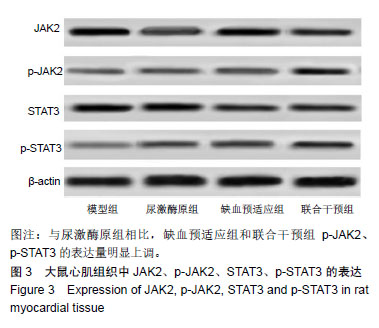
| [1]Sheng X,Chen M,Huang B,et al.Cardioprotective effects of low-level carotid baroreceptor stimulation against myocardial ischemia-reperfusion injury in canine model.J Interv Card Electrophysiol.2016;45(2):131-140.[2]Kurian GA, Rashmi R, Srinivasan V, et al. The Role of Oxidative Stress in Myocardial Ischemia and Reperfusion Injury and Remodeling: Revisited. Oxid Med Cell Longev. 2016;2016:1656450. [3]Robert R, Vinet M, Jamet A, et al.Effect of non-invasive remote ischemic preconditioning on intra-renal perfusion in volunteers. J Nephrol. 2017;30(3):393-395.[4]王枫岭,刘志远,徐娜,等.尿激酶—肝素系列溶栓治疗不稳定型心绞痛的临床疗效[J].河南医学研究,2001,10(2):125-127.[5]高建波,张颖,娄建石.多疗程无创性延迟肢体缺血预适应保护大鼠心肌缺血再灌注损伤的持久效应研究[J].临床心血管病杂志, 2014,30(5):439-442.[6]徐雷,安少波,杜晓静,等.尿激酶原与尼可地尔改善STEMI患者急诊PPCI术后的临床效果[J].重庆医学, 2018,47(26):3458-3460, 3463.[7]赵晓楠,袁恒杰,朱学慧,等.无创性延迟肢体缺血预适应对抗大鼠脑缺血再灌注损伤的内皮机制[J].中国医院药学杂志, 2015, 35(10):877-881.[8]丁洪涛,刘霖,王智超,等.p38 MAPK抑制物对大鼠心肌缺血再灌注损伤的保护作用及凋亡信号通路的影响[J]. 临床和实验医学杂志,2014,13(6):425-428.[9]Yu H,Guan Q,Guo L,et al.Gypenosides alleviate myocardial ischemia-reperfusion injury via attenuation of oxidative stress and preservation of mitochondrial function in rat heart. Cell Stress Chaperones. 2016 ;21(3):429-437.[10]Liao YH, Xia N, Zhou SF, et al.Interleukin-17A contributes to myocardial ischemia/reperfusion injury by regulating cardiomyocyte apoptosis and neutrophil infiltration. J Am Coll Cardiol. 2012;59(4):420-429. [11]Gurewich V.Thrombolysis; a critical first-line therapy with an unfulfilled potential. Am J Med. 2016;129(6):573-575.[12]汪雁博,谷新顺,傅向华. 国产重组人尿激酶原治疗急性心肌梗死有效性和安全性的Meta分析[J].中国全科医学, 2016, 19(17): 2083-2088.[13]孙凯,陈文华,张颖,等.无创性延迟肢体缺血预适应对心肌梗死大鼠预后的影响[J].中国病理生理杂志,2017,33(1):116-122. [14]Xuan F,Jian J.Epigallocatechin gallate exerts protective effects against myocardial ischemia/reperfusion injury through the PI3K/Akt pathway-mediated inhibition of apoptosis and the restoration of the autophagic flux. Int J Mol Med. 2016;38(1):328-336.[15]Cheng L,Jin Z,Zhao R,et al.Resveratrol attenuates inflammation and oxidative stress induced by myocardial ischemia-reperfusion injury: role of Nrf2/ARE pathway. Int J Clin Exp Med. 2015;8(7):10420-10428.[16]Tang XL, Liu JX, Dong W,et al.Cardioprotective effect of protocatechuic acid on myocardial ischemia/reperfusion injury. J Pharmacol Sci.2014;125(2):176183.[17]李燕,陈文华,孙凯,等.无创性延迟肢体缺血预适应对心脏性猝死的预防作用研究[J].中国药理学通报, 2016, 32(11): 1565-1570.[18]朱娜,要瑞莉,刘俊双,等.大鼠肢体缺血/再灌注后心肌细胞凋亡及氧化应激的调节作用[J].中国老年学杂志, 2015,35(23): 6666-6668.[19]Cheng Z,Ling LI,Xueying M O, et al. Non-invasive remote limb ischemic postconditioning protects rats against focal cerebral ischemia by upregulating STAT3 and reducing apoptosis.Int J Mol Med.2014;34(4):957-966.[20]Zhao GL,Yu L M,Gao WL,et al.Berberine protects rat heart from ischemia/reperfusion injury via activating JAK2/STAT3 signaling and attenuating endoplasmic reticulum stress.Acta Pharmacologica Sinica.2016;37(3):354-367.[21]Yang Y, Duan W, Jin Z, et al.JAK2/STAT3 activation by melatonin attenuates the mitochondrial oxidative damage induced by myocardial ischemia/reperfusion injury. J Pineal Res.2013;55(3):275-286.[22]Liu S,Yang Y,Song YQ,et al.Protective effects of N(2)-L-alanyl-L-glutamine mediated by the JAK2/STAT3 signaling pathway on myocardial ischemia reperfusion. Mol Med Rep.2018;17(4):5102-5108. |