Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (29): 6326-6332.doi: 10.12307/2025.760
Previous Articles Next Articles
Causal relationship between immune cells and bone metabolic diseases: a Mendelian randomization analysis of European populations in international databases
Chen Tianxin1, 2, Zhang Zhilong1, Zhang Shuai1, Gao Yun1, Zhu Yuqi1, Yang Shengping1
- 1Orthopedic Department, Eye Hospital, China Academy of Chinese Medical Sciences, Beijing 100040, China; 2Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China
-
Received:2024-07-24Accepted:2024-10-11Online:2025-10-18Published:2025-03-08 -
Contact:Yang Shengping, Attending physician, Orthopedic Department, Eye Hospital, China Academy of Chinese Medical Sciences, Beijing 100040, China -
About author:Chen Tianxin, MD candidate, Orthopedic Department, Eye Hospital, China Academy of Chinese Medical Sciences, Beijing 100040, China; Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China -
Supported by:Central High-Level Traditional Chinese Medicine Hospital Project of Eye Hospital, China Academy of Chinese Medical Science, No. GSP1-06 (to YSP); China’s National Administration of Traditional Chinese Medicine International Cooperation Special Project, No. 0610-2240NF0215 (to GY); China Academy of Chinese Medical Sciences Innovation Fund - Major Research and Development Project, No. CI2021A02012 (to GY); The 2nd Shijingshan District Famous Traditional Chinese Medicine Inheritance Workshop, No. Zhu Yuqi workshop 2022 (to ZYQ)
CLC Number:
Cite this article
Chen Tianxin, , Zhang Zhilong, Zhang Shuai, Gao Yun, Zhu Yuqi, Yang Shengping. Causal relationship between immune cells and bone metabolic diseases: a Mendelian randomization analysis of European populations in international databases[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6326-6332.
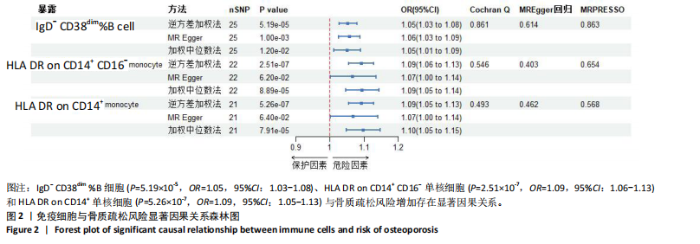
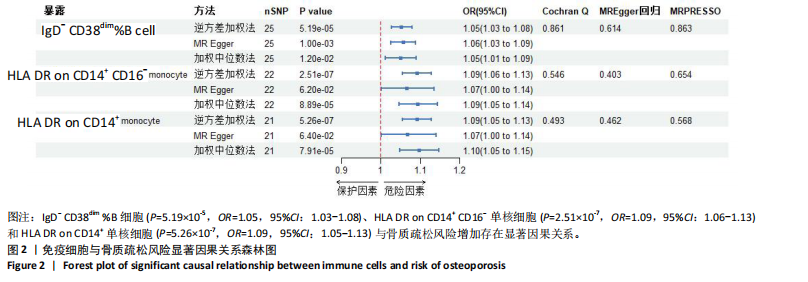
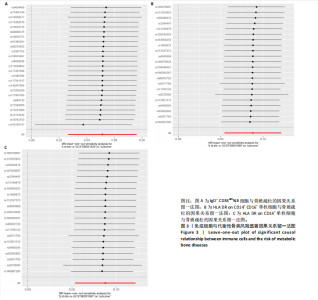
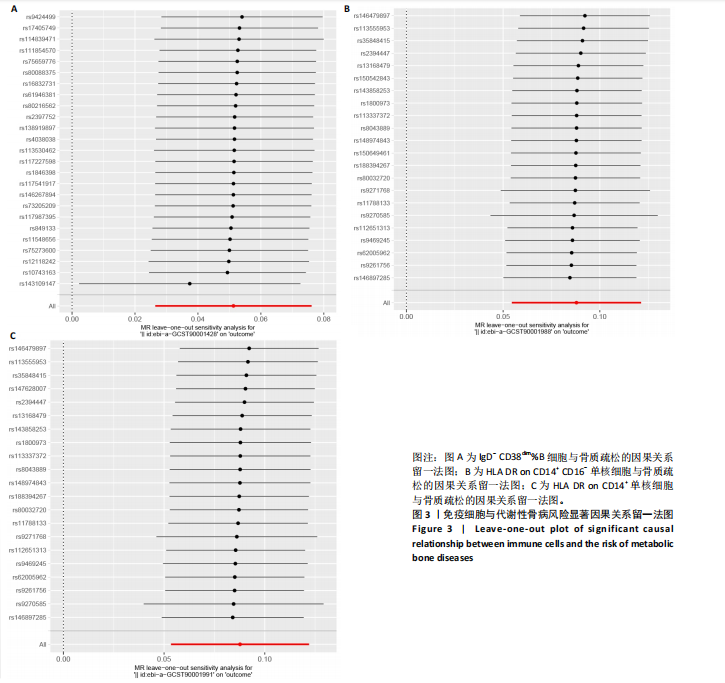
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

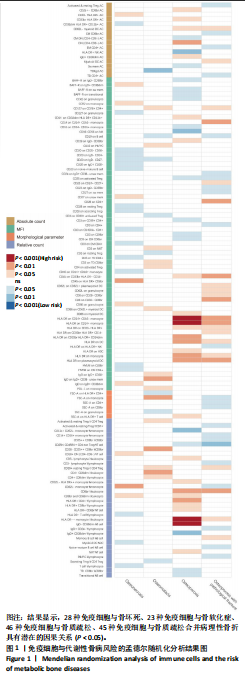
2.1 工具变量筛选 731种免疫细胞达到显著阈值的工具变量数量从3个到691个不等。731种免疫细胞工具变量的F值范围为19.55-2 435.82,均符合F > 10,说明此次研究具有弱工具变量偏倚的可能性较小。 2.2 孟德尔随机化分析结果 逆方差加权法分析显示,28种免疫细胞与骨坏死、23种免疫细胞与骨软化症、46种免疫细胞与骨质疏松、45种免疫细胞与骨质疏松合并病理性骨折具有潜在的因果关系(P < 0.05),具体见图1。 IgD- CD38dim%B细胞(P=5.19×10-5,OR=1.05,95%CI:1.03- 1.08)、HLA DR on CD14+ CD16-单核细胞(P=2.51×10-7,OR=1.09,95%CI:1.06-1.13)和HLA DR on CD14+单核细胞(P=5.26×10-7,OR=1.09,95%CI:1.05-1.13)与骨质疏松风险增加存在显著因果关系,并且MR-Egger法、加权中位数法显示因果关系方向一致,见图2。 2.3 敏感性分析结果 Cochran’s Q检验结果显示,IgD- CD38dim%B细胞、HLA DR on CD14+ CD16-单核细胞和HLA DR on CD14+单核细胞与骨质疏松的工具变量不存在异质性(P > 0.05)。MR-PRESSO和MR-Egger回归分析显示显著因果关系的工具变量不存在水平多效性(P > 0.05),见图2。留一法分析显示显著因果关系的结果在逐个剔除单核苷酸多态性后结果具有稳定性,见图3。MR Steiger检验结果显示,IgD- CD38dim%B细胞、HLA DR on CD14+ CD16-单核细胞、HLA DR on CD14+单核细胞对骨质疏松的方向均为“TRUE”,并且均P < 0.000 1,说明结果未受反向因果关系影响。"
| [1] 朱汉民,王松,肖文琳,等.线粒体自噬调控骨代谢[J].中国组织工程研究, 2025,29(8):1676-1683. [2] CHENG K, GUO Q, YANG W, et al. Mapping Knowledge Landscapes and Emerging Trends of the Links Between Bone Metabolism and Diabetes Mellitus: A Bibliometric Analysis From 2000 to 2021. Front Public Health. 2022;10:918483. [3] 郭曹培,程飘涛,杨成兵,等.骨免疫与骨代谢[J].中国组织工程研究,2024, 28(14):2261-2266. [4] CAO RR, YU XH, XIONG MF, et al. The immune factors have complex causal regulation effects on bone mineral density. Front Immunol. 2022;13:959417. [5] ZHENG J, YAO Z, XUE L, et al. The role of immune cells in modulating chronic inflammation and osteonecrosis. Front Immunol. 2022;13:1064245. [6] CHAROENNGAM N. Vitamin D and Rheumatic Diseases: A Review of Clinical Evidence. Int J Mol Sci. 2021;22(19):10659. [7] FISCHER V, HAFFNER-LUNTZER M. Interaction between bone and immune cells: Implications for postmenopausal osteoporosis. Semin Cell Dev Biol. 2022;123:14-21. [8] AURORA R, VEIS D. Does Aging Activate T-cells to Reduce Bone Mass and Quality? Curr Osteoporos Rep. 2022;20(5):326-333. [9] EPSLEY S, TADROS S, FARID A, et al. The Effect of Inflammation on Bone. Front Physiol. 2021;11:511799. [10] Orrù V, Steri M, Sidore C, et al. Complex genetic signatures in immune cells underlie autoimmunity and inform therapy. Nat Genet. 2020;52(10):1036-1045. [11] KURKI MI, KARJALAINEN J, PALTA P, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613(7944):508-518. [12] SKRIVANKOVA VW, RICHMOND RC, WOOLF BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. JAMA. 2021;326(16):1614-1621. [13] EMDIN CA, KHERA AV, KATHIRESAN S. Mendelian Randomization. JAMA. 2017; 318(19):1925-1926. [14] LYU F, WANG L, JIA Y, et al. Analysis of Zinc and Stromal Immunity in Disuse Osteoporosis: Mendelian Randomization and Transcriptomic Analysis. Orthop Surg. 2023;15(11):2947-2959. [15] 陈天鑫,张智龙,朱瑜琪,等.恶性肿瘤与骨密度因果关系的双向两样本孟德尔随机化研究[J].现代预防医学,2023,50(18):3276-3280+3287. [16] 陈天鑫,董婷婷,李妍,等.孟德尔随机化分析血液代谢物与肌少症相关特征的因果关系[J].中国组织工程研究,2024,28(27):4288-4292. [17] FEIGE J, MOSER T, AKGÜN K, et al. Repeated iv anti-CD20 treatment in multiple sclerosis: Long-term effects on peripheral immune cell subsets. Ann Clin Transl Neurol. 2024;11(2):450-465. [18] JAVELOT MJ, SERGHERAERT J, AGBO-GODEAU S, et al. Rituximab as a trigger factor of medication-related osteonecrosis of the jaw. A case report. J Stomatol Oral Maxillofac Surg. 2020;121(3):300-304. [19] KERIBIN P, GUERROT D, JARDIN F, et al. Osteonecrosis of the Jaw in a Patient Presenting With Post-Transplantation Lymphoproliferative Disorder Treated With Rituximab: A Case Report. J Oral Maxillofac Surg. 2017;75(12):2599-2605. [20] ALLEGRA A, OTERI G, ALONCI A, et al. Association of osteonecrosis of the jaws and POEMS syndrome in a patient assuming rituximab. J Craniomaxillofac Surg. 2014;42(4):279-282. [21] GONZÁLEZ-OSUNA L, SIERRA-CRISTANCHO A, ROJAS C, et al. Premature Senescence of T-cells Favors Bone Loss During Osteolytic Diseases. A New Concern in the Osteoimmunology Arena. Aging Dis. 2021;12(5):1150-1161. [22] LIU CG, LI DY, GAO X, et al. Examining the causal relationship between circulating immune cells and the susceptibility to osteomyelitis: A Mendelian randomization study. Int Immunopharmacol. 2024;131:111815. [23] WANG C, ZHU Y, PAN D. Identifying the causal relationship between immune factors and osteonecrosis: a two-sample Mendelian randomization study. Sci Rep. 2024;14(1):9371. [24] KUWAHARA N, KODAKA T, ZUSHI Y, et al. T-cell large granular lymphocytic (LGL) leukemia consists of CD4+/CD8dim and CD4-/CD8+ LGL populations in association with immune thrombocytopenia, autoimmune neutropenia, and monoclonal B-cell lymphocytosis. J Clin Exp Hematop. 2019;59(4):202-206. [25] TAN Y, QIU Z, ZENG H, et al. Microcystin-leucine-arginine impairs bone microstructure and biomechanics by activating osteoimmune response and inhibiting osteoblasts maturation in developing rats. Toxicology. 2023;494:153595. [26] EROGLU S, KARATAS G. Platelet/lymphocyte ratio is an independent predictor for osteoporosis. Saudi Med J. 2019;40(4):360-366. [27] AKBAS EM, GUNGOR A, OZCICEK A, et al. Vitamin D and inflammation: evaluation with neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. Arch Med Sci. 2016;12(4):721-727. [28] MORRIS HA, TURNER AG, ANDERSON PPH. Vitamin-D regulation of bone mineralization and remodelling during growth. Front Biosci (Elite Ed). 2012;4(2): 677-689. [29] RAMPOLDI F, DONATO E, ULLRICH L, et al. γδ T cells license immature B cells to produce a broad range of polyreactive antibodies. Cell Rep. 2022;39(8):110854. [30] FRASE D, LEE C, NACHIAPPAN C, et al. The Inflammatory Contribution of B-Lymphocytes and Neutrophils in Progression to Osteoporosis. Cells. 2023; 12(13):1-15. [31] LAGERQUIST MK, GUPTA P, SEHIC E, et al. Reduction of Mature B Cells and Immunoglobulins Results in Increased Trabecular Bone. JBMR Plus. 2022;6(9): e10670. [32] DRUMMOND FJ, MACKRILL JJ, O’SULLIVAN K, et al. CD38 is associated with premenopausal and postmenopausal bone mineral density and postmenopausal bone loss. J Bone Miner Metab. 2006;24(1):28-35. [33] BOLZONI M, TOSCANI D, COSTA F, et al. The link between bone microenvironment and immune cells in multiple myeloma: Emerging role of CD38. Immunol Lett. 2019;205:65-70. [34] MAGGI J, CARRASCAL M, SOTO L, et al. Isolation of HLA-DR-naturally presented peptides identifies T-cell epitopes for rheumatoid arthritis. Ann Rheum Dis. 2022; 81(8):1096-1105. [35] DOUROUDIS K, TARASSI K, ATHANASSIADES T, et al. HLA alleles as predisposal factors for postmenopausal osteoporosis in a Greek population. Tissue Antigens. 2007;69(6):592-596. [36] TSUJI S, MUNKHBAT B, HAGIHARA M, et al. HLA-A*24-B*07-DRB1*01 haplotype implicated with genetic disposition of peak bone mass in healthy young Japanese women. Hum Immunol. 1998;59(4):243-249. [37] LIN YC, ZHENG G, LIU HT, et al. USP7 promotes the osteoclast differentiation of CD14+ human peripheral blood monocytes in osteoporosis via HMGB1 deubiquitination. J Orthop Translat. 2023;40: 80-91. [38] AMANO S, KAWAKAMI K, IWAHASHI H, et al. Functional role of endogenous CD14 in lipopolysaccharide-stimulated bone resorption. J Cell Physiol. 1997;173(3):301-309. [39] COLLINS FL, STONE MD, TURTON J, et al. Oestrogen-deficiency induces bone loss by modulating CD14+ monocyte and CD4+ T cell DR3 expression and serum TL1A levels. BMC Musculoskelet Disord. 2019;20(1):326. [40] KYRGIDIS A, YAVROPOULOU MP, ZIKOS P, et al Changes in peripheral monocyte populations 48-72 hours after subcutaneous denosumab administration in women with osteoporosis. J Musculoskelet Neuronal Interact. 2020;20(3):339-346. [41] CAFIERO C, GIGANTE M, BRUNETTI G, et al. Inflammation induces osteoclast differentiation from peripheral mononuclear cells in chronic kidney disease patients: crosstalk between the immune and bone systems. Nephrol Dial Transplant. 2018;33(1):65-75. [42] REINKE S, GEISSLER S, TAYLOR WR, et al. Terminally differentiated CD8⁺ T cells negatively affect bone regeneration in humans. Sci Transl Med. 2013;5(177): 177ra36. [43] PIETSCHMANN P, GRISAR J, THIEN R, et al. Immune phenotype and intracellular cytokine production of peripheral blood mononuclear cells from postmenopausal patients with osteoporotic fractures. Exp Gerontol. 2001;36(10):1749-1759. [44] SCHLUNDT C, REINKE S, GEISSLER S, et al. Individual Effector/Regulator T Cell Ratios Impact Bone Regeneration. Front Immunol. 2019;10:1954. [45] OPELZ G, DÖHLER B. Association of mismatches for HLA-DR with incidence of posttransplant hip fracture in kidney transplant recipients. Transplantation. 2011;91(1):65-69. [46] BAËHL S, GARNEAU H, LORRAIN D, et al. Alterations in Monocyte Phenotypes and Functions after a Hip Fracture in Elderly Individuals: A 6-Month Longitudinal Study. Gerontology. 2016;62(5):477-490. [47] VIVEIROS MMH, VIVEIROS MEM, SILVA MG, et al. Expression of inflammatory cytokines in mesenchymal stem cells derived from proximal humerus fractures. Stem Cell Investig. 2022;9:3. |
| [1] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei, Zhou Jiatan. Based on Mendelian randomization, the causal relationship between 1400 metabolites and sarcopenia and the correlation analysis of cardiovascular disease were investigated [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-11. |
| [2] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [3] | Jin Jiming, Hao Yangquan, Zhao Rushun, Zhang Yuting, Jiang Yonghong, Xu Peng, Lu Chao. Application of bilateral hip magnetic resonance imaging to predict risk of osteonecrosis of femoral head [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1890-1896. |
| [4] | Zhao Jiyu, Wang Shaowei. Forkhead box transcription factor O1 signaling pathway in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1923-1930. |
| [5] | Dong Tingting, Chen Tianxin, Li Yan, Zhang Sheng, Zhang Lei. Causal relationship between modifiable factors and joint sports injuries [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1953-1962. |
| [6] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [7] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [8] | Zhao Jiacheng, Ren Shiqi, Zhu Qin, Liu Jiajia, Zhu Xiang, Yang Yang. Bioinformatics analysis of potential biomarkers for primary osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1741-1750. |
| [9] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [10] | Li Yueyao, Zhang Min, Yang Jiaju. Cistanoside A mediates p38/MAPK pathway to inhibit osteoclast activity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1144-1151. |
| [11] | Zheng Lin, Jin Wenjun, Luo Shanshan, Huang Rui, Wang Jie, Cheng Yuting, An Zheqing, Xiong Yue, Gong Zipeng, Liao Jian. Eucommia ulmoides promotes alveolar bone formation in ovariectomized rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1159-1167. |
| [12] |
Huang Xiaobin, Ge Jirong, Li Shengqiang, Xie Lihua, Huang Jingwen, He Yanyan, Xue Lipeng.
Mechanisms of different yin nourishing and kidney tonifying methods on osteoclastysis pathway in ovariectomized rats #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1214-1219.
|
| [13] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [14] |
Zhao Wensheng, Li Xiaolin, Peng Changhua, Deng Jia, Sheng Hao, Chen Hongwei, Zhang Chaoju, He Chuan.
Gut microbiota and osteoporotic fractures #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1296-1304.
|
| [15] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||