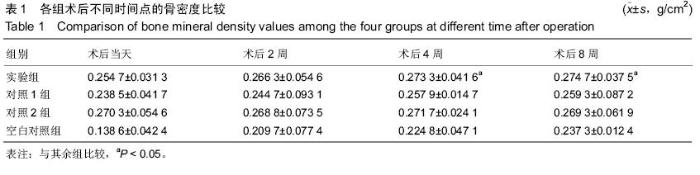
| [1] 汤勇智,陈建庭,徐俊昌,等.纳米珍珠层人工骨修复兔桡骨缺损的实验研究[J].广东医学,2009,30(10):1429-1431.[2] 李晓红,朱晓姝,赵献银,等.荧光标记拔牙创口骨愈合过程中矿化沉积速度的研究[J].中国骨质疏松杂志, 2007, 13(7):486-489.[3] 刘源.海螵蛸/骨形态发生蛋白复合人工骨成骨及再血管化的初步试验研究[D].大连医科大学,2012. [4] Bosch P,Musgrave D,Ghivizzani S,et al.The efficiency of muscle-derived cell-mediated bone formation.Cell Transplant.2000;9(4):463-470. [5] 裴国献,魏宽海,金丹,等.组织工程学实验技术[M].北京:人民军医出版社, 2006:78-98.[6] Wong EW,Sheehan PE,Lieber CM. Nanobcammechanics elasticity, strength and toughness of nanorods and nanotubes. Science. 1997;277:1971-1975.[7] Puelacher WC, Wisser J, Vacanti CA, et al. Temporomandibular joint disc replacement made by tissue engineered growth of cartilage.J Oral Maxillofac Surg.2007;52(11):1172-1173.[8] Athanasiou KA,Niederauer GG,Agrawal CM,et al. Sterilization,toxicity,biocompatibility and clinical applications of polylactic acid/polyglycolic acid copolymers.Biomaterials.1996;17:93-94.[9] 刘艺,顾国奎,刘克泉,等.海螵蛸接骨动物实验的组织学研究[J].中国中医骨伤科杂志, 1996,3(5):6-8.[10] Ashiku SK,Randolph MA,Vacanti CA,et al.Tissue Engineered cartilage.Mater Sci Forum. 1997;250: 129-130.[11] Berland S,Delattre 0,Borzeix S,et al.Nacre/bone interface changes in durable nacreendosseous implants in sheep. Biomaterials 2005;26(15):2767-2773.[12] 汤勇智.纳米珍珠层人工骨的制备及实验研究[D].南方医科大学,2009.[13] 舒晓军,杨青芳,杜江华,等.聚乳酸的改性及应用[J].合成纤维工业, 2006,29(6):44-47.[14] 刘金标,陈建庭,金大地,等.珍珠层/聚乳酸组合人工骨体外相容性及降解实验研究[J].第一军医大学学报, 2003, 23(22):130-132.[15] 汤勇智,陈建庭,赵成毅,等.纳米珍珠层粉的降解实验及其复合人工骨的生物相容性研究[J].中国矫形外科杂志, 2009,17(2):131-134.[16] Atlan G,Delattre OBerland S,LeFaou A,et al.Interface between boneandna-creimplants in sheep. Biomaterials.1999;11:1017-1022.[17] 李鹏,毛克亚,江涛,等.β-磷酸三钙/α-半水硫酸钙复合人工骨体外降解速度可与成骨一致[J].中国组织工程研究与临床康复,2011,15(51):9501-9504.[18] 刘艺,顾国奎,刘克泉.海缥峭接骨动物实验的组织学研究[J].中国中医骨伤科杂志,1996,3(5):6-8.[19] Burstein FD,griyan S.Tetracycline fluorescence incident photometry:a new technique to quantitate bone formation.J Craniofac Surg.1994;5(2):77-80.[20] Duplat D,Chabadel A,Gallet M,et al.The in vitro osteoclastic degradation of nacre. Biomaterials. 2007; 28(12):2155-2162. |