研究的质量评价结果 在31篇文献中,“低风险”8篇[19-21,24,27-28,30,32]、“有一定风险”23篇[18,22-23,25-26,29,31,33-48]、“高风险”0篇。31篇文献均报告了随机分组,其中21项研究交代了随机序列的产生方式[19-22,24,26-28,30-31,33,35-37,40-41,44-48],如随机数字表法、计算机随机法;盲法方面,23项对参与者实施盲法[18-36,41,43-45],11项对参与者和研究者均实施盲法[18-21,23-24,27-30,32];31项研究均数据完整,未出现结局数据缺失的偏倚,未出现结果的选择性报道,偏倚风险较低,见图3。 2.4 传统Meta分析结果 短期认知功能量表评分共纳入31项研究[18-48],长期认知功能量表评分共纳入13项研究[18-24,26,30,33,36,44,47],2项结局指标的传统Meta分析结果均表明纳入研究间异质性较高。以刺激方式为参数进行亚组分析后异质性依然较高,因此对结果进行描述性分析。研究结果表明,短期认知功能量表评分的传统Meta分析包含14种刺激方式;长期认知功能量表评分的传统Meta分析包含7种刺激方式。tDCS-DLPFC,HF-rTMS-DLPFC,HL-rTMS-M1+CR,tDCS-Cz,LF-rTMS-M1对短期认知功能的改善效果显著优于常规治疗,HF-rTMS-M1对短期认知功能的改善效果显著优于LF-rTMS-M1,见表2。LF-rTMS-M1,LF-rTMS-DLPFC对长期认知功能的改善效果显著优于常规治疗,见表3。 2.5 网状Meta分析结果 2.5.1 短期认知功能改善效果 该结局指标共纳入31项研究[18-48],涉及14种非侵入性脑刺激的不同刺激方式,包括iTBS-DLPFC,tDCS-DLPFC,HF-rTMS-DLPFC,HF-rTMS-M1,LF-rTMS-DLPFC,LF-rTMS-FL,HL-rTMS-M1+CR,tDCS-M1,tDCS-Cz,LF-rTMS-M1,LF-rTMS-FL+PL,HF- rTMS+tDCS-DLPFC+M1,HF-rTMS-M1+PFC,证据网络见图4A。节点分析模型显示短期认知功能量表评分指标P=0.066,说明该结局指标整体直接比较的结果与间接比较的结果较为一致,故采用一致性模型进行分析。使用节点劈裂法进行局部不一致性检验,发现LF-rTMS-M1与HF-rTMS-M1,LF-rTMS-M1与常规治疗的直接比较与间接比较的结果存在不一致(P < 0.05),直接比较结果显示HF-rTMS-M1对短期认知功能的改善效果显著优于LF-rTMS-M1"
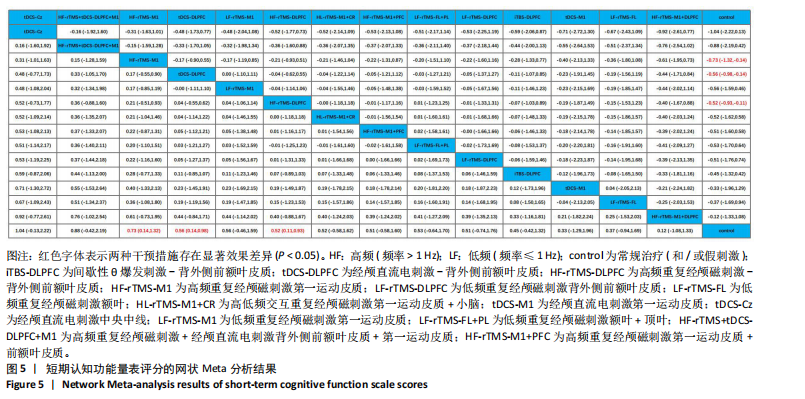
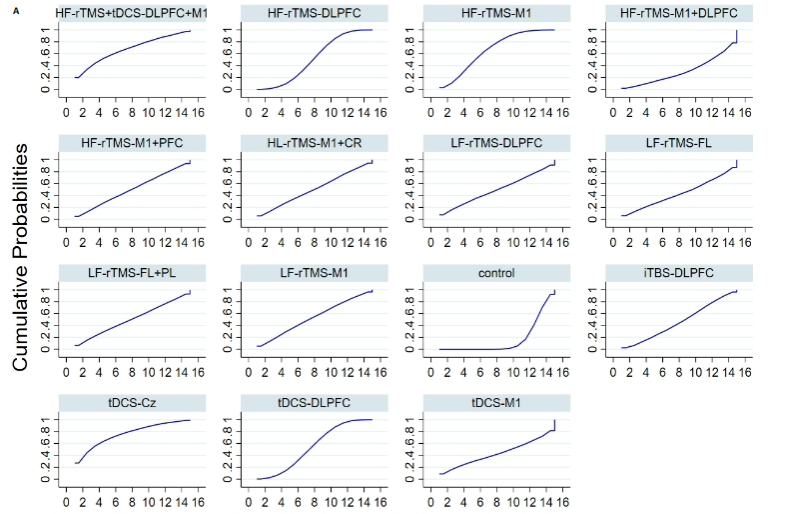
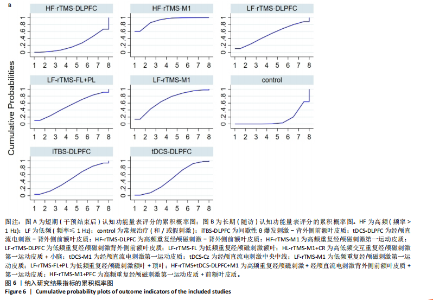
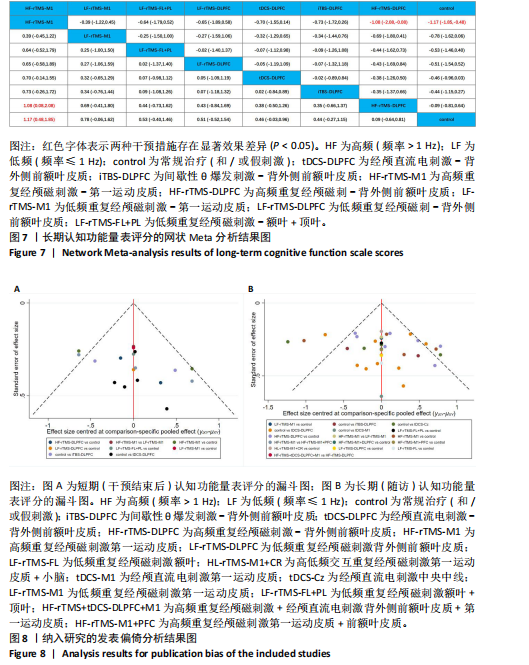
(SMD=0.66,95%CI=0.19-1.12,P=0.005);LF-rTMS-M1对短期认知功能的改善效果显著优于常规治疗(SMD=1.09,95%CI=0.61-1.57,P < 0.001),详见表2。 网状Meta分析结果显示,HF-rTMS-M1(SMD=0.73,95%CI=0.14-1.32,P < 0.05)、tDCS-DLPFC (SMD=0.56,95%CI=0.14-0.98,P < 0.05)、HF-rTMS- DLPFC(SMD=0.52,95%CI=0.11-0.93;P < 0.05)对短期认知功能的改善效果显著优于常规治疗,而尚无证据表明其他刺激方式对短期认知功能的改善效果优于常规治疗。14种刺激方式两两比较的结果显示,没有任何两项刺激方式之间呈现显著性差异(P > 0.05),详见图5。 基于累积概率图的治疗效果排序结果显示,14种刺激方式改善短期认知功能评分效果的优劣顺序依次为:tDCS-Cz(75.7%),HF-rTMS+tDCS-DLPFC+M1(67.5%),HF-rTMS-M1(66.2%),tDCS-DLPFC(54.4%),LF-rTMS-M1(53.4%),HF-rTMS-DLPFC(51.4%),HL-rTMS-M1+CR (50.7%),LF-rTMS-FL+PL(50.7%),HF-rTMS-M1+PFC(50.4%),LF-rTMS-DLPFC (49.7%),iTBS-DLPFC(46.5%),LF-rTMS-FL (43.5%),tDCS-M1(43.2%),HF-rTMS-M1+DLPFC(30.4%),详见图6A。 2.5.2 长期认知功能改善效果 该结局指标共纳入13项研究[18-24,26,30,33,36,44,47],涉及7种非侵入性脑刺激的不同刺激方式,包括tDCS-DLPFC,iTBS-DLPFC,HF-rTMS-M1,LF-rTMS-DLPFC,HF-rTMS-DLPFC,LF-rTMS-M1,LF-rTMS-FL+PL,证据网络见图4B。图中闭环来源于同一项三臂临床试验[36],因此未对该结果进行不一致性检验,可直接采用一致性模型进行分析。 网状Meta分析结果显示,HF-rTMS-M1(SMD=1.17,95%CI:0.48- 1.85,P < 0.05)对长期认知功能的改善效果显著优于常规治疗,尚无证据表明其他6种刺激方式对长期认知功能的改善效果优于常规治疗。7种刺激方式两两比较结果显示,HF-rTMS-M1对长期认知功能的改善效果显著优于HF-rTMS-DLPFC (SMD=1.08,95%CI:0.08-2.08,"

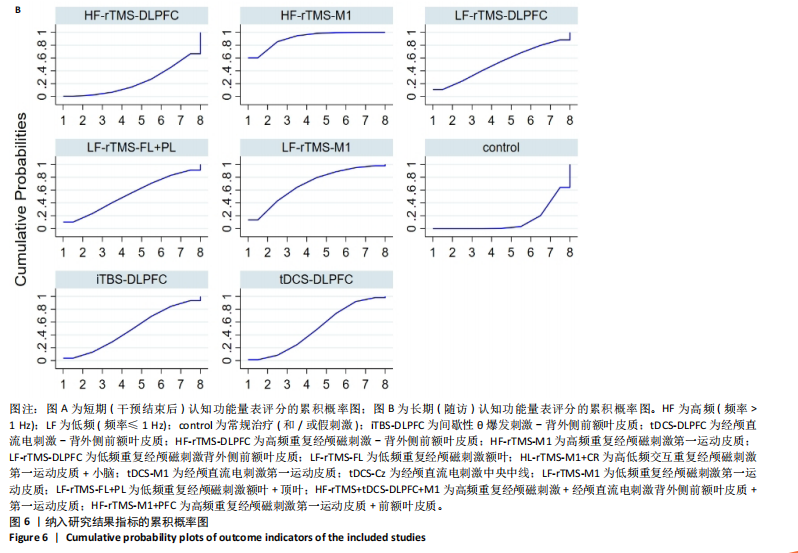
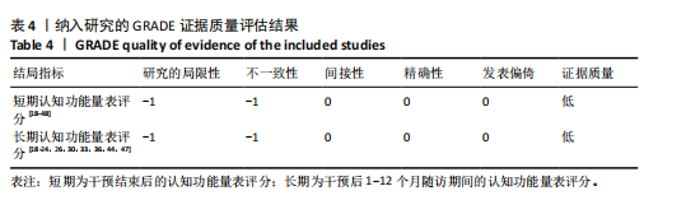
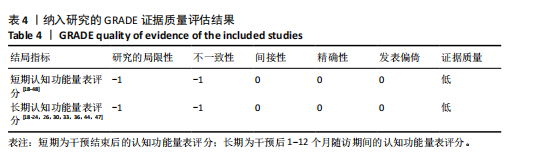
P=0.005),剩余两两比较结果未呈现显著性差异(P > 0.05),详见图7。 基于累积概率图的治疗效果排序结果显示,7种刺激方式改善短期认知功能评分效果的优劣顺序依次为:HF-rTMS-M1(91.2%),LF-rTMS-M1(68.8%),LF-rTMS-FL+PL (53.5%),LF-rTMS-DLPFC (52.3%),tDCS-DLPFC(49.5%),iTBS-DLPFC (48.8%),HF-rTMS-DLPFC (23.4%),详见图6B。 2.6 发表偏倚检验结果 文章对2个结局指标分别进行发表偏倚检验,结果表明短期认知功能量表的漏斗图内散点分布不均且有部分落在范围之外,见图8A,提示研究可能存在发表偏倚;长期认知功能量表的漏斗图基本对称,见图8B,提示存在发表偏倚的可能性较小,但对于结果仍需谨慎解释。同时进行不对称检验,短期认知功能量表评分Egger检验结果显示P=0.360(P > 0.05),长期认知功能量表评分Egger检验结果显示P=0.229(P > 0.05),没有证据表明所纳入的分析存在小样本研究效应。 2.7 GRADE证据分级结果 文章结局指标的证据强度受以下 5 个因素的影响:①研究的局限性:纳入研究在随机、分配隐藏和盲法方面描述不清楚;②不一致性:不同研究置信区间重叠程度较差,异质性检验的I2≥50%;③间接性:结局指标与评估目的关联不强;④精准性:置信区间过宽;⑤发表偏倚:漏斗图不对称且纳入随机对照试验都为小样本。文章纳入研究均为随机对照试验,但由于短期和长期认知功能量表评分大部分研究在随机、分配隐藏和盲法方面描述不清楚,因此对2项结局指标均进行降级;此外,短期和长期认知功能量表评分结果的异质性较高,因此对2项结局指标均进行降级。GRADE证据分级结果表明,短期和长期认知功能量表评分结局指标证据等级均为低级,见表4。 2.8 不良反应 有4篇文献报道了不良反应[20,30,35,40]。患者在接受干预过程中常出现轻微头痛、颈痛、针刺感、乏力等症状,往往在治疗后很快自行缓解,仅有一项报道患者因头痛和失眠拒绝完成疗程[20],表明非侵入性脑刺激安全性较高。"
| [1] MORRIS HR, SPILLANTINI MG, SUE CM, et al. The pathogenesis of Parkinson’s disease. Lancet. 2024;403(10423):293-304. [2] 陈芝君,马建,唐娜,等.中国帕金森病疾病负担变化趋势分析及预测[J].中国慢性病预防与控制,2022,30(9):649-654. [3] NEMADE D, SUBRAMANIAN T, SHIVKUMAR V. An update on medical and surgical treatments of Parkinson’s disease. Aging Dis. 2021;12(4):1021-1035. [4] ARMSTRONG MJ, OKUN MS. Diagnosis and treatment of Parkinson disease: a review. JAMA. 2020;323(6):548-560. [5] GOLDMAN JG, SIEG E. Cognitive impairment and dementia in Parkinson disease. Clin Geriatr Med. 2020;36(2):365-377. [6] LIU H, ZHONG Y, ZENG Z, et al. Drug-related problems in hospitalised Parkinson’s disease patients in China. Eur J Hosp Pharm. 2022;29(6):308-312. [7] SUDBRACK-OLIVEIRA P, RAZZA LB, BRUNONI AR. Non-invasive cortical stimulation: Transcranial direct current stimulation (tDCS). Int Rev Neurobiol. 2021;159:1-22. [8] ZEWDIE E, CIECHANSKI P, KUO HC, et al. Safety and tolerability of transcranial magnetic and direct current stimulation in children: Prospective single center evidence from 35 million stimulations. Brain Stimul. 2020;13(3):565-575. [9] FREEDBERG MV, REEVES JA, FIORITI CM, et al. Reproducing the effect of hippocampal network-targeted transcranial magnetic stimulation on episodic memory. Behav Brain Res. 2022;419:113707. [10] 杨钰琳,常万鹏,丁江涛,等.经颅直流电刺激不同靶点治疗帕金森病效果的网状Meta分析[J].中国组织工程研究, 2024,28(11):1797-1804. [11] DENG S, DONG Z, PAN L, et al. Effects of repetitive transcranial magnetic stimulation on gait disorders and cognitive dysfunction in Parkinson’s disease: a systematic review with meta-analysis. Brain Behav. 2022; 12(8):2697. [12] SUAREZ-GARCÍA DMA, GRISALES- CÁRDENAS JS, ZIMERMAN M, et al. Transcranial direct current stimulation to enhance cognitive impairment in parkinson’ s disease: a systematic review and meta-analysis. Front Neurol. 2020;11:597955. [13] BEGEMANN MJ, BRAND BA, ĆURČIĆ-BLAKE B, et al. Efficacy of non-invasive brain stimulation on cognitive functioning in brain disorders: a meta-analysis. Psychol Med. 2020;50(15):2465-2486. [14] 黄木兰,王丽萍,胡柯嘉,等.非侵入式脑刺激对帕金森病患者执行功能的影响:网状meta分析[J].海军军医大学学报, 2024,45(5):584-591. [15] STERNE JAC, SAVOVIĆ J, PAGE MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:I4898. [16] 刘津池,刘畅,华成舸.随机对照试验偏倚风险评价工具RoB2(2019修订版)解读[J].中国循证医学杂志,2021,21(6): 737-744. [17] 王琪,王建成,潘蓓,等.网状Meta分析证据质量分级:GRADE方法学前沿与进展[J].中国循证医学杂志,2020,20(8):979-985. [18] BIUNDO R, WEIS L, FIORENZATO E, et al. Double-blind randomized trial of t-DCS versus sham in Parkinson patients with mild cognitive impairment receiving cognitive training. Brain Stimul. 2015;8(6):1223-1225. [19] HE W, WANG JC, TSAI PY. Theta burst magnetic stimulation improves parkinson’s-related cognitive impairment: a randomised controlled study. Neurorehabil Neural Repair. 2021;35(11):986-995. [20] KHEDR EM, MOHAMED KO, ALI AM, et al. The effect of repetitive transcranial magnetic stimulation on cognitive impairment in Parkinson’s disease with dementia: Pilot study. Restor Neurol Neurosci. 2020;38(1):55-66. [21] LANG S, GAN L S, YOON E J, et al. Theta-burst stimulation for cognitive enhancement in Parkinson’s disease with mild cognitive impairment: a randomized, double-blind, sham-controlled trial. Front Neurol. 2020; 11:584374. [22] LAWRENCE BJ, GASSON N, JOHNSON AR, et al. Cognitive training and transcranial direct current stimulation for mild cognitive impairment in Parkinson’s disease: a randomized controlled trial. Parkinsons Dis. 2018;4318475. [23] MANENTI R, BRAMBILLA M, BENUSSI A, et al. Mild cognitive impairment in Parkinson’s disease is improved by transcranial direct current stimulation combined with physical therapy. Mov Disord. 2016;31(5):715‐724. [24] MANENTI R, COTELLI MS, COBELLI C, et al. Transcranial direct current stimulation combined with cognitive training for the treatment of Parkinson Disease: a randomized, placebo-controlled study. Brain Stimul. 2018;11(6):1251-1262. [25] SIMONETTA C, BISSACCO J, CONTI M, et al. Motor cortex transcranial direct current stimulation improves non-motor symptoms in early-onset Parkinson’s disease: a pilot study. J Neural Transm (Vienna). 2024; 131(2):189‐193. [26] ZHUANG S, WANG FY, GU X, et al. Low-frequency repetitive transcranial magnetic stimulation over right dorsolateral prefrontal cortex in Parkinson’s disease. Parkinson’s Dis. 2020;7295414. [27] BUARD I, SCIACCA DM, MARTIN CS, et al. Transcranial magnetic stimulation does not improve mild cognitive impairment in Parkinson’s disease. Mov Disord. 2018; 33(3):489-491. [28] CHANG WH, KIM MS, PARK E, et al. Effect of dual-mode and dual-site noninvasive brain stimulation on freezing of gait in patients with Parkinson disease. Arch Phys Med Rehabil. 2017;98(7):1283-1290. [29] KIMURA H, KURIMURA M, KUROKAWA K, et al. A comprehensive study of repetitive transcranial magnetic stimulation in Parkinson’s disease. ISRN Neurol. 2011; 2011:845453. [30] PAL E, NAGY F, ASCHERMANN Z, et al. The impact of left prefrontal repetitive transcranial magnetic stimulation on depression in Parkinson’s disease: a randomized, double-blind, placebo-controlled study. Mov Disord. 2010;25(14): 2311-2317. [31] AFTANAS LI, BRACK IV, KULIKOVA KI, et al. Clinical and neurophysiological effects of the therapeutic combination of high-frequency rhythmic transcranial magnetic stimulation of the motor and frontal cortex in Parkinson’s disease. Neurosci Behav Physiol. 2021;51(2):135-141. [32] Spagnolo F, Fichera M, Chieffo R, et al. Bilateral repetitive transcranial magnetic stimulation with the h-coil in Parkinson’s disease: a randomized, sham-controlled study. Front Neurol. 2021;11:584713. [33] 郑秀琴,于苏文,何益民,等.高频重复经颅磁刺激对帕金森病患者临床症状及其细胞衰老相关因子的影响[J].中华物理医学与康复杂志,2022,44(5):427-432. [34] 蔡庆节,徐鹏飞,邹涛,等.高频重复经颅磁刺激对伴抑郁的帕金森病患者情绪及认知功能的影响[J].癫痫与神经电生理学杂志,2019,28(6):331-335. [35] 高巧林,梁佳佳,王娜,等.高频重复经颅磁刺激治疗对早期帕金森病患者轻度认知功能障碍的临床疗效观察[J].贵州医药,2022,46(7):1048-1049. [36] 郭芬.高频重复经颅磁刺激在帕金森病患者中的应用效果观察[J].医药论坛杂志,2020,41(4):98-101. [37] 洪东好,祝善尧,陈海燕,等.康复运动训练联合经颅直流电刺激对帕金森病患者步行功能、平衡功能和认知功能的影响[J].现代生物医学进展,2022, 22(13):2575-2578. [38] 胡喜莲,薛翠萍,刘自双.经颅直流电刺激辅助功能康复训练对帕金森病患者康复的效果[J].中国老年学杂志,2021, 41(17):3724-3727. [39] 胡晓颖,雷鸿雁,张彤,等.rTMS刺激双侧前额叶背外侧治疗帕金森病患者临床观察[J].中国实用神经疾病杂志,2023, 26(4):443-447. [40] 黄荣,李晓晖,陈文武.重复经颅磁刺激联合帕罗西汀对帕金森合并抑郁患者认知、情绪及血清清 5-HT、IL-1β 水平的影响[J].国际精神病学杂志,2023,50(3): 466-468, 472. [41] 李学,张俊红,祁亚伟,等.经颅直流电刺激对早期未治疗帕金森病患者认知功能及听觉事件相关电位的影响[J].中华物理医学与康复杂志,2018,40(3):198-201. [42] 李煜,郭艳红,杨丽娟.重复经颅磁刺激改善帕金森病患者认知对步态的影响[J].世界中医药,2019,14(12):3389-3393. [43] 缪礁丹,张玉勋,唐卉,等.高-低频交互rTMS对中期帕金森病患者SCOPA-AUT评分认知功能及运动功能的影响[J].中国实用神经疾病杂志,2023,26(11):1326-1330. [44] 苏敏,韩立影,刘传道,等.重复经颅磁刺激对帕金森病非运动症状康复疗效的研究[J].中华物理医学与康复杂志,2012, 34(12):911-915. [45] 孙莉,王舒,叶维,等.经颅直流电刺激联合计算机辅助认知康复训练改善帕金森病认知障碍的临床疗效观察[J].中国康复,2020,35(6):308-311. [46] 王超,牛德旺,吴文波,等.经颅直流电刺激联合个性化康复教育应用于帕金森病患者情绪、认知功能和步态的影响[J].国际精神病学杂志,2022,49(5):904-907. [47] 王广君,赵振华,吴东川,等.经颅直流电刺激对帕金森病非运动症状的疗效[J].中国医药导报,2016,13(5):75-78. [48] 王磊,黄廷,张真.鼠神经生长因子联合rTMS治疗帕金森病的疗效观察[J].分子诊断与治疗杂志,2023,15(11):1913-1916, 1920. [49] HE W, FONG PY, LEUNG TWH, et al. Protocols of non-invasive brain stimulation for neuroplasticity induction. Neurosci Lett. 2020;719:133437. [50] MOSILHY EA, ALSHIAL EE, ELTARAS MM, et al. Non-invasive transcranial brain modulation for neurological disorders treatment: a narrative review. Life Sci. 2022; 307:120869. [51] MORETTI J, RODGER J. Working toward an integrated plasticity/network framework for repetitive transcranial magnetic stimulation to inform tailored treatments. Neural Regen Res. 2024;19(7):1423-1424. [52] YANG Y, YAN Z, CHANG W, et al. Effect of different modalities of transcranial magnetic stimulation on Parkinson’s patients cognitive impairment and long-term effectiveness: a systematic review and network meta-analysis. Front Neurosci. 2024;18:1354864. [53] DE SOUZA SOUTO JJ, EDITE CASÉ DE OLIVEIRA M, SILVA GM, et al. Transcranial direct current stimulation and cognitive changes in Parkinson’s disease, a systematic review with meta-analysis and meta-regression. Appl Neuropsychol Adult. 2024. doi: 10.1080/23279095.2024.2367108. [54] JIANG Y, GUO Z, MCCLURE MA, et al. Effect of rTMS on Parkinson’s cognitive function: a systematic review and meta-analysis. BMC Neurol. 2020;20(1):377. [55] ZHANG W, DENG B, XIE F, et al. Efficacy of repetitive transcranial magnetic stimulation in Parkinson’s disease: a systematic review and meta-analysis of randomised controlled trials. EClinicalMedicine. 2022;52:101589. [56] AARSLAND D, BATZU L, HALLIDAY GM, et al. Parkinson disease-associated cognitive impairment. Nat Rev Dis Primers. 2021; 7(1):47. [57] LI X, QI G, YU C, et al. Cortical plasticity is correlated with cognitive improvement in Alzheimer’s disease patients after rTMS treatment. Brain Stimul. 2021;14(3):503-510. [58] TRUNG J, HANGANU A, JOBERT S, et al. Transcranial magnetic stimulation improves cognition over time in Parkinson’ s disease. Parkinsonism Relat Disord. 2019;66:3-8. [59] 熊莉君,杨燕,王芳.重复经颅磁刺激联合心理干预治疗帕金森病抑郁患者的疗效观察[J].中华物理医学与康复杂志, 2023,45(4):312-316. [60] MCGREGOR MM, NELSON AB. Circuit mechanisms of Parkinson’s disease. Neuron. 2019;101(6):1042-1056. [61] SHEN L, HUANG Y, LIAO Y, et al. Effect of high-frequency repetitive transcranial magnetic stimulation over M1 for consciousness recovery after traumatic brain injury. Brain Behav. 2023;13(5):2971. [62] LIU X, LIU H, LIU Z, et al. Transcranial direct current stimulation for Parkinson’s disease: a systematic review and meta-analysis. Front Aging Neurosci. 2021;13:746797. [63] BINDMAN LJ, LIPPOLD OC, REDFEARN JW. The action of brief polarizing currents on the cerebral cortex of the rat (1) during current flow and (2) in the production of long-lasting after-effects. J Physiol. 1964; 172(3):369-382. [64] JONES DT, GRAFF-RADFORD J. Executive dysfunction and the prefrontal cortex. Continuum (Minneap Minn). 2021;27(6): 1586-1601. [65] CONCA A, PESCHINA W, KÖNIG P, et al. Effect of chronic repetitive transcranial magnetic stimulation on regional cerebral blood flow and regional cerebral glucose uptake in drug treatment-resistant depressives. A brief report. Neuropsychobiology. 2002;45(1): 27-31. [66] HE PK, WANG LM, CHEN JN, et al. Repetitive transcranial magnetic stimulation (rTMS) fails to improve cognition in patients with parkinson’s disease: a Meta-analysis of randomized controlled trials. Int J Neurosci. 2022;132(3):269-282. [67] PALMA JA, THIJS RD. Non-pharmacological treatment of autonomic dysfunction in Parkinson’s disease and other synucleinopathies. J Parkinsons Dis. 2024; 14(1):81-92. [68] LIU X, LI L, LIU Y. Comparative motor effectiveness of non-invasive brain stimulation techniques in patients with Parkinson’s disease: a network meta-analysis. Medicine. 2023;102(39):e34960. |
| [1] | Yang Yuanyuan, Zhou Shanshan, Cheng Xiaofei, Feng Luye, Tang Jiqin. Network meta-analysis of non-invasive brain stimulation in the treatment of lower limb motor dysfunction after stroke [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1008-1018. |
| [2] | Zhang Yuxin, Yu Cong, Zhang Cui, Ding Jianjun, Chen Yan. Differences in postural control ability between older adults with mild cognitive impairment and those with normal cognition under different single-task and dual-task conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1643-1649. |
| [3] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [4] | Wang Zhifeng, Yang Jiao, Xi Yujiang, Xu Shuangfeng, Shi Ting, Lan Junfeng, Hao Zhihui, He Pengfen, Yang Aiming, Pan Pan, Wang Jian. Biomarkers affecting the progression of mild to moderate cognitive impairment after stroke: #br# a non-targeted metabolomics analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5116-5126. |
| [5] | Hu Tong, Li Xuan, Yuan Jing, Wang Wei. Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5224-5236. |
| [6] | Wang Jingying, , Ren Binbin, Ma Suna, Yang Yueyue, , Wu Song, , Guan Mengya, . Mechanism of alpha-synuclein in mitochondrial damage induced by Parkinson’s disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3668-3674. |
| [7] | Dong Zhiwen, Yu Cong, Chen Yan, Ding Jianjun . Central nervous mechanisms underlying effects of cognitive impairment on dual-task stance: #br# functional near-infrared spectroscopy analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3579-3587. |
| [8] | Qian Lei, Yu Hongli, Zhao Xiuzhi, Zhu Yucan. Effect of transcranial magnetic stimulation on potassium channels in the dentate gyrus of the hippocampus of Alzheimer’s disease mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2544-2552. |
| [9] | Yan Jie, Zhou Jing, Zhao Jingpu, Zhang Qingfang, Zhou Mingchao, Wang Yulong. Visual analysis of high-definition transcranial direct current stimulation research [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5110-5115. |
| [10] | Lin Qinzhao, Wei Mengli, Zhong Yaping, Wu Qian, Zhou Botao, Wang Haifeng. Effect of transcranial direct current stimulation on human single-leg landing stability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(26): 4209-4215. |
| [11] | Qi Liuxin, Zhou Mian, Wang Xiangyu, Sun Wei, Wang Jiangna. Effect of support surface stability on balance in the elderly with mild cognitive impairment under different visual input conditions [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3897-3902. |
| [12] | Shi Jiao, Li Xingjie, Liu Qiqi, Liu Jun, Yuan Xu, Chen Shangjie. Effect of electronic moxibustion on the volume of hippocampal subregion in patients with amnestic mild cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(20): 3176-3181. |
| [13] | Deng Longfei, Zhang Yeting, Fu Yan. Aerobic exercise inhibits neuroinflammation and alleviates cognitive impairment in Alzheimer’s disease model mice [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2209-2214. |
| [14] | Yang Yulin, Chang Wanpeng, Ding Jiangtao, Xu Hongli, Wu Xiao, Xiao Boheng, Ma Lihong. Transcranial direct current stimulation at different targets for Parkinson’s disease: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(11): 1797-1804. |
| [15] | Jiang Xuemin, Wang Yu, Sun Yanlin. Transcranial direct current stimulation of the dorsolateral prefrontal cortex improves attentional bias in mobile phone addicts [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(23): 3736-3741. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||