[1] SLAGTER KW, MEIJER HJA, HENTENAAR DFM, et al. Immediate single-tooth implant placement with simultaneous bone augmentation versus delayed implant placement after alveolar ridge preservation in bony defect sites in the esthetic region: A 5-year randomized controlled trial. J Periodontol. 2021;92(12):1738-1748.
[2] FANG CH, SUN CK, LIN YW, et al. Metformin-Incorporated Gelatin/Nano-Hydroxyapatite Scaffolds Promotes Bone Regeneration in Critical Size Rat Alveolar Bone Defect Model. Int J Mol Sci. 2022;23(1):558-564.
[3] HOLLÝ D, KLEIN M, MAZREKU M, et al. Stem Cells and Their Derivatives-Implications for Alveolar Bone Regeneration: A Comprehensive Review. Int J Mol Sci. 2021;29(21):11746.
[4] WANG CW, ASHNAGAR S, GIANFILIPPO RD, et al. Laser-assisted regenerative surgical therapy for peri-implantitis: A randomized controlled clinical trial. J Periodontol. 2021;92(3):378-388.
[5] LU JJ, WANG ZS, ZHANG HY, et al. Bone Graft Materials for Alveolar Bone Defects in Orthodontic Tooth Movement. Tissue Eng Part B Rev. 2022;28(1):35-51.
[6] FAN Y, CUI C, ROSEN CJ, et al. Klotho in Osx+-mesenchymal progenitors exerts pro-osteogenic and anti-inflammatory effects during mandibular alveolar bone formation and repair. Signal Transduct Target Ther. 2022;11(1):155.
[7] 刘亮亮,王宁,仲维剑,等.改良型富血小板纤维蛋白在上颌窦底提升术中成骨效果的临床研究[J]. 中国实用口腔科杂志,2023, 16(1):76-81.
[8] LI T, LONG H, NIU W, et al. The repair and regeneration mechanism of platelet-rich fibrin-promoting tissue after alveolar bone defect through the notch pathway. Cell Mol Biol. 2023;69(7):85-90.
[9] VEMAGIRI CT, DAMERA S, PAMIDI VRC, et al. Management of Alveolar Cleft Defect by Iliac Crest Secondary Bone Grafting: A Case Report[. Int J Clin Pediatr Dent. 2022;15(4):472-474.
[10] YUAN Y, ZHANG HM, HUANG H. microRNAs in inflammatory alveolar bone defect: A review. J Periodontal Res. 2021;56(2):219-225.
[11] SHAHEEN MY. Nanocrystalline hydroxyapatite in periodontal bone regeneration: A systematic review. Saudi Dent J. 2022;34(8): 647-660.
[12] YU H, CAI Q, LI B, et al. The Assessment of Volumetric Changes for Alveolar Ridge Preservation or Reconstruction by Three-dimensional Analysis at Posterior Extraction Sites with Severe Bone Defects Using DBBM-C Collagen Membrane and PRF: A Prospective and Randomized Clinical Trial. Int J Periodontics Restorative Dent. 2024;10(3):1-27.
[13] 邹多宏,刘昌奎,薛洋,等.帐篷钉技术在牙槽骨修复与再生中的临床应用及操作规范[J].中国口腔颌面外科杂志,2021,19(1):1-5.
[14] 杨艳兰,徐普.干细胞修复牙槽骨缺损:微环境认知新进展[J].解放军医学杂志,2021,46(4):404-409.
[15] ZWITTNIG K, MUKADDAM K, VEGH D, et al. Platelet-Rich Fibrin in Oral Surgery and Implantology: A Narrative Review. Transfus Med Hemother. 2022;50(4):348-359.
[16] LIU Y, GUO L, LI X, et al. Challenges and Tissue Engineering Strategies of Periodontal-Guided Tissue Regeneration. Tissue Eng Part C Methods. 2022;28(8):405-419.
[17] BEE SL, HAMID ZAA. Asymmetric resorbable-based dental barrier membrane for periodontal guided tissue regeneration and guided bone regeneration: A review. J Biomed Mater Res B Appl Biomater. 2022;110(9):2157-2182.
[18] BANIULYTE G, ALI K, BURNS L. Guided tissue regeneration techniques involving blood-derived products in periradicular surgery: a systematic review and meta-analysis protocol. JBI Evid Synth. 2021;19(12): 3378-3383.
[19] 刘堃,王舒思,张磊,等.块状自体骨联合脱细胞牛骨基质重建牙槽嵴的影像学观察[J].口腔医学,2021,41(4):312-317.
[20] AL MALAK A, EL MASRI Y, AL ZIAB M, et al. Current State of Clinical Trials Regarding Alveolar Bone Grafting. Cleft Palate Craniofac J. 2023; 21(29):1032-1038.
[21] MIRON RJ, MORASCHINI V, FUJIOKA-KOBAYASHI M, et al. Use of platelet-rich fibrin for the treatment of periodontal intrabony defects: a systematic review and meta-analysis. Clin Oral Investig. 2021;25(5): 2461-2478.
[22] AMARALVALLADÃO CA JR, FREITAS MONTEIRO M, JOLY JC. Guided bone regeneration in staged vertical and horizontal bone augmentation using platelet-rich fibrin associated with bone grafts: a retrospective clinical study. Int J Implant Dent. 2020;17(1):72.
[23] USTAOĞLU G, UĞUR AYDIN Z, ÖZELÇI F. Comparison of GTR, T-PRF and open-flap debridement in the treatment of intrabony defects with endo-perio lesions: a randomized controlled trial. Med Oral Patol Oral Cir Bucal. 2020;1(1):117-123.
[24] ALSHUJAA B, TALMAC AC, ALTINDAL D, et al. Clinical and radiographic evaluation of the use of PRF, CGF, and autogenous bone in the treatment of periodontal intrabony defects: Treatment of periodontal defect by using autologous products. J Periodontol. 2023;6(17): 562-567.
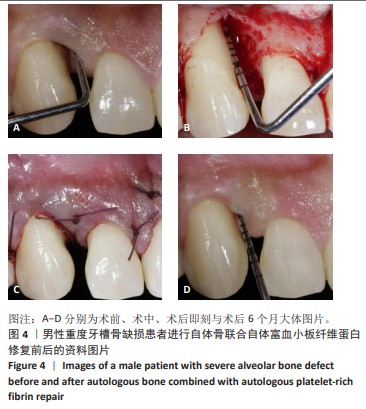
[25] 都吉秀,陈琰,曾文娟.自体骨植入联合富血小板纤维蛋白在充填自体牙移植牙周骨缺损中的效果[J].实用临床医学,2021,22(3): 51-53,59.
[26] 李晶,孙晓军,孟兵.自体骨联合PRF在阻生下颌第三磨牙致第二磨牙远中骨缺损的应用[J].医学综述,2021,27(5):1012-1016.
[27] 李娜,刘静,范多娇.富血小板纤维蛋白膜在老年糖尿病患者牙周组织缺损再生中的应用效果研究[J].老年医学与保健,2023, 29(3):579-584.
[28] 汪婷,范后宝,张森,等.隐神经脉冲射频联合关节腔富血小板血浆注射治疗膝关节骨关节炎的疗效[J].江苏医药,2023,49(6): 572-576,582.
[29] GOLLAPUDI M, BAJAJ P, OZA RR. Injectable Platelet-Rich Fibrin - A Revolution in Periodontal Regeneration. Cureus. 2022;14(8): 2651-2658.
[30] ARSHAD S, TEHREEM F, REHAB KHAN M, et al. Platelet-Rich Fibrin Used in Regenerative Endodontics and Dentistry: Current Uses, Limitations, and Future Recommendations for Application. Int J Dent. 2021;11(23):1013-1019.
[31] 李权,李媛怡,曹东升.改良型富血小板纤维蛋白在中厚皮片供区创面中的临床应用[J].安徽医科大学学报,2021,56(4):656-659.
[32] DOLLY AS, PL R, BLAISIE RAJULA P, et al. A Comparative Cytocompatibility Assessment of Leukocyte-Platelet-Rich Fibrin (L-PRF) and Injectable Platelet-Rich Fibrin (I-PRF) on the Pre-osteoblastic MG-63 Cell Line in Chronic Periodontitis Patients: An In Vitro Study. Cureus. 2023;15(11):1062-1069.
[33] CSIFÓ-NAGY BK, SÓLYOM E, BOGNÁR VL, et al. Efficacy of a new-generation platelet-rich fibrin in the treatment of periodontal intrabony defects: a randomized clinical trial. BMC Oral Health. 2021;15(1):580.
[34] ALSHOIBY MM, FAWZY EL-SAYED KM, ELBATTAWY W, et al. Injectable platelet-rich fibrin with demineralized freeze-dried bone allograft compared to demineralized freeze-dried bone allograft in intrabony defects of patients with stage-III periodontitis: a randomized controlled clinical trial. Clin Oral Investig. 2023;27(7):3457-3467.
[35] GUPTA S, JAIN A, GUPTA M, et al. Influence of periodontitis and diabetes on structure and cytokine content of platelet-rich fibrin. Oral Dis. 2023;29(8):3620-3629.
[36] FRANCISCO I, FERNANDES MH, VALE F. Platelet-Rich Fibrin in Bone Regenerative Strategies in Orthodontics: A Systematic Review. Materials (Basel). 2020;16(8):1866.
[37] FARSHIDFAR N, JAFARPOUR D, FIROOZI P, et al. The application of injectable platelet-rich fibrin in regenerative dentistry: A systematic scoping review of In vitroandIn vivostudies. Jpn Dent Sci Rev. 2022; 58(36):89-123.
[38] TAVELLI L, CHEN CJ, BAROOTCHI S, et al. Efficacy of biologics for the treatment of periodontal infrabony defects: An American Academy of Periodontology best evidence systematic review and network meta-analysis. J Periodontol. 2022;93(12):1803-1826.
[39] MIJIRITSKY E, ASSAF HD, PELEG O, et al. Use of PRP, PRF and CGF in Periodontal Regeneration and Facial Rejuvenation-A Narrative Review. Biology (Basel). 2021;10(4):317-324.
[40] 杜宁,刘昕,田啊林,等.牙周炎NLRP3炎性小体表达量与炎症反应、牙槽骨吸收的相关性研究[J]. 湖南师范大学学报(医学版), 2021,18(2):59-62.
[41] 谢一敦,王生党.128例慢性牙周炎Pg感染患者血清MMP-3、HMGB-1水平与病情严重程度的相关性分析[J].医学临床研究, 2023,40(4):561-563,567.
[42] RAZAVI P, REZAEE SA, AKHONDIAN S, et al. Matrix Metalloproteinase-3 but Not Matrix Metalloproteinase-9, Implicated in the Manifestation of Chronic Periodontitis. Rep Biochem Mol Biol. 2023;11(4):656-662.
[43] 孙帅.转化生长因子-β3诱导牙髓干细胞的应用进展[J].临床口腔医学杂志,2021,37(2):117-120.
[44] YAMADA S, TSUSHIMA K, KINOSHITA M, et al. Mouse Model of Loeys-Dietz Syndrome Shows Elevated Susceptibility to Periodontitis via Alterations in Transforming Growth Factor-Beta Signaling. Front Physiol. 2021;11(12):2213-2219. |