| [1] Tsai RJF, Tseng SCG. Human allograft limbal transplantation of corneal surface reconstructions. Cornea. 1994;13: 389.
[2] Cameron AM, Steinet JP, Sabatini DM, et al. Immunophilin FK506 binding protein associated with inositol 1, 4, 5 triSphosphaterecept or modulates calcium flux. Proc Nat Acad Sci. 1995;92(5):1784-1788.
[3] Boisgerault F, Liu Y, Anosova N, et al. Role of CD4+ and CD8+ T cells in allorecognition: lessons from cornealtransplantation. J Immunol. 2001;167(4): 1891-1899.
[4] 徐筱杰,主编.计算机辅助药物分子设计[M].北京:化学工业出版社,2004:12.
[5] 宋云龙,陆倍倍,张万年.基于结构的计算机辅助药物设计方法学与应用研究[J].药学进展, 2002, 26(6) :359-364.
[6] 何新华,谢云德,肖鹤,等.新型CD4抑制剂J2的合成及其活性评价[J]. 中国药物化学杂志, 2009, 19(4):290-292.
[7] 张磊,冯健男,崔健,等.J2小分子化合物能有效抑制小鼠急性移植物抗宿主反应的实验研究[J].军事医学科学院院刊, 2008, 32(6): 519-522.
[8] He X, Jian NF, Xin HH, et al. Potent inhibition of the CD4- dependent T cell response by J2, a novel nonpeptide organic ligand of CD4 D1. Mol Immunol. 2007;44: 784-795.
[9] He X, Han Z, Zu YY, et al. J2 prolongs the corneal allograft survival through inhibition of the CD4+ T cell-mediated response in vivo. Trans Immunol.2007;18:130-137.
[10] Da JW, Han Z, Guo JC, et al. Further study on molecular biological effects of CD4 D1 inhibitor J2 on allografts following corneal transplantation in mice. Sci Res Ess. 2010; 5(1): 63-70.
[11] 王大江,黄一飞,张晗,等.小分子化合物J2抑制小鼠角膜移植术后排斥反应的研究[J].中华眼科杂志,2009, 45(4):350-355.
[12] 王大江,黄一飞,张晗,等.小分子化合物J2对小鼠角膜移植术后植片RANTES基因表达的影响[J]. 眼视光学杂志, 2008,10(3): 174-177.
[13] 张晗,黄一飞,王丽强.小分子免疫抑制剂J2抗移植排斥的实验研究[J]. 解放军药学学报, 2006, 22(2):115-118.
[14] 张晗,黄一飞,王丽强.基于CD4分子构型设计的小分子免疫抑制药J2抗移植排斥反应的作用研究[J]. 医药导报, 2006, 25(8): 723-725.
[15] 张晗,黄一飞,王丽强.小分子化合物J2在抑制小鼠角膜移植排斥反应中作用的初步研究[J]. 中华眼科杂志,2007, 43(7):608- 612.
[16] 王大江,黄一飞,张晗.小分子化合物J2对小鼠淋巴细胞的影响[J]. 解放军药学学报,2007, 23(2): 81-84.
[17] 赵勇,主编.移植免疫耐受[M]. 北京:中国医药科技出版社, 2005: 2-11.
[18] 杨朝忠,耿燕,姚晓明,主编. 眼表移植学[M]. 北京:军事医学科学出版社,2008:138-141.
[19] Larkin DF, Calder VL, Lightman SL. Identification and characterization of cells infiltrating the graft and aqueous humour in rat corneal allograft rejection. Clin Exp Immunol. 1997;107: 381-391
[20] Kiritoshi A, SundarRaj N, Thoft RA. Differentiation in cultured limbal epithelium as defined by keratin expression. Invest Opthalmol Vis Sic. 1991;32: 3073-3077.
[21] Kenyon KR, Tseng SCG. Limal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96: 709.
[22] Sarikcioglu L, Duygulu E, Aydin H, et al. Effects of intrathecal administration of FK506 after sciatic nerve crush injury. J Reconstr Microsurg. 2006;22(8):649-654.
[23] Hontanilla B, Yeste L, Auba C, et al. Neurnonal quantification in cold preserved nerve autografts and treatment with FK506 through osmotic pump s compared to nerve autografts. J Reconstr Microsurg. 2006;22(5):363-374.
[24] 陈实,主编.移植免疫学[M]. 武汉:湖北科学技术出版社,1998: 78-91.
[25] Streilein JW, Arancibia-Caracamo C, Osawa H. The role o f minor histocompatibility alloantigens in penetrating keratoplasty. Dev Ophthalmol. 2003;36: 74-88.
[26] Boisgérault F, Liu Y, Anosova N, et al. Role of CD4+ and CD8+ T cells in allorecognition: lessons from corneal transplantation. J Immunol. 2001;167(4): 1891-1899.
[27] Pleyer U, Milani JK, Dukes A, et al. Effect of topically applied anti-CD4 monoclonal antibodies on orthotopic corneal allografts in a rat model. Invest Ophthalmol Vis Sci. 1995; 36(1): 52-61.
[28] Pindjáková J, Vítová A, Krulová M, et al. Corneal rat-to-mouse xenotransplantation and the effects of anti-CD4 or anti-CD8 treatment on cytokine and nitric oxide production Transpl Int. 2005;18(7):854-862.
[29] Yamada J, Kurimoto I, Streilein W. Role of CD4+ T cells in immunobiology of orthotopic corneal transplants in mice. Invest Ophthalmol Vis Sci. 1999; 40: 2614-2621
[30] 史伟云,谢立信. CD4和CD8基因敲除鼠行穿透性角膜移植术后免疫排斥特征的研究[J].中华眼科杂志,2005, 41(4): 350-354.
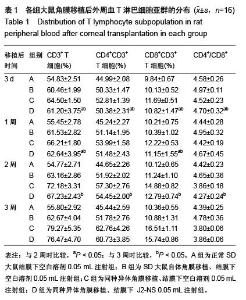
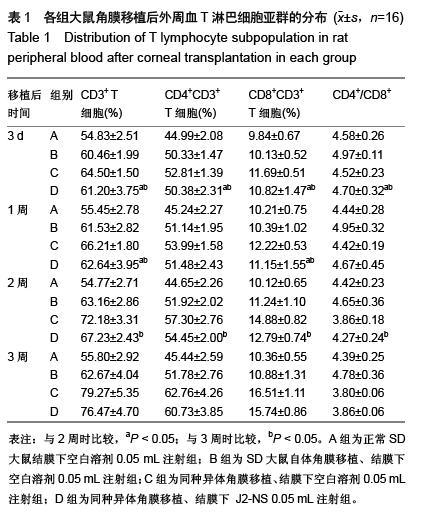
[31] 刘彤,王鹏志,朱理玮,等.大鼠小肠移植后外周血T淋巴细胞亚群的变化[J]. 中华器官移植杂志,1996, 17(1):15-17.
[32] 吴京,王小宁.角膜移植排斥反应的实验研究Ⅱ-T淋巴细胞亚群及T-CEC的变化[J]. 眼科新进展,1997, 17(3):137-139.
[33] Creemers P, Brink J, Wainwright H, et al. Evaluation of peripheral blood CD4 and CD8 lymphocyte subsets, CD69 expression and histologic rejection grade as diagnostic markers for the presence of cardiac allograft rejection. TransplImmunol. 2002;10(4): 285-292.
[34] Völker-Dieben HJ, Claas FH, Schreuder GM, et al. Beneficial effect of HLA-DR matching on the survival of corneal allografts. Transplantation.2000; 70: 640-648.
[35] Sheldon S, Poulton K. HLA typing and its influence on organ transplantation. Methods Mol Biol. 2006;333: 157-174.
[36] Reinhard T, Böhringer D, Enczmann J, et al. Improvement of graft prognosis in penetrating normal-risk keratoplasty by HLA class I and II matching. Eye (Lond). 2004;18(3): 269-277. |