Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (10): 2171-2177.doi: 10.12307/2025.254
Previous Articles Next Articles
Manufacture and mechanical property on zirconia abutments with a titanium base in dental implant restoration
Wang Huan, Lu Jing, Li Ying, Meng Maohua, Shu Jiayu, Luo Yuncai, Li Wenjie, Dong Qiang
- School of Stomatology, Guizhou Medical University/Affiliated Stomatological Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China
-
Received:2023-12-11Accepted:2024-02-04Online:2025-04-08Published:2024-08-26 -
Contact:Dong Qiang, MD, Chief physician, Doctoral supervisor, School of Stomatology, Guizhou Medical University/Affiliated Stomatological Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
About author:Wang Huan, Master candidate, School of Stomatology, Guizhou Medical University/Affiliated Stomatological Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China
CLC Number:
Cite this article
Wang Huan, Lu Jing, Li Ying, Meng Maohua, Shu Jiayu, Luo Yuncai, Li Wenjie, Dong Qiang. Manufacture and mechanical property on zirconia abutments with a titanium base in dental implant restoration[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(10): 2171-2177.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
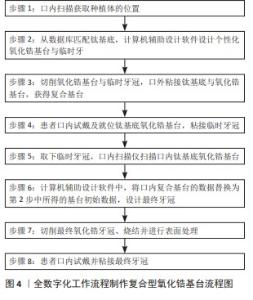
2.1 钛基底氧化锆基台的印模与制作 2.1.1 钛基底氧化锆基台的印模方法 随着数字化印模技术的发展,种植牙修复的数字化印模方法被普遍应用。DERKSEN等[17]研究表明,相较于传统的印模方法,通过口内扫描制作的钛基底氧化锆基台上的修复体在临床中调牙合时间更短、效率更高。在MANGANO等[18]和LERNERDE等[19]的回顾性研究中,全数字化工作流程制作的钛基底氧化锆基台的1年和3年成功率分别为92.4%和91.3%,全数字化工作流程制作复合型氧化锆基台似乎是一种可靠的治疗方案,该数字化工作流程共8个步骤,具体见图4。然而,该方案的有效性仍需要对更多患者进一步的研究和不同的修复体(如种植体支持的多单位桥)来证实。为了进一步比较数字化印模与传统印模上制作的钛基底氧化锆基台修复体的远期成功率,DERKSEN等[20]对50例患者和84个修复体完成了为期3年的随访,结果显示两种不同印模方式制作的修复体3年成功率没有统计学差异。钛基底氧化锆基台修复时存在2种不同的数字化印模方法,分别是直接安装扫描杆转移种植体位置到数字化修复软件中与直接用扫描仪获得钛基底相关数据信息。有研究对以上两种方法制作的基台及牙冠进行口腔种植单牙修复精度分析,结果显示直接安装扫描杆转移种植体位置到数字化修复软件中得到的基台相关数据信息更为精确可靠,加工制造的修复冠精密度更高和稳定性更好[21],可见在钛基底氧化锆基台修复制作工艺上,其全数字化的工作流程似乎是可靠的。然而,目前关于钛基底氧化锆基台数字化印模方式的研究有限,仍需要更多的高水平临床询证证据和生物力学研究进一步分析。 2.1.2 钛基底的选择和氧化锆基台的制作 钛基底氧化锆基台是通过计算机辅助设计与制造个性化氧化锆层,然后将其粘接到预制钛基底,既可以提供良好的美学效果又可避免在基台连接处存在氧化锆,兼具钛的强度与氧化锆基台良好的美学效果[7,22]。目前,几种常用计算机辅助设计与制作系统包括Cerec系统、Lava系统、Everest系统、Wieland系统和Procera系统[23]。预制的钛基底包括由种植体制造商制作的原厂钛基底和第三方厂家制作的钛基底。研究表明,由第三方厂家制作的钛基底与种植体连接处会存在更大的微间隙,产生不利的应力集中[24-25]。ASGEIRSSON等[26]和STUCKI等[27]对氧化锆基台使用非原厂钛基底1年和3年的随访观察得到同样的结果,使用非原厂钛基底与探诊出血指数、探诊深度及牙槽骨吸收显著增加密切相关,因此,临床中不推荐氧化锆基台使用非原厂钛基底。针对其上部结构氧化锆基台制作的体外实验研究证明,由原厂制作和第三方加工厂制作的氧化锆基台与钛基底的边缘和内部密合度方面无统计学差异,两者均可达到高度密合[28]。综上所述,建议尽量选择种植体制造商制作的钛基底用于钛基底氧化锆基台,其上部结构氧化锆基台部分则可以选择原厂或第三方加工厂制作。"

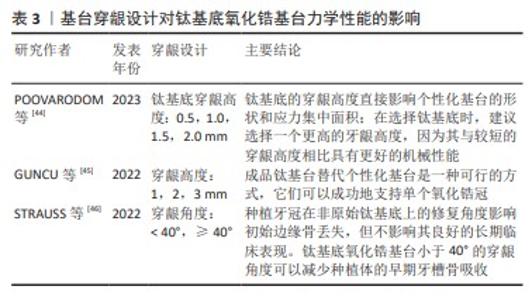
2.2 钛基底氧化锆基台的力学性能 2.2.1 种植体-基台连接方式对钛基底氧化锆基台力学性能的影响 研究表明,种植体-基台连接方式是种植体周围炎发生发展的重要影响因素[29],对中央螺丝的稳定性和基台力学性能也有影响[30-31]。传统上,将基台连接分为外部连接或内部连接[32]。内连接可以根据基台与种植体内部的关系进一步分类,如间隙配合连接、内锥形连接和组合连接,其中又可以根据基台连接部分的几何特征分为抗旋和非抗旋连接[33]。 相较于外连接的钛基底氧化锆基台,具有内连接结构的种植体基台连接会更稳定[10],同样在防止微泄漏方面,内六边形尤其是具有莫氏锥度的内锥形连接种植体在静态加载和动态加载条件下都更具前景[34]。钛基底氧化锆基台的内锥形连接更有利于应力的分布,体外实验结果显示,内部柱形连接模型均出现中央螺丝折断,而内锥形连接模型的临界负荷值均接近正常咀嚼力大小[35]。然而,不同制造商的基台连接锥度也不相同,同一制造商也有不同锥度的内连接。研究认为,具有莫氏锥度的基台连接有利于减少中央螺丝松动的可能[36]。基于种植体基台连接设计对种植体修复的长期稳定性有重要的影响,各大种植厂家不断推出新的设计,例如:士卓曼品牌最新的BLX种植体系统,一个具有极限锁合的内连接设计,包括7°莫氏锥度及六面星形抗旋转结构。为了比较内连接类型对种植修复稳定性的影响,?AKMAK等[31]将极限锁合连接的基台与经典的具有15°内锥形连接的十字锁合钛基底氧化锆基台的稳定性进行对比,结果显示两种连接方式基台的初始扭矩值相似,然而在循环加载前后,十字锁合连接的种植体-基台连接具有更高的去扭矩值和更低的扭矩损失百分比;但是在循环加载过程中没有观察到螺丝松动,表明两种种植体-基台连接都很稳定。 在种植体和钛基底之间抗旋连接的结构可以减少预载荷损失和应力集中,这将降低种植体松动或失败相关的并发症的风险。在ADOLFI等[33]对抗旋和非抗旋钛基底氧化锆基台的边缘密合度、疲劳反应、应力集中的研究中,与非抗旋的钛基底氧化锆基台相比,具有抗旋结构的钛基底表现出更好的扭矩值维持,但两组间的扭矩值损失仅相差1.4 N·cm,根据基台设计的不同扭矩损失可高达到50.71%[37],因此这两种设计均在临床可接受范围,并且它们表现出相当的应力分布,均能承受前牙的最大咬合力,两种基台设计都可以被认为是前牙种植修复的可行选择。 因此,在使用钛基底氧化锆基台修复时,内连接具有更好的稳定性,外连接存在抗侧向力不足和中央螺丝易松动等缺点,但外连接的结构设计简单、直观,加工工艺简便,目前仍然在临床中应用。同时应该选择具有抗旋结构的基台连接或者是具有莫氏锥度的非抗旋连接,良好的莫氏锥度可以获得更大的摩擦力和冷焊接效果,可以根据患者的需求、种植体稳定性和其他临床因素综合考虑来选择。目前基台连接对钛基底氧化锆基台力学性能的影响相关研究进展,见表1。"

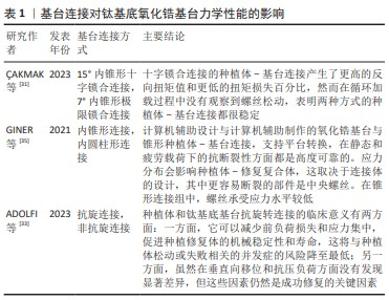
2.2.2 基台角度对钛基底氧化锆基台力学性能的影响 目前,钛基底氧化锆基台可能是上颌美学区的首选治疗方案,然而在上颌前牙区牙槽骨的一些解剖变化可能会限制种植体的轴向位置,此时便需要选择用带角度的钛基底氧化锆基台修复。一项有限元分析显示,与钛基台和氧化锆基台相比,钛基底氧化锆基台上的中央螺丝、基台、牙冠和种植体上的冯米塞斯应力均明显更低,使用17°基台分析模型比25°基台分析模型皮质骨和松质骨的应变值均更低[38]。KAPOOR等[39]研究得到同样的结果,在种植体周围骨中最大的应力出现在25°的基台,然后是15°基台和直基台,与钛基台相比,钛基底氧化锆直基台和成角基台修复的种植体对种植体周围骨转移的压力更小。 为了进一步探究角度钛基底氧化锆基台的角度范围,ZHANG等[40]用三维有限元的方法对上颌中切牙0°,15°,30°,-15°的钛基底氧化锆基台进行动态加载,以分析基台的应力分布以及种植体-基台连接处的微间隙,结果显示,当氧化锆基台角度从15°增加到30°时,中央螺丝、钛基底和周围骨组织的应力分别逐渐增加了9%,20%和23% ;30°氧化锆基台组的应力水平接近材料的屈服极限;然而当种植体长轴向腭侧倾斜时,-15°基台的应力降低3%,种植体应变水平降低17%,周围骨组织应变水平降低26%。另一项关于钛基底氧化锆基台的体外实验同样发现,未修复牙冠基台的失效载荷受到基台角度的影响,30°组67%的样品和-15°组83%的样品在氧化锆基台最薄弱部分断裂,即种植体-基台连接处出现断裂,粘接牙冠后基台的失效载荷接近或超过了前牙的最大咬合力[41]。 研究表明,氧化锆基台的成角角度对种植修复体的应力分布、微动大小和微间隙大小均有显著影响。种植体-基台界面的微动和微间隙是导致种植体周围牙槽骨吸收的重要原因[42],因此建议在上颌前牙区使用钛基底氧化锆基台时,种植体应放置在正确的轴向角度不超过15°或向腭侧倾斜;当唇部倾斜超过30°时,使用角度钛基底氧化锆基台就必须有效降低咬合力,以减少种植体折断的风险,并且建议使用具有更高推荐扭矩值的带角度的钛基底氧化锆基台[43]。目前基台连接对钛基底氧化锆基台力学性能的影响相关研究进展,见表2。"

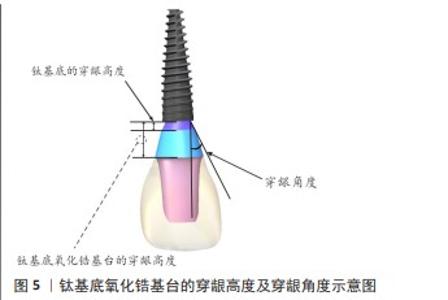
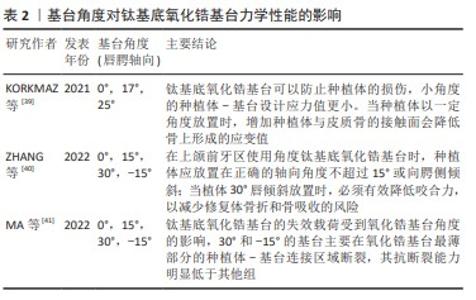
2.2.3 穿龈设计对钛基底氧化锆基台力学性能的影响 在不同的牙龈高度情况下均可以使用钛基底氧化锆基台修复种植体,然而钛基底的穿龈高度(图5)也会对基台的力学性能产生影响。目前临床中运用的钛基底的穿龈高度在0.5-2.0 mm之间,这取决于不同的种植体系统[44-45]。POOVARODOM等[44]研究表明,随着钛基底穿龈高度的增加,钛基底与氧化锆基台粘接界面随之远离应力集中区,钛基底氧化锆基台的应力值减小。穿龈高度较短的氧化锆基台出现较大的冯米塞斯应力和主应力,相反具有较高穿龈高度的钛基底氧化锆基台降低了个性化基台的断裂风险,而不增加其他任何机械并发症的风险。在探究穿龈高度对种植体周围骨吸收的影响中得到同样的结果,穿龈高度与种植体周围骨吸收呈反比,穿龈高度越高性能越好,穿龈高度大于2.5 mm的基台观察到较少的边缘骨丢失[36]。 除基台穿龈高度外,基台穿龈设计还需要考虑穿龈角度(图5)对种植修复体产生的影响。一项5年的临床随访研究显示,钛基底氧化锆基台的穿龈角度可能会影响修复初期牙槽骨的吸收,但不影响其良好的长期临床效果,小于40°的穿龈角度可以减少钛基底氧化锆基台修复初期的牙槽骨吸收[46]。穿龈角度与牙槽骨吸收之间的正相关关系可能与各种原因有关:首先,穿龈角度过大(> 40°)可能不利于卫生清洁[47];其次,种植体与基台界面可能存在微运动,种植体基台间形成的微间隙造成牙槽骨的吸收[48]。 "

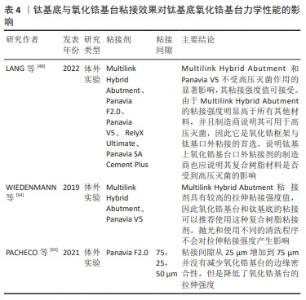
2.2.4 钛基底与氧化锆基台粘接效果对钛基底氧化锆基台力学性能的影响 氧化锆基台通过粘接与钛基底连接,它们的长期成功率在很大程度上取决于粘接的稳定性,因此氧化锆和钛基底之间可靠的粘接强度是临床成功的关键因素[49]。一项平均随访期达72.35个月的回顾性研究包含94例患者与325个种植修复体,其中氧化锆基台与钛基底间脱粘接的机械并发症发生率高达修复体总数的2.61%[50],可见提高两者间的粘接强度对减少此类并发症有重要意义。 研究表明,粘接剂的种类对氧化锆基台与钛基底间的粘接强度有显著影响[51–53]。最近的研究中,LANG等[49]对目前常用的复合树脂类粘接剂用于钛基底与氧化锆基台的粘接强度进行体外实验,所测粘接剂包括Multilink Hybrid Abutment、Panavia F2.0、Panavia V5、 RelyX Ultimate、以及Panavia SA Cement Plus,结果显示Multilink Hybrid Abutment比其他粘接剂的粘结强度都更强。WIEDENMANN等[54]的研究结果也显示,使用Multilink Hybrid Abutment粘接剂将氧化锆基台固定于钛基底,比运用Panavia V5具有更高的抗拉伸粘接强度。Multilink Hybrid Abutment制造商推荐其适用于钛基底与陶瓷材料的粘接,体外研究证明Multilink Hybrid Abutment粘接氧化锆基台与钛基底具有可靠的粘接强度,并且其粘接强度不受基台表面清洁处理(超声清洁、高压蒸汽灭菌、低压等离子处理等)的影响[54];此外,Multilink Hybrid Abutment是一种完全自固化的复合树脂黏合剂,可以避免大于一定厚度氧化锆显著降低光透射率而导致的光固化不全,因此建议Multilink Hybrid Abutment为氧化锆基台与钛基底口外粘接的首选粘接剂。除粘接剂的种类外,还应考虑钛基底与氧化锆基台间的粘接间隙差异产生的影响。PACHECO等[55]研究表明,钛基底与氧化锆基台间粘接间隙的增加并不影响两者间的边缘密合性,但75 μm粘接间隙的氧化锆基台拉伸强度均低于25 μm和50 μm实验组,提示大于75 μm的粘接间隙会降低氧化锆基台的拉伸强度,但目前的研究并不能给出两者间粘接间隙合适的范围值。 此外,钛基底和氧化锆基台的表面处理方式也会影响粘接效果。研究表明,用氧化铝颗粒进行钛基底和氧化锆基台表面的喷砂处理可以显著提高粘接效果,然而喷砂也可能造成氧化锆基台的微裂纹,进而影响其力学性能[52,56-57]。除表面进行喷砂处理外,有研究显示用含磷酸盐基的底漆进行表面化学改性同样可以提高钛基底和氧化锆基台间的粘接效果,然而表面机械预处理比化学改性更重要[52,56]。 综上所述,Multilink Hybrid Abutment可以作为氧化锆基台与钛基底口外粘结的首选粘接剂,钛基底与氧化锆基台的表面喷砂处理能提高两者间的粘接强度。目前钛基底与氧化锆基台粘接效果对Ti-base氧化锆基台力学性能影响的相关研究进展,见表4。"

| [1] HALIM FC, PESCE P, DE ANGELIS N, et al. Comparison of the Clinical Outcomes of Titanium and Zirconia Implant Abutments: A Systematic Review of Systematic Reviews. J Clin Med. 2022;11(17):5052. [2] VAZOURAS K, GHOLAMI H, MARGVELASHVILI-MALAMENT M, et al. An Esthetic Evaluation of Different Abutment Materials in the Anterior Maxilla: A Randomized Controlled Clinical Trial Using a Crossover Design. J Prosthodont. 2022;31(8):673-680. [3] LV X, PU Y, ZHANG X, et al. One-piece versus two-piece zirconia abutment supported single implant crown in the esthetic region: 3-Year results from a split-mouth randomized controlled clinical trial. Clin Oral Implants Res. 2023;34(12):1330-1341. [4] LOPES ACO, MACHADO CM, BONJARDIM LR, et al. The Effect of CAD/CAM Crown Material and Cement Type on Retention to Implant Abutments: CAD/CAM Crown Retentiveness on Ti-Base Abutments. J Prosthodont. 2019;28(2):e552-e556. [5] CÁRDENAS R, SÁNCHEZ D, EUÁN R, et al. Effect of fatigue loading and failure mode of different ceramic implant abutments. J Prosthet Dent. 2022;127(6):875-881. [6] PITTA J, HJERPPE J, BURKHARDT F, et al. Mechanical stability and technical outcomes of monolithic CAD/CAM fabricated abutment‐crowns supported by titanium bases: An in vitro study. Clin Oral Implants Res. 2021;32(2):222-232. [7] WATANABE H, FELLOWS C, AN H. Digital Technologies for Restorative Dentistry. Dent Clin North Am. 2022;66(4):567-590. [8] SAILER I, KARASAN D, TODOROVIC A, et al. Prosthetic failures in dental implant therapy. Periodontol 2000. 2022;88(1):130-144. [9] AFRASHTEHFAR KI, WEBER A, ABOU-AYASH S. Titanium-base abutments may have similar long-term peri-implant effects as non-bonded one-piece abutments. Evid Based Dent. 2022;23:134-135. [10] SAILER I, ASGEIRSSON AG, THOMA DS, et al. Fracture strength of zirconia implant abutments on narrow diameter implants with internal and external implant abutment connections: A study on the titanium resin base concept. Clin Oral Implants Res. 2018;29(4):411-423. [11] ZHAI Z, NAKANO T, CHEN Y, et al. Abutment removal torque and implant conical surface morphological changes after standardized artificial aging: An in vitro study. J Prosthet Dent. 2022:S0022-3913(22)00738-7. [12] POZZI A, ARCURI L, FABBRI G, et al. Long-term survival and success of zirconia screw-retained implant-supported prostheses for up to 12 years: A retrospective multicenter study. J Prosthet Dent. 2023;129(1): 96-108. [13] JUICA D, MARCUS N, GRANDON F, et al. Premature failure of a screw-retained ceramic single crown: A clinical report and fractographic analysis. J Prosthet Dent. 2022;127(1):32-37. [14] 方科达,丁鑫,周慧,等.CAD/CAM个性化瓷基台的体外力学性能研究[J].牙体牙髓牙周病学杂志,2017,27(1):22-27. [15] DERKSEN W, JODA T, CHANTLER J, et al. Group 2 ITI Consensus Report: Technological developments in implant prosthetics. Clin Oral Implants Res. 2023;34(S26):104-111. [16] WATANABE S, NAKANO T, ONO S, et al. Fracture Resistance of Zirconia Abutments with or without a Titanium Base: An In Vitro Study for Tapered Conical Connection Implants. Materials (Basel). 2022;15(1): 364. [17] DERKSEN W, TAHMASEB A, WISMEIJER D. Randomized Clinical Trial comparing clinical adjustment times of CAD/CAM screw-retained posterior crowns on ti‐base abutments created with digital or conventional impressions. One‐year follow-up. Clin Oral Implants Res. 2021;32(8):962-970. [18] MANGANO F, MARGIANI B, ADMAKIN O. A Novel Full-Digital Protocol (SCAN-PLAN-MAKE-DONE®) for the Design and Fabrication of Implant-Supported Monolithic Translucent Zirconia Crowns Cemented on Customized Hybrid Abutments: A Retrospective Clinical Study on 25 Patients. Int J Environ Res Public Health. 2019; 16(3):317. [19] LERNER H, MOUHYI J, ADMAKIN O, et al. Artificial intelligence in fixed implant prosthodontics: a retrospective study of 106 implant-supported monolithic zirconia crowns inserted in the posterior jaws of 90 patients. BMC Oral Health. 2020;20(1):80. [20] DERKSEN W, WISMEIJER D. Three-Year Follow-up of a Randomized Clinical Trial on Screw-Retained Monolithic Zirconia Restorations on Ti-Base Abutments Based on Digital or Conventional Impression Techniques. Int J Prosthodont. 2023;36(4):410-415. [21] 曹伟玉,曹捷,刘宾益,等.2种种植修复制作工艺的Ti-base基台一体冠用于口腔种植单冠修复精度的研究[J].上海口腔医学, 2022,31(4):414-417. [22] GEHRKE P, ABAZARI C, SCHLICHTER K, et al. Qualitative and Semi-Quantitative Assessment of Processing-Related Surface Contamination of One- and Two-Piece CAD/CAM Abutments before and after Ultrasonic Cleaning. Materials (Basel). 2020;13(14):3225. [23] 李立,李婷婷,张昀,等.计算机辅助设计与制造技术在口腔修复中的应用[J].卫生职业教育,2017,35(19):152-154. [24] RAMALHO I, WITEK L, COELHO P, et al. Influence of Abutment Fabrication Method on 3D Fit at the Implant-Abutment Connection. Int J Prosthodont. 2020;33(6):641-647. [25] CARDOSO KB, BERGAMO ETP, CRUZ VDM, et al. Three-dimensional misfit between Ti-Base abutments and implants evaluated by replica technique. J Appl Oral Sci. 2020;28:e20200343. [26] ASGEIRSSON AG, SAILER I, GAMPER F, et al. Veneered zirconia abutments cemented on non‐original titanium bases: 1-year results of a prospective case series. Clin Oral Implants Res. 2019;30(8):735-744. [27] STUCKI L, ASGEIRSSON A, JUNG R, et al. Zirconia Restorations Cemented onto Nonoriginal Titanium Bases May Result in Increased Bleeding on Probing, Probing Depth Values, and Varying Mean Marginal Bone Levels. Int J Prosthodont. 2021;34(5):560-566. [28] GEHRKE P, SING T, FISCHER C, et al. Marginal and Internal Adaptation of Hybrid Abutment Assemblies After Central and Local Manufacturing, Respectively. Int J Oral Maxillofac Implants. 2018;33(4):808-814. [29] KOUTOUZIS T. Implant‐abutment connection as contributing factor to peri‐implant diseases. Periodontol 2000. 2019;81(1):152-166. [30] JACOBS N, SEGHI R, JOHNSTON WM, et al. Displacement and performance of abutments in narrow-diameter implants with different internal connections. J Prosthet Dent. 2022;127(1):100-106. [31] ÇAKMAK G, GÜVEN ME, DONMEZ MB, et al. Effect of internal connection type and screw channel angle on the screw stability of anterior implant‐supported zirconia crowns.Clin Oral Implants Res. 2023;34(11):1248-1256. [32] QIU H, ZHANG Y, HUANG W, et al. Sintering Properties of Tetragonal Zirconia Nanopowder Preparation of the NaCl + KCl Binary System by the Sol–Gel–Flux Method. ACS Sustainable Chem. Eng. 2023;11(3): 1067-1077. [33] ADOLFI D, GRANGEIRO MTV, AUSIELLO P, et al. Effect of Antirotational Two-Piece Titanium Base on the Vertical Misfit, Fatigue Behavior, Stress Concentration, and Fracture Load of Implant-Supported Zirconia Crowns. Materials (Basel). 2023;16(13):4848. [34] MISHRA SK, CHOWDHARY R, KUMARI S. Microleakage at the Different Implant Abutment Interface: A Systematic Review. J Clin Diagn Res. 2017;11(6):ZE10-ZE15. [35] GINER S, BARTOLOMÉ JF, GOMEZ-COGOLLUDO P, et al. Mechanical Performance of Chairside Ceramic CAD/CAM Restorations and Zirconia Abutments with Different Internal Implant Connections: In Vitro Study and Finite Element Analysis. Materials (Basel). 2021;14(17):5009. [36] GEHRKE SA, SCARANO A, CORTELLARI GC, et al. Marginal Bone Level and Biomechanical Behavior of Titanium-Indexed Abutment Base of Conical Connection Used for Single Ceramic Crowns on Morse-Taper Implant: A Clinical Retrospective Study. J Funct Biomater. 2023;14(3): 128. [37] BARBOSA GA, BERNARDES SR, DAS NEVES FD, et al. Relation between implant/abutment vertical misfit and torque loss of abutment screws. Braz Dent J. 2008;19(4):358-363. [38] KORKMAZ IH, KUL E. Investigation of the Type of Angled Abutment for Anterior Maxillary Implants: A Finite Element Analysis. J Prosthodont. 2022;31(8):689-696. [39] KAPOOR S, RODRIGUES S, MAHESH M, et al. Evaluation of Stress Generated with Different Abutment Materials and Angulations under Axial and Oblique Loading in the Anterior Maxilla: Three-Dimensional Finite Element Analysis. Int J Dent. 2021;2021:9205930. [40] ZHANG Y, YU P, YU H. Stress distribution and microgap formation in angulated zirconia abutments with a titanium base in narrow diameter implants: A 3D finite element analysis. Int J Numer Method Biomed Eng. 2022;38(7):e3610. [41] MA R, YU P, ZHANG Y, et al. Mechanical stability of angulated zirconia abutments supporting maxillary anterior single crowns on narrow-diameter implants. Clin Oral Investig. 2022;27(1):221-233. [42] KOTSAKIS GA, ROMANOS GE. Biological mechanisms underlying complications related to implant site preparation. Periodontol 2000. 2022;88(1):52-63. [43] MULLA SH, SEGHI RR, JOHNSTON WM, et al. Effect of cyclic loading on reverse torque values of angled screw channel systems. J Prosthet Dent. 2022;128(3):458-466. [44] POOVARODOM P, RUNGSIYAKULL C, SURIYAWANAKUL J, et al. Effect of gingival height of a titanium base on the biomechanical behavior of 2-piece custom implant abutments: A 3-dimensional nonlinear finite element study. J Prosthet Dent. 2023;130(3):380.e1-380.e9. [45] GUNCU M, AKTAS G, GUNCU G, et al. Clinical, Technical, and Radiologic Outcomes of 182 Implant-Supported Zirconia Single Crowns Using Titanium-Base Abutments: A Retrospective Study. Int J Prosthodont. 2022;35(4):553-559. [46] STRAUSS FJ, SIEGENTHALER M, HÄMMERLE CHF, et al. Restorative angle of zirconia restorations cemented on non‐original titanium bases influences the initial marginal bone loss: 5‐year results of a prospective cohort study. Clin Oral Implants Res. 2022;33(7):745-756. [47] DE TAPIA B, MOZAS C, VALLES C, et al. Adjunctive effect of modifying the implant‐supported prosthesis in the treatment of peri‐implant mucositis. J Clin Periodontol. 2019;46(10):1050-1060. [48] HERMANN JS, SCHOOLFIELD JD, SCHENK RK, et al. Influence of the Size of the Microgap on Crestal Bone Changes Around Titanium Implants. A Histometric Evaluation of Unloaded Non‐Submerged Implants in the Canine Mandible. J Periodontol. 2001;72(10):1372-1383. [49] LANG R, HILLER KA, KIENBÖCK L, et al. Influence of autoclave sterilization on bond strength between zirconia frameworks and Ti-base abutments using different resin cements. J Prosthet Dent. 2022;127(4): 617.e1-617.e6. [50] SAPONARO PC, KARASAN D, DONMEZ MB, et al. Prosthetic complications with monolithic or micro-veneered implant-supported zirconia single-unit, multiple-unit, and complete-arch prostheses on titanium base abutments: A single center retrospective study with mean follow-up period of 72.35 months. Clin Implant Dent Relat Res. 2023;25(1):99-106. [51] MEHL C, KERN M. Retention of zirconia on titanium in two-piece abutments with self-adhesive resin cements. J Prosthet Dent. 2018; 120(2):214-219. [52] VON MALTZAHN NF, HOLSTERMANN J, KOHORST P. Retention Forces between Titanium and Zirconia Components of Two‐Part Implant Abutments with Different Techniques of Surface Modification. Clin Implant Dent Relat Res. 2016;18(4):735-744. [53] GEHRKE P, ALIUS J, FISCHER C, et al. Retentive Strength of Two‐Piece CAD / CAM Zirconia Implant Abutments. Clin Implant Dent Relat Res. 2014;16(6):920-925. [54] WIEDENMANN F, LIEBERMANN A, SPINTZYK S, et al. Influence of Different Cleaning Procedures on Tensile Bond Strength Between Zirconia Abutment and Titanium Base. Int J Oral Maxillofac Implants. 2019;34(6):1318-1327. [55] PACHECO ND, SENNA PM, GOMES RS, et al. Influence of luting space of zirconia abutment on marginal discrepancy and tensile strength after dynamic loading. J Prosthet Dent. 2021;125(4):683.e1-683.e8. [56] FREIFRAU VON MALTZAHN N, BERNARD S, KOHORST P. Two‐part implant abutments with titanium and ceramic components: Surface modification affects retention forces-An in‐vitro study. Clin Oral Implants Res. 2019;30(9):903-909. [57] MEHL C, ZHANG Q, LEHMANN F, et al. Retention of zirconia on titanium in two-piece abutments with self-adhesive resin cements. J Prosthet Dent. 2018;120(2):214-219. |
| [1] | Zhu Wenbo, Zhang Xujing, Xu Yan, Shi Xintong. Design and mechanical performance of cell-gradient scaffolds based on three-period minimal surface [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(16): 3449-3457. |
| [2] | Wu Zhixin, Jiang Wenwen, Zhan Jianhui, Li Yangshurun, Ren Wenyan, Wang Yiyu. Hydrogels: role and problems in the repair of oral and maxillofacial defects [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(10): 2178-2188. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||