Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (2): 322-330.doi: 10.12307/2025.206
Previous Articles Next Articles
Causal relationship between sedentary and physical activity levels in the Oswestry disability index score and intervertebral disc degeneration
Huang Renjun1, Yang Jingyan1, Ma She1, Wang Chaoyi1, Zhao Yuyang1, Yu Dong2
- 1The Third Clinical School of Beijing University of Chinese Medicine, Beijing 100029, China; 2Department of Spine, The Third Clinical Hospital of Beijing University of Chinese Medicine, Beijing 100029, China
-
Received:2024-01-02Accepted:2024-01-29Online:2025-01-18Published:2024-05-24 -
Contact:Yu Dong, MD, Chief physician, Master’s supervisor, Department of Spine, The Third Clinical Hospital of Beijing University of Chinese Medicine, Beijing 100029, China -
About author:Huang Renjun, Master candidate, The Third Clinical School of Beijing University of Chinese Medicine, Beijing 100029, China -
Supported by:2022 Cultivation Project of the Ministry of Education Engineering Research Center, The Third Affiliated Hospital of Beijing University of Chinese Medicine, Beijing, No. BZYSY-2022-GCYJZXQX-08 (to YD)
CLC Number:
Cite this article
Huang Renjun, Yang Jingyan, Ma She, Wang Chaoyi, Zhao Yuyang, Yu Dong. Causal relationship between sedentary and physical activity levels in the Oswestry disability index score and intervertebral disc degeneration[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 322-330.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
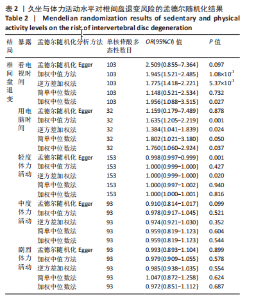
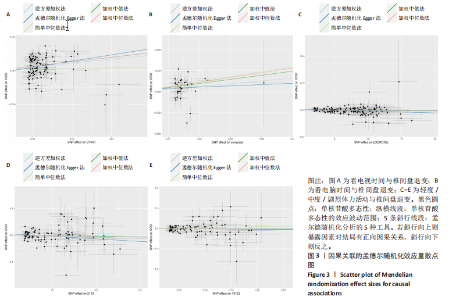
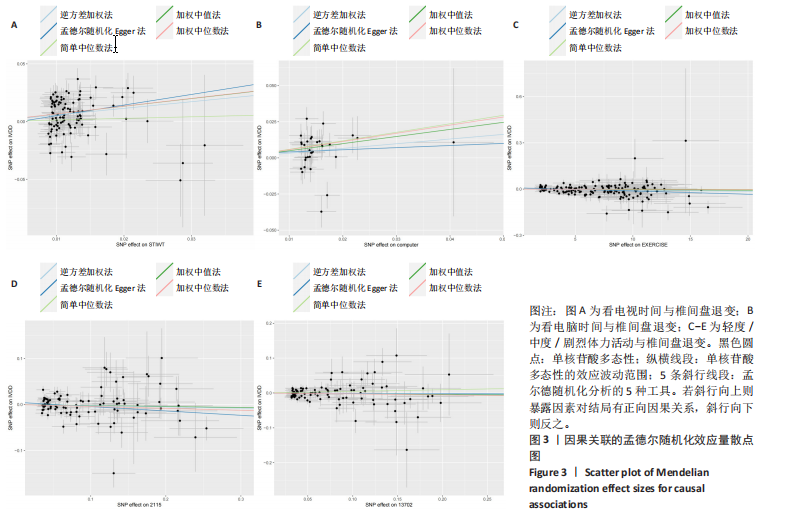
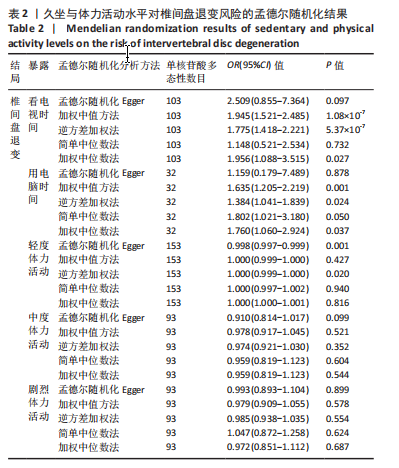
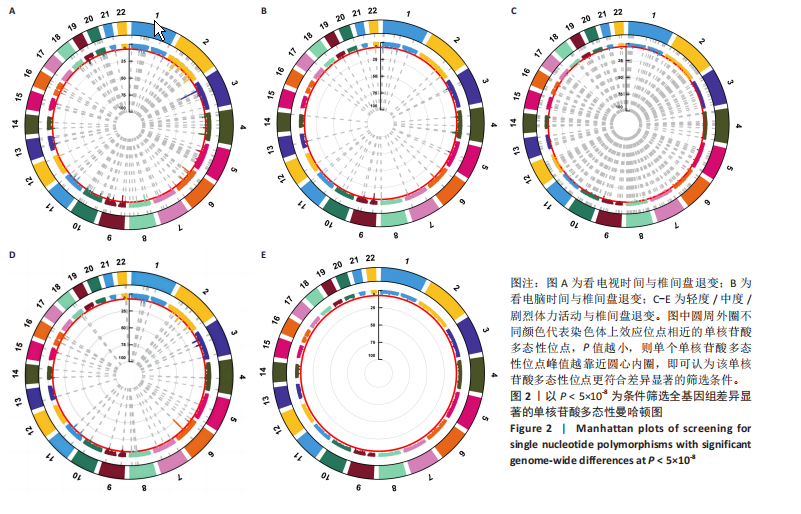
2.1 工具变量的选取 按照此次研究的工具变量的筛选条件,2个久坐行为表型(看电视/用电脑的时间)、3个体力活动水平表型(轻度/中度/剧烈体力活动)的工具变量被纳入研究,所有工具变量的F值均> 10,表明此次研究中工具变量进行因果效应的估计可靠性较高。 2.2 久坐行为与椎间盘退变的因果关系 在久坐行为(看电视/用电脑的时间)与椎间盘退变的关联研究中,首先从看电视/用电脑的时间GWAS中分别提取112/36个显著相关水平(P < 5×10-8)并去除连锁不平衡(r2 < 0.001,10 000 kb)的SNP,从Pheno Scanner数据库检索相关的表型,分别剔除其对应表型与椎间盘退变具有相关意义的9/4个SNP,即(rs472913、rs883027、rs9326862、rs4711634、rs17568389、rs12553324、rs184332798、rs111901094、rs6125907)/(rs2652429、rs76824303、rs36083903、rs7281293),MR-PRESSO分析无离群值,SNP的F统计量分别为(16.60-83.84)/(18.28-45.22)。最终分别纳入103/32个SNP进行久坐行为(看电视/用电脑的时间)与椎间盘退变的MR分析。总效应值的方向一致,呈正相关,散点图回归线无明显偏移,见图3。5种方法的统计学结果显著。看电视的时间:逆方差加权法为OR=1.775,95%CI:1.418-2.221,P=5.37×10-7;用电脑的时间:逆方差加权法为OR=1.384,95%CI:1.041-1.839,P=0.024。结果表明久坐行为(看电视/用电脑的时间)是椎间盘退变发病的风险因素。随着看电视/用电脑的时间增加椎间盘退变的发病风险随之增加。 2.3 体力活动水平与椎间盘退变的因果关系 在体力活动水平(轻度/中度/剧烈体力活动)与椎间盘退变的关联研究中,首先从轻度/中度/剧烈体力活动GWAS中分别提取159/95/96个显著相关水平(P < 5×10-8)并去除连锁不平衡(r2 < 0.001,10 000 kb)的SNP,从PhenoScanner数据库检索相关的表型,分别剔除其对应表型与椎间盘退变具有相关意义的6/2/3个SNP,即(rs5719937、rs191830420、rs74379084、rs10867028、rs624452、rs117908644)/(rs35211652、rs190615711)/(rs55771812、rs113206446、rs4688885)。MR-PRESSO分析无离群值,SNP的F统计量分别为(39.80-83.20)/(39.80-83.20)/(31.69-54.43)。最终分别纳入153/93/93个SNP进行体力活动水平(轻度/中度/剧烈体力活动)与椎间盘退变的MR分析,发现在轻度体力活动与椎间盘退变关系中MR Egger法和逆方差加权法的统计学结果显著,加权中值法、简单中位数法、加权中位数法结果无统计学意义,但总效应值的方向一致,呈负相关,散点图回归线无明显偏移,见图3。逆方差加权法为OR=1.000,95%CI:0.999-1.000,P=0.020。结果表明,轻度体力活动可能是椎间盘退变发病的保护因素。随着轻度体力活动持续时间减少,椎间盘退变的发病风险随之增加,其他详细数据见表2。"
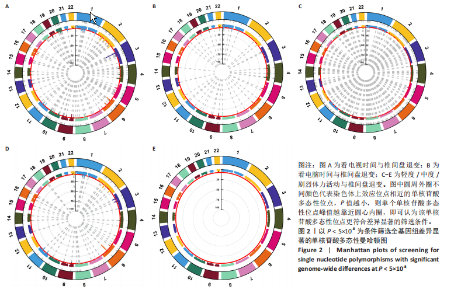
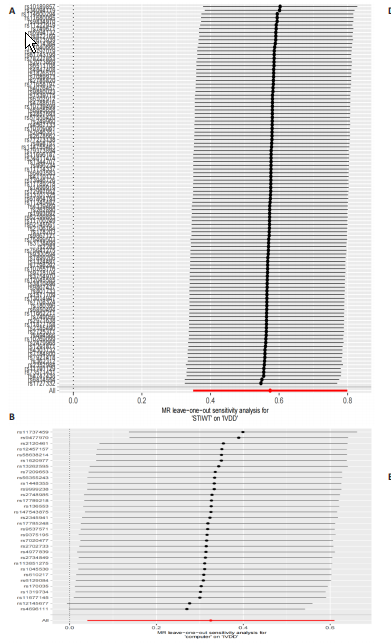
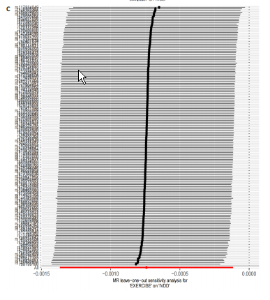
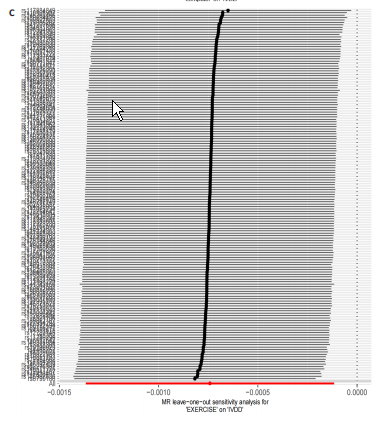
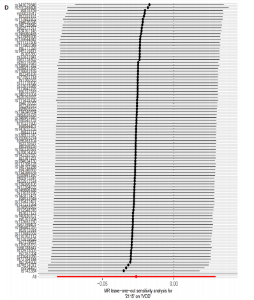
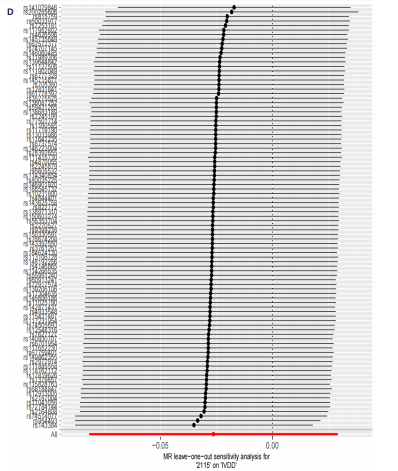
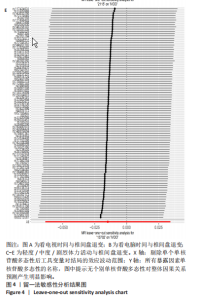
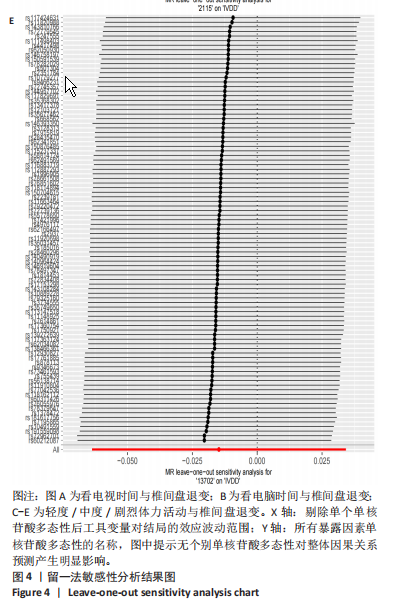
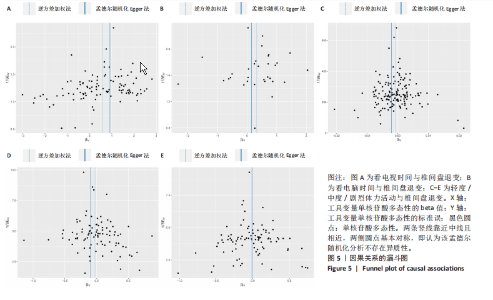
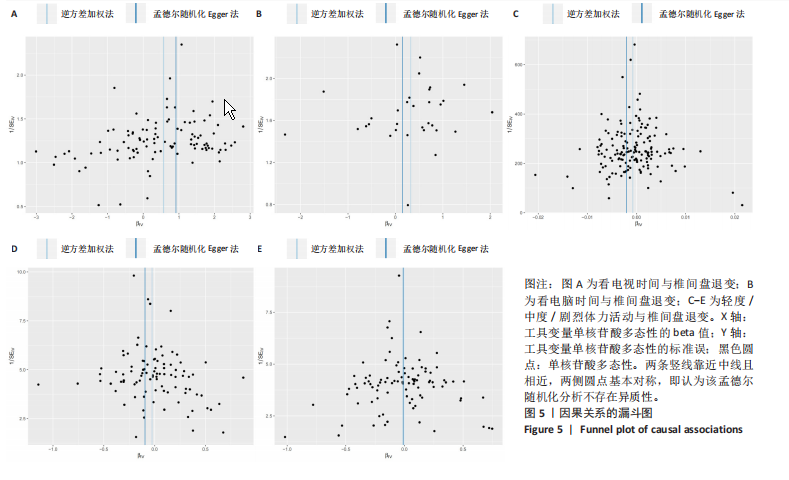
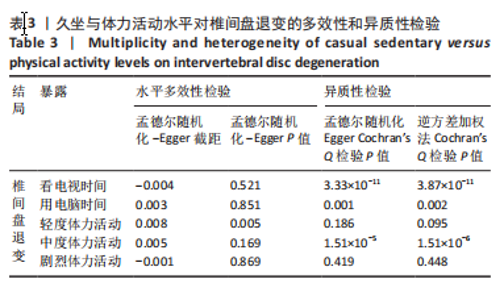
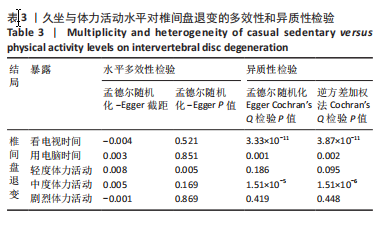
2.4 敏感性分析 MR-Egger截距分析中[P(轻度体力活动-椎间盘退变)=0.005],存在潜在的水平多效性,说明SNP可能通过轻度体力活动以外的途径影响结局;在Cochran’s Q异质性检验中,[P(看电视的时间-椎间盘退变)]=3.33×10-11 < 0.05,[P(用电脑的时间-椎间盘退变)=0.001 < 0.05,表明数据存在异质性,见表3。尽管检测到异质性,可能与样本量、分析方法和数据库有关,但逆方差加权分析结果表明,看电视/用电脑的时间与椎间盘退变存在因果关系,满足独立性假设,且符合水平多效性检验,故允许异质性存在,不影响阳性结果的解读。留一法分析表明,因果关系不是由某个SNP驱动,见图4。漏斗图分布基本对称,未见明显偏倚,见图5。 "
| [1] BHUJEL B, SHIN HE, CHOI DJ, et al. Mesenchymal Stem Cell-Derived Exosomes and Intervertebral Disc Regeneration: Review. Int J Mol Sci. 2022;23(13):7306. [2] SCARCIA L, PILEGGI M, CAMILLI A, et al. Degenerative Disc Disease of the Spine: From Anatomy to Pathophysiology and Radiological Appearance, with Morphological and Functional Considerations. J Pers Med. 2022;12(11):1810. [3] TERAGUCHI M, YOSHIMURA N, HASHIZUME H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthritis Cartilage. 2014;22(1):104-110. [4] WEGNER M, BACKHAUß JC, MICHALSKY Y, et al. Prevalence of degenerative vertebral disc changes in elite female Crossfit athletes - a cross-sectional study. BMC Musculoskelet Disord. 2023;24(1):963. [5] XU J, SHAO T, LOU J, et al. Aging, cell senescence, the pathogenesis and targeted therapies of intervertebral disc degeneration. Front Pharmacol. 2023;14:1172920. [6] SONG C, ZHOU Y, CHENG K, et al. Cellular senescence - Molecular mechanisms of intervertebral disc degeneration from an immune perspective. Biomed Pharmacother. 2023;162:114711. [7] TREMBLAY MS, AUBERT S, BARNES JD, et al. Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. [8] HANNA F, DAAS RN, EL-SHAREIF TJ, et al. The Relationship Between Sedentary Behavior, Back Pain, and Psychosocial Correlates Among University Employees. Front Public Health. 2019;7:80. [9] TEICHTAHL AJ, URQUHART DM, WANG Y, et al. Physical inactivity is associated with narrower lumbar intervertebral discs, high fat content of paraspinal muscles and low back pain and disability. Arthritis Res Ther. 2015;17(1):114. [10] MENDES MA, DA SILVA I, RAMIRES V, et al. Metabolic equivalent of task (METs) thresholds as an indicator of physical activity intensity. PLoS One. 2018;13(7):e0200701. [11] KIM D, LEE J, PARK HK, et al. Comparing the standards of one metabolic equivalent of task in accurately estimating physical activity energy expenditure based on acceleration. J Sports Sci. 2017;35(13):1279-1286. [12] LYONS FL, MARTIN GINIS KA. Multidimensionality of leisure-time physical activity behaviour in adults with spinal cord injury: implications for measurement. Spinal Cord. 2023. doi: 10.1038/s41393-023-00947-6. [13] VIEIRA LA, DOS SANTOS AA, PELUSO C, et al. Influence of lifestyle characteristics and VDR polymorphisms as risk factors for intervertebral disc degeneration: a case-control study. Eur J Med Res. 2018;23(1):11. [14] BOWDEN JA, BOWDEN AE, WANG H, et al. In vivo correlates between daily physical activity and intervertebral disc health. J Orthop Res. 2018;36(5):1313-1323. [15] BOWDEN J, HOLMES MV. Meta-analysis and Mendelian randomization: A review. Res Synth Methods. 2019;10(4):486-496. [16] RICHMOND RC, DAVEY SMITH G. Mendelian Randomization: Concepts and Scope. Cold Spring Harb Perspect Med. 2022;12(1):a040501. [17] DAVEY SMITH G, HEMANI G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89-98. [18] HARTWIG FP, BORGES MC, HORTA BL, et al. Inflammatory Biomarkers and Risk of Schizophrenia: A 2-Sample Mendelian Randomization Study. JAMA Psychiatry. 2017;74(12):1226-1233. [19] SKRIVANKOVA VW, RICHMOND RC, WOOLF BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. JAMA. 2021; 326(16):1614-1621. [20] BURGESS S. Violation of the Constant Genetic Effect Assumption Can Result in Biased Estimates for Non-Linear Mendelian Randomization. Hum Hered. 2023;88(1):79-90. [21] KARAGEORGIOU V, TYRRELL J, MCKINLEY TJ, et al. Weak and pleiotropy robust sex-stratified Mendelian randomization in the one sample and two sample settings. Genet Epidemiol. 2023 Mar;47(2):135-151. [22] HAN Y, ZHANG Y, ZENG X. Assessment of causal associations between uric acid and 25-hydroxyvitamin D levels. Front Endocrinol (Lausanne). 2022;13:1024675. [23] BOWDEN J, DAVEY SMITH G, HAYCOCK PC, et al. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 2016;40(4):304-314. [24] DOBRIJEVIC E, VAN ZWIETEN A, KIRYLUK K, et al. Mendelian randomization for nephrologists. Kidney Int. 2023;104(6):1113-1123. [25] VERBANCK M, CHEN CY, NEALE B, et al. Publisher Correction: Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(8):1196. [26] BURGESS S, THOMPSON SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017; 32(5):377-389. [27] ALJOHANI AA, ALARAWI SM, ALHUSAYNI YM, et al. Prevalence of Low Back Pain Among University Attendants in Tabuk City During 2023: A Cross-Sectional Study in Saudi Arabia. Cureus. 2023;15(12):e50357. [28] BAKLOUTI M, BEN AYED H, KETATA N, et al. Low back-pain among school-teachers in Southern Tunisia: prevalence and predictors. Scand J Pain. 2023;23(4):687-693. [29] BOOTH FW, ROBERTS CK, LAYE MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143-1211. [30] AUBRY C, NÜESCH C, FIEBIG O, et al. Accelerometry-based physical activity, disability and quality of life before and after lumbar decompression surgery from a physiotherapeutic perspective: An observational cohort study. N Am Spine Soc J. 2021;8:100087. [31] KANAYAMA M, TOGAWA D, TAKAHASHI C, et al. Cross-sectional magnetic resonance imaging study of lumbar disc degeneration in 200 healthy individuals. J Neurosurg Spine. 2009;11(4):501-507. [32] BALLING M, HOLMBERG T, PETERSEN CB, et al. Total sitting time, leisure time physical activity and risk of hospitalization due to low back pain: The Danish Health Examination Survey cohort 2007-2008. Scand J Public Health. 2019;47(1):45-52. [33] FRYDENLUND G, JØRGENSEN T, TOFT U, et al. Sedentary leisure time behavior, snacking habits and cardiovascular biomarkers: the Inter99 Study. Eur J Prev Cardiol. 2012;19(5):1111-1119. [34] BLÜHER M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288-298. [35] OTTEN JJ, JONES KE, LITTENBERG B, et al. Effects of television viewing reduction on energy intake and expenditure in overweight and obese adults: a randomized controlled trial. Arch Intern Med. 2009;169(22):2109-2115. [36] AMBROSIO L, MAZZUCA G, MAGUOLO A, et al. The burden of low back pain in children and adolescents with overweight and obesity: from pathophysiology to prevention and treatment strategies. Ther Adv Musculoskelet Dis. 2023;15:1759720X231188831. [37] SAMARTZIS D, KARPPINEN J, CHAN D, et al. The association of lumbar intervertebral disc degeneration on magnetic resonance imaging with body mass index in overweight and obese adults: a population-based study. Arthritis Rheum. 2012;64(5):1488-1496. [38] HE Q, BENNETT AN, FAN B, et al. Assessment of Bidirectional Relationships between Leisure Sedentary Behaviors and Neuropsychiatric Disorders: A Two-Sample Mendelian Randomization Study. Genes (Basel). 2022;13(6):962. [39] PINHEIRO MB, FERREIRA ML, REFSHAUGE K, et al. Symptoms of Depression and Risk of New Episodes of Low Back Pain: A Systematic Review and Meta-Analysis. Arthritis Care Res (Hoboken). 2015;67(11):1591-1603. [40] DZAKPASU FQS, CARVER A, BRAKENRIDGE CJ, et al. Musculoskeletal pain and sedentary behaviour in occupational and non-occupational settings: a systematic review with meta-analysis. Int J Behav Nutr Phys Act. 2021;18(1):159. [41] ALEXANDER L, CHRISTENSEN SM, RICHARDSON L, et al. Nutrition and physical activity: An Obesity Medicine Association (OMA) Clinical Practice Statement 2022. Obes Pillars. 2022;1:100005. [42] VERBRUGGHE J, HANSEN D, DEMOULIN C, et al. High Intensity Training Is an Effective Modality to Improve Long-Term Disability and Exercise Capacity in Chronic Nonspecific Low Back Pain: A Randomized Controlled Trial. Int J Environ Res Public Health. 2021;18(20):10779. [43] 林承宇. 清宫正骨腰部练功法干预腰椎间盘突出症的临床研究及生物力学分析[D].北京:中国中医科学院,2023. [44] 杨超凡.腰背伸动作对腰椎间盘退变大鼠多裂肌的影响[D].郑州:河南中医药大学,2016. [45] HLAING SS, PUNTUMETAKUL R, KHINE EE, et al. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord. 2021;22(1):998. [46] ZHOU W, SHI Y, WANG H, et al. Exercise-induced FNDC5/irisin protects nucleus pulposus cells against senescence and apoptosis by activating autophagy. Exp Mol Med. 2022;54(7):1038-1048. [47] DA CRUZ FERNANDES IM, PINTO RZ, FERREIRA P, et al. Low back pain, obesity, and inflammatory markers: exercise as potential treatment. J Exerc Rehabil. 2018;14(2):168-174. [48] VAN DE VEGTE YJ, SAID MA, RIENSTRA M, et al. Genome-wide association studies and Mendelian randomization analyses for leisure sedentary behaviours. Nat Commun. 2020;11(1):1770. |
| [1] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei, Zhou Jiatan. Based on Mendelian randomization, the causal relationship between 1400 metabolites and sarcopenia and the correlation analysis of cardiovascular disease were investigated [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-11. |
| [2] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [3] | Dong Tingting, Chen Tianxin, Li Yan, Zhang Sheng, Zhang Lei. Causal relationship between modifiable factors and joint sports injuries [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1953-1962. |
| [4] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [5] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [6] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [7] |
Zhao Wensheng, Li Xiaolin, Peng Changhua, Deng Jia, Sheng Hao, Chen Hongwei, Zhang Chaoju, He Chuan.
Gut microbiota and osteoporotic fractures #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1296-1304.
|
| [8] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [9] | Li Jiatong, Jin Yue, Liu Runjia, Song Bowen, Zhu Xiaoqian, Li Nianhu . Association between thyroid function levels and phenotypes associated with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1312-1320. |
| [10] | Xiang Pan, Che Yanjun, Luo Zongping. Compressive stress induces degeneration of cartilaginous endplate cells through the SOST/Wnt/beta-catenin pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 951-957. |
| [11] | Ding Zhili, Huang Jie, Jiang Qiang, Li Tusheng, Liu Jiang, Ding Yu. Constructing rabbit intervertebral disc degeneration models by different methods under X-ray guidance: a comparative study [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 995-1002. |
| [12] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| [13] | Wang Xuepeng, , He Yong, . Effect of insulin-like growth factor family member levels on inflammatory arthritis: a FinnGen biobank-based analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7656-7662. |
| [14] | Wang Tao, Wang Shunpu, Min Youjiang, Wang Min, Li Le, Zhang Chen, Xiao Weiping. Causal relationship between gut microbiota and rheumatoid arthritis: data analysis in European populations based on GWAS data [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7663-7668. |
| [15] | Han Jie, Pan Chengzhen, Shang Yuzhi, Zhang Chi. Identification of immunodiagnostic biomarkers and drug screening for steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7690-7700. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||