Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (20): 5341-5348.doi: 10.12307/2026.054
Previous Articles Next Articles
Improved clinical outcomes with fiber posts: personalized design, precise surface treatments, and advanced materials and technologies
Bai Huahui1, Wei Mengting1, Quan Zhiheng1, Yang Lurui1, Hu Yichun1, Fu Jiale2
- 1School of Stomatology, China Medical University, Shenyang 110002, Liaoning Province, China; 2Department of Dental Materials Science, Digital Prosthodontic Center, School and Hospital of Stomatology, China Medical University, Shenyang 110002, Liaoning Province, China
-
Accepted:2025-03-06Online:2026-07-18Published:2025-12-03 -
Contact:Fu Jiale, PhD, Associate chief physician, Master’s supervisor, Department of Dental Materials Science, Digital Prosthodontic Center, School and Hospital of Stomatology, China Medical University, Shenyang 110002, Liaoning Province, China -
About author:Bai Huahui, School of Stomatology, China Medical University, Shenyang 110002, Liaoning Province, China -
Supported by:Innovation and Entrepreneurship Training Program of China Medical University, No. S202410159031 (to WMT, BHH)
CLC Number:
Cite this article
Bai Huahui, Wei Mengting, Quan Zhiheng, Yang Lurui, Hu Yichun, Fu Jiale. Improved clinical outcomes with fiber posts: personalized design, precise surface treatments, and advanced materials and technologies[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(20): 5341-5348.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
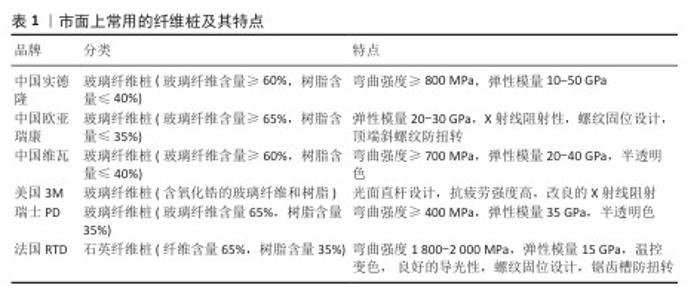
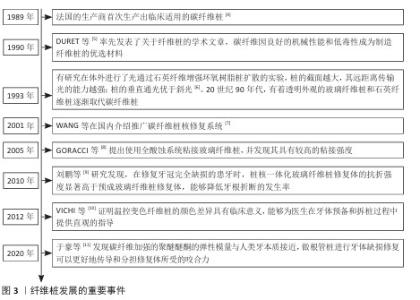
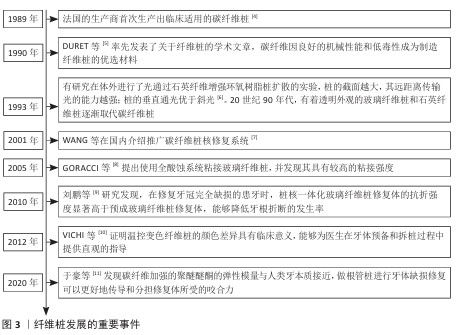
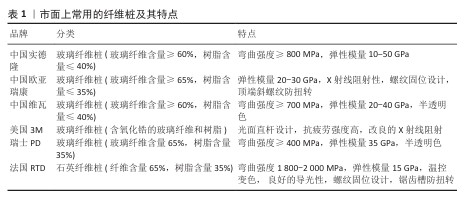
2.2 纤维桩分类及市面上常用的纤维桩 纤维桩是一种由纤维和树脂基质组成的复合材料,其中纤维决定了桩的承载能力,基质确保复合结构的完整性[12]。为提升纤维与树脂基质之间的粘接力,常需用硅烷偶联剂进行处理,从而优化纤维桩的机械性能。纤维桩根据纤维成分主要分为碳纤维桩、玻璃纤维桩、石英纤维桩等。 碳纤维桩是将碳含量高于90%的碳纤维注入树脂基质中制成。相较于传统金属桩,碳纤维桩的力学性能更好,弹性模量与牙本质接近,抗疲劳性和耐腐蚀性得到改善。现代的碳纤维桩主体一般都是白色或乳白色,在美学性能上有所改进。玻璃纤维桩是一种性能较好的非金属纤维桩,所用的玻璃纤维主要由非晶态二氧化硅及氧化铝、氧化钙、氧化硼、氧化镁、氧化钠等多种化合物混合而成,其中二氧化硅含量最多。玻璃纤维桩具有适中的弹性模量,能够精准模拟牙本质的机械性能,减少根折风险;此外,玻璃纤维桩还具备较高的弯曲强度和拉伸强度,是目前牙科修复中最为广泛应用的纤维桩。石英纤维桩所用的石英纤维是由纯结晶态的二氧化硅构成,可以提供更好的美学效果。石英纤维桩具有极高的抗疲劳强度,可确保修复效果的持久性;同时,它出色的光传导作用有助于桩核植入根管后树脂的固化[13]。市面上常用的纤维桩及其特点如表1所示。 "
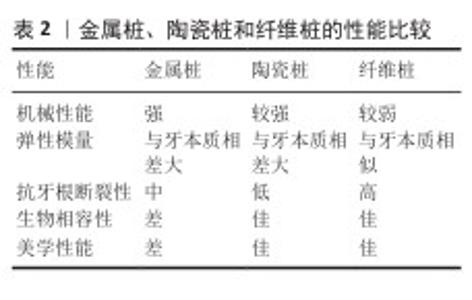
2.3 纤维桩的临床应用及注意事项 2.3.1 金属桩、陶瓷桩与纤维桩的对比 根管桩根据材料的不同分为金属桩、陶瓷桩和纤维桩,表2对比了它们的性能。目前临床应用较多的为纤维桩与金属桩,二者各有优势与局限性,在失败率方面并无显著差异,因此,医生应根据患者的实际情况进行选择[14]。陶瓷桩虽然具有较好的美学效果和生物相容性,但价格较高、易导致根折且难以修复,限制了其在临床中的应用[15]。 金属桩主要由各类合金材料组成,可分为铸造金属桩和预成金属桩。传统上铸造金属桩用于修复牙髓治疗后的牙齿,尤其适用于牙本质肩领高度不足或需要改变冠根角度的情况。预成金属桩是半成品,便于使用,能够缩短患者就诊时间。尽管金属桩的强度高且物理性能好,但弹性模量(金合金为200 GPa[16],钴铬合金为180-210 GPa[17],钛合金为110 GPa[17],镍铬合金为206 GPa[18])远高于牙本质(约18.6 GPa[19]),可能导致牙根内应力集中区域发生折裂[20]。金属材料还会产生微电流引起腐蚀和溶解,降低粘接效果,其色泽也可能会透过外部的冠修复体而影响美观性[21]。 陶瓷桩主要为氧化锆桩,氧化锆因具有较高的机械强度、化学稳定性及与牙齿相似的颜色而被广泛应用于口腔修复领域。AWAD等[22]利用计算机辅助设计与计算机辅助制造技术开发了铣削单个氧化锆桩核的工艺,该技术可以制作出美观而坚硬的根管桩,有效恢复根管健康。研究显示氧化锆桩是铸造金属桩在前牙美学修复中的可行替代品[23-24],然而其高弹性模量(210 GPa[17])可能会影响牙根的应力分布,增加断裂风险[20]。 与金属桩和陶瓷桩相比,纤维桩在临床应用中的优势显著,具有抗生化降解、美观性好、导电性低、拉伸强度高且弹性模量接近牙本质等优点[25-26]。纤维桩不含金属元素,对牙龈组织的刺激较小,能降低炎性因子水平,并且能够减少牙折、脱粘接和继发龋的发生[27]。纤维桩本身的抗折断性能较差,若发生桩折断可进行拆桩后的再修复。研究发现,纤维桩和金属桩修复根管治疗牙的生存率相似,并且纤维桩在抗折性能上与钛合金桩无显著差异[28-29]。研究指出纤维桩的远期生存率高达92.8%,表现出长期稳定性[21]。玻璃纤维桩全冠修复能够有效改善后牙严重缺损患者的咀嚼功能,提高美学效果,降低牙周炎症反应及不良反应发生率,提高临床疗效[30]。 临床工作中选用何种类型的纤维桩需要综合考虑纤维桩的性能及患者需求。碳纤维桩适合后牙修复,不推荐用于对美观要求较高的前牙。玻璃纤维桩和石英纤维桩的美学性能好,适用多数牙齿的修复。石英纤维桩的耐疲劳性能和弯曲强度更有优势。在临床应用中,选择合适的纤维桩还需要考虑桩长度、直径、桩形态与根管形态的适应性、桩的形状与表面结构等因素。理想的桩长度应在保证根尖封闭的前提下达到根长的2/3-3/4,然而随着粘接材料性能的提升,当遇到短根或弯曲根的牙齿,纤维桩的长度不能达到剩余根的2/3时,可以考虑制备剩余根的1/2[31]。单根患牙桩的直径应为牙根直径的1/4-1/3,不宜超过1/2。研究表明,对于椭圆形根管,椭圆形纤维桩不能显著增加桩的固位力,但是通过增加辅桩可以提高桩的固位力和牙齿的抗折能力[32]。 2.3.2 牙本质肩领的临床意义 为确保冠修复体稳固有效,其边缘应覆盖缺损区边缘的健康牙本质,保留至少1.5 mm的牙本质作为牙本质肩领。牙本质肩领可以形成箍效应,进而增强固位和抗力。箍效应能够降低纤维桩对牙根结构的楔入力,从而减少粘接界面的应力,降低咀嚼失效的风险,并且可以改善应力分布,抵抗部分侧向力,从而提高牙齿的抗折能力[33]。原则上牙本质肩领高度不小于1.5-2.0 mm,并且厚度不小于1.0 mm。也有研究表明,剩余牙齿结构的高度为1.0 mm就足够满足修复需求[34],而当肩领的高度达到2.0 mm时,其抗折性能表现尤为显著[33,35]。当剩余牙体组织较少时,为预备出牙本质肩领而向龈下预备过多可能破坏生物学宽度,可通过正畸牵引或牙冠延长术来获得至少1.0 mm的肩领高度[36]。有学者提出牙本质肩领的高度与冠根比相匹配可优化修复效果,实验显示,肩领高度为1.92 mm且冠根比为0.9-0.92时牙齿的抗断裂强度达到最大[37]。 牙齿的机械强度和预后受剩余牙本质壁的数量和位置影响[38]。连续肩领能够增强根管治疗牙的抗折能力,若剩余牙本质壁足够厚实,即使肩领不完整,也可显著提升牙齿的抗折性能,并且非均匀肩领优于无肩领[36]。肩领的位置对于不同牙位的抗折性能有不同影响,例如:上颌中切牙的腭侧壁对提高抗折能力至关重要[39]。三维有限元分析显示,下颌切牙保留2.0 mm完整肩领或颊侧肩领时的抗折强度较大,保留舌侧肩领和近中侧肩领时的抗折强度次之,无肩领时抗折强度最小[40]。研究发现前磨牙的抗折强度主要受缺损牙壁数的影响,与肩领高度无关[41]。上颌前磨牙在保留颊侧肩领时抗折强度更佳[42]。上颌尖牙和下颌前磨牙的实验表明,缺少近中肩领的牙齿受影响最小,而缺少舌侧肩领的牙齿抗折强度会显著下降[43]。 牙本质肩领的数量指导治疗方案的选择。轻度牙体缺损时推荐选择纤维桩,牙体缺损较重时推荐选择铸造金属桩修复,其中贵金属铸造桩更佳。四壁完整患牙建议直接全冠修复;三壁完整患牙应用纤维桩能提高修复成功率[44];金属铸造桩修复能够为二壁完整患牙提高更强的抗断裂能力[45];一壁完整患牙由于颈部抗力较差,推荐使用铸造金属桩修复[45];零壁且无法通过冠延长术等方法获得牙本质壁的患牙,远期预后极差,建议拔除[44]。研究显示,根管治疗后冠状面缺损不超过2壁的牙中,纤维桩的中期(3-7年)生存率较高[46]。 "
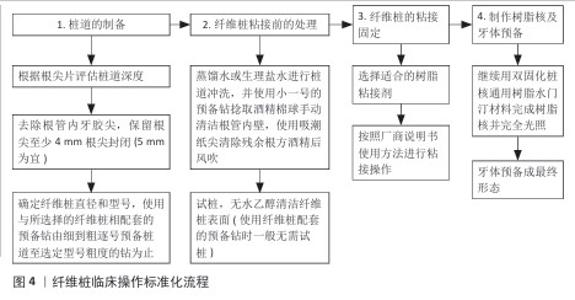
2.3.3 临床适应证与禁忌证 适应证:所有适合桩核冠修复的残根和残冠,包括牙冠中度以上缺损、断面达龈下但能够通过冠延长术或牵引术暴露出断面以下至少1.5 mm根面高度的患牙,都可使用纤维桩进行修复。患牙需要经过完善的根管治疗,原有根尖周炎症得到控制,在根管治疗至少7 d后可以对患牙行纤维桩修复。纤维桩在后牙牙体缺损修复中的成功率较高、并发症较少,可以降低不可修复性根折的发生率,有利于进一步修复[47]。研究表明,对于伴龈下骨折的前牙,采用冠延长术并用玻璃纤维桩、复合树脂核和全瓷冠修复可以满足美学需求,并且能够取得良好的长期预后[48]。 禁忌证:①牙根长度不足的患牙:纤维桩的长度过短会影响其与根管壁之间的摩擦力及与水门汀和粘接剂之间的粘接力,进而影响纤维桩的固位[24]。研究表明,7.5 mm纤维桩比5.0 mm纤维桩更能增强下颌前磨牙的抗折性能,而过短的纤维桩易导致牙齿折断[38]。因此,当牙根过短时不宜采用纤维桩修复。②根管弯曲、细小的患牙:根管狭窄和弯曲使得预备器械难以有效扩大根管,影响桩道尺寸,可能导致去除过多的健康牙本质,增加牙根折断风险。研究发现,上颌中切牙经纤维桩修复后纤细型牙齿的应力值最大[49]。使用不同桩核系统修复薄壁根管时,纤维桩修复的患牙在抗折性能上显著不及铸造金属桩所达到的修复效果[50]。③不具备牙本质肩领且也无法通过牙周手术或正畸牵引等方法获得牙本质肩领的患牙:有研究显示,剩余健全牙本质肩领小于1.0 mm时,铸造桩核的修复效果更优[36]。有研究表明,不具备牙本质肩领的患牙远期预后极差,建议拔除[44]。④咬合间隙不足的患牙:牙齿咬合过紧时,修复体必须极其纤薄。若采用纤维桩核,可能会因桩核系统的机械强度不足以承受咬合力增加桩体折断的风险,最终可能引发冠修复体的脱落和修复失败等问题[51]。 2.3.4 纤维桩的临床操作标准化流程 长期随访发现,因粘接操作具有一定的技术敏感性,纤维桩存在粘接失败风险,临床规范化操作具有重要意义。纤维桩临床操作标准化流程如图4。另以RTD 温控螺纹石英纤维桩为例(MACRO-LOCK POST ILLUSION X-RO),结合临床实际病例总结操作步骤如下,供广大临床医生借鉴参考。去净暂封物,暴露根管口预备区域并做好隔湿。根据根尖片评估桩道预备深度,使用启动钻或P钻去除根管内牙胶尖,在根尖部位至少保留4.0 mm根尖封闭,弯曲根管除外。根据牙齿解剖学状况并参考根尖片确定纤维桩的直径型号,选择合适型号的纤维桩。注意多根管患牙为避免过多破坏根壁,可选择直径较小的纤维桩,桩周围根管壁厚度应≥1.0 mm。使用与所选择的纤维桩相配套的修整钻头由细到粗逐号预备桩道至选定型号粗度的钻为止,预备过程中持续冷水降温修整钻。酒精棉捻擦拭根管,去除根管内壁上的牙胶碎屑;蒸馏水或生理盐水冲洗根管后使用吸潮纸尖吸净水分,但保持轻微湿润。使用纤维桩配套的修整钻进行桩道预备一般无需试桩;如需要试桩,试桩后建议采用无水乙醇清洁纤维桩表面,风吹干燥备用。在根管内壁及牙面涂布自酸蚀通用型粘接剂2遍,气枪吹5 s后使用纸尖吸除根尖区多余的粘接剂,光固化灯接近根管口位置垂直光照20 s。在纤维桩表面涂布单层自酸蚀通用型粘接剂,气枪吹5 s,光照固化10 s。 将双固化桩核通用树脂水门汀注入根管内,立即快速地在纤维桩表面涂布一层水门汀材料,插入纤维桩,光固化灯从根管口向,颊(唇),腭(舌)向分别照射40 s,使水门汀充分固化。继续用双固化桩核通用树脂水门汀材料完成树脂核并完全光照。牙体预备形成最终形态。 "

2.5 纤维桩现存的问题及解决方案 2.5.1 纤维桩与根管不密合 纤维桩与根管不密合通常由于根管预备不当或特殊形状(如喇叭形)导致桩道预备的直径、形状与纤维桩不匹配,以及根管内残留物未被彻底清除。利用超声洁牙机彻底清除根管内残留物,可提高纤维桩与根管的密合度,增强修复体的稳定性和长期效果[55]。有研究显示预制纤维桩与根尖段和中段根管的贴合良好,与颈段贴合较差[56]。计算机辅助设计与制造纤维桩与传统铸造桩核的内密合度和抗折性相似,均好于预制纤维桩[57]。研究表明,在根管治疗中使用数字化导板可以引导根管方向,避免偏移,提高纤维桩与根管的密合性;如果能从锥形束CT扫描中提取根管形态,在桩道预备之前定制桩核,能够提高修复效率[58]。另外,计算机辅助设计与制造一体化纤维桩核与根管形态高度一致,应力分布更加均匀,尤其适应喇叭口形态[59]。 计算机辅助设计与制造纤维桩核具有加固无髓牙的潜力,修复后的牙即使折断后仍可修复[60]。计算机辅助设计与制造技术以一种可预测和简化的方式制造桩核修复体,但是需要进一步研究相应的参数(如铣削策略、桩的几何形状、长度和宽度)以生产出性能更佳的纤维桩,同时需要更多的体外和临床研究来明确合适的临床方案和评估各种材料的适用性。 2.5.2 纤维桩松动、脱落 研究表明纤维桩的寿命主要受脱粘接影响,长期存在的微渗漏可使细菌及其毒素侵入,刺激巨噬细胞、淋巴细胞等引发慢性炎症反应,导致纤维桩周围组织红肿、疼痛,影响修复效果。合理使用表面处理和粘接技术有助于延长纤维桩的使用寿命[29]。唾液污染会降低纤维桩与复合树脂的粘接强度,粘接前应彻底清洗消毒桩道,对试桩后纤维桩表面进行酒精清洁[61]。研究发现,17%乙二胺四乙酸和超声冲洗可提高树脂水门汀与牙本质边缘的密合度[62]。在另一项研究中,次氯酸钠与乙醇酸联用冲洗桩道不会对粘接强度产生负面影响,并且比乙二胺四乙酸联用的效果更好[63]。喷砂、硅烷化、过氧化氢蚀刻等处理方法可以增强纤维桩与粘接剂的粘接强度,降低因根管松动、脱落而导致的临床失败的风险[64]。有学者研究不同表面处理方式对粘接效果的影响,使用掺铒钇铝石榴石晶体激光处理纤维桩,可使纤维桩表面粗糙度增大,并有一定程度的环氧基去除作用;使用掺铒钇铝石榴石晶体激光联合照射根管和纤维桩,可显著增强粘接强度,并且优于单一方法处理的纤维桩或根管[65-66]。有研究表明,粘接体系(Clearfil SE - CSE和Single Bond Universal-SBU)联合新型旋转刷使用可提高纤维桩与根面牙本质的粘接强度,使用双固化自粘结树脂水门汀粘接时,在混合后延迟120 s进行光活化的粘接强度最高[67]。解剖个性化纤维桩能够获得更薄的粘接剂层,有利于增强粘接剂与牙本质的粘接强度[68]。 2.5.3 纤维桩折断 纤维桩折断的问题通常源于纤维桩选择不当及牙体组织支持能力不足。尽管纤维桩具有良好的弹性模量和美学性能,但其弯曲强度不足可能导致桩折断。新材料和新工艺的应用将显著提升纤维桩的性能。相关研究表明,通过玻璃纤维和热塑性聚丙烯树脂纤维编织技术所制造的纯玻璃纤维核心桩结构和较高热塑性聚丙烯/玻璃纤维比率的桩结构与商业可用的纤维桩类型相当,但具有更高的抗弯强度[69]。有研究显示聚醚醚酮具有良好的力学性能,较传统材料具有更好的应力分布,对基牙具有较好的保护作用[70]。聚醚醚酮的刚度不足可以通过纤维增强来改善,如玻璃纤维增强聚醚醚酮复合材料具有良好的力学性能、生物安全性,具有作为桩核材料的巨大潜力[71]。关于聚醚醚酮的粘接实验显示,脱粘接表面仅残留少量树脂粘接剂,其惰性表面使得粘接较为困难,需要进一步探究适当的表面处理方式和粘接系统以满足修复的粘接需求[72]。另外,聚醚醚酮的使用寿命还需临床试验进一步评估。 2.5.4 纤维桩的拆除 经过桩核冠修复的根管治疗牙在出现纤维桩折断或根尖周疾病时,需要拆除纤维桩,在此过程中剩余牙体组织的完整性对于长期修复效果至关重要。拆桩时应精确控制磨除方向和力度,以避免损伤健康牙本质、产生微裂纹和防止根管侧穿。目前,临床上常用的拆桩方法包括纤维桩拆除套装法、超声法、数字化导板引导法及动态导航法[73-74]。其中,纤维桩拆除套装法使用特定的钻头从纤维桩中心磨除纤维桩[75]。超声法通过振动传递能量至粘接剂层引发粘接剂内的微断裂,破坏粘接效果,从而实现桩核的取出,尽管拆桩效果优于纤维桩拆除套装法,但有研究表明此法操作时间较长且可能会降低根管的抗折能力[76]。数字化导板引导法主要适用于可操作空间较大的前牙区,比传统技术更快更准确,可减少牙体组织的磨除量和根管壁侧穿的风险[77]。据报道,借助数字化导板可以在拆桩术前进行预设计并制作钛桩核和牙冠,实现断裂纤维桩的取出和即刻修复,有效减少患者的就诊次数、提升治疗效率[78]。动态导航法具有实时可视化的优势,能够高效、精准、微创地去除纤维桩,并可应用于咬合间隙较小的区域[79]。 近年来,铒激光拆除法作为一种新型的拆桩方法受到关注,该方法通过定向激活水分子和单体使水分子产生爆裂,进而去除水分子周围的硬组织[80-81]。体外研究表明,铒激光拆除法能够缩短拆桩时间(仅为超声法的55%),并减少微裂纹的形成[81];在另一项研究中,铒激光法的拆桩速度比超声法快5倍,引起的根面升温更低[82],然而该方法在临床应用中的效果仍需进一步验证。 "

| [1] BHUVA B, GIOVARRUSCIO M, RAHIM N, et al. The restoration of root filled teeth: a review of the clinical literature. Int Endod J. 2021;54(4):509-535. [2] PRAKASH J, GOLGERI MS, HALEEM S, et al. A Comparative Study of Success Rates of Post and Core Treated Anterior and Posterior Teeth Using Cast Metal Posts. Cureus. 2022;14(10): e30735. [3] YADAV M, GREWAL MS, ARYA A, et al. Comparison of fracture resistance of endodontically treated maxillary first premolar with mesio-occlusal-distal access restored with composite resin, fiber post, and prefabricated metal posts restored with/without full-coverage metal crowns. J Conserv Dent. 2021; 24(6):594-598. [4] LAMICHHANE A, XU C, ZHANG FQ. Dental fiber-post resin base material: a review. J Adv Prosthodont. 2014;6(1):60. [5] DURET B, REYNAUD M, DURET F. New concept of coronoradicular reconstruction: the composipost (1). Chir Dent Fr. 1990;60(540): 131-141 contd. [6] ASMUSSEN E, PEUTZFELDT A, HEITMANN T. Stiffness, elastic limit, and strength of newer types of endodontic posts. J Dent. 1999; 27(4):275-278. [7] 张相皥,王新知.碳纤维桩的性能及应用[J].口腔颌面修复学杂志,2002,3(4):255-258. [8] GORACCI C, SADEK F, FABIANELLI A, et al. Evaluation of the adhesion of fiber posts to intraradicular dentin. Oper Dent. 2005;30(5): 627-635. [9] 刘鹏,李亚南,姜慧,等.CAD/CAM一体化玻璃纤维桩核抗折力的体外实验研究[J].北京口腔医学,2010,18(2):90-93. [10] VICHI A, SCHIAVETTI R, PACIFICI E, et al. Masking of temperature-induced color changes in a thermo-sensitive fiber post. Am J Dent. 2012;25(2):123-128. [11] 于豪,白石柱,冯志宏,等.聚醚醚酮用于桩核冠修复的三维有限元分析[J].实用口腔医学杂志,2020,36(1):5-9. [12] MIURA H, YOSHII S, FUJIMOTO M, et al. Effects of Both Fiber Post/Core Resin Construction System and Root Canal Sealer on the Material Interface in Deep Areas of Root Canal. Materials (Basel). 2021;14(4):982. [13] CP PASMADJIAN A, N DIÓGENES A, P PERIN C, et al. The luminous transmittance of the quartz-glass fiber posts is superior to glass fiber posts. Acta Odontol Latinoam. 2023; 36(2):106-111. [14] MARTINS MD, JUNQUEIRA RB, DE CARVALHO RF, et al. Is a fiber post better than a metal post for the restoration of endodontically treated teeth? a systematic review and meta-analysis. J Dent. 2021;112:103750. [15] DIREK A, TEKIN S, KHURSHID Z. Fracture strength of cad-cam milled polyetheretherketone (PEEK) post-cores vs conventional post-cores; an in vitro study. PeerJ. 2024;12:e18012. [16] MONTANARI R, VARONE A. Processing–Structure–Property Relationships in Metals. Metals. 2019;9(8):907. [17] RAHMITASARI F, ISHIDA Y, KURAHASHI K, et al. PEEK with Reinforced Materials and Modifications for Dental Implant Applications. Dent J (Basel). 2017;5(4):35. [18] MAPAR A, TAHERI-NASSAJ N, SHEN J, et al. Finite ccndibular Second Molar Under Percussion Conditions. J Med Biol Eng. 2022;42:1-11. [19] HASHEMI S, BAGHAEI K, FATHI A, et al. Stress Analysis of Endodontically Treated Tooth-Implant Different Connectors Designs in Maxillary Posterior Region: A Finite Element Analysis. Eur J Dent. 2024;18(2):587-597. [20] KHARBOUTLY N AD, ALLAF M, KANOUT S. Three-Dimensional Finite Element Study of Endodontically Treated Maxillary Central Incisors Restored Using Different Post and Crown Materials. Cureus. 2023;15(1):e33778. [21] TSINTSADZE N, MARGVELASHVILI-MALAMENT M, NATTO ZS, et al. Comparing survival rates of endodontically treated teeth restored either with glass-fiber-reinforced or metal posts: A systematic review and meta-analyses. J Prosthet Dent. 2024;131(4):567-578. [22] AWAD MA, MARGHALANI TY. Fabrication of a custom-made ceramic post and core using CAD-CAM technology. J Prosthet Dent. 2007;98(2):161-162. [23] PALEPWAD AB, KULKARNI RS. In vitro fracture resistance of zirconia, glass-fiber, and cast metal posts with different lengths. J Indian Prosthodont Soc. 2020;20(2):202-207. [24] KOLE S, ERGUN G. Bond strength of various post-core restorations with different lengths and diameters following cycle loading. J Mech Behav Biomed Mater. 2023;142:105804. [25] ALSHABIB A, ABID ALTHAQAFI K, ALMOHARIB HS, et al. Dental Fiber-Post Systems: An In-Depth Review of Their Evolution, Current Practice and Future Directions. Bioengineering. 2023;10(5):551. [26] MADFA AA. Effect of Dental Glass Fiber Posts on Root Stresses and Fracture Behavior of Endodontically Treated Maxillary Central Incisors: A Finite Element Analysis Study. Cureus. 2023;15(8):e43056. [27] JUREMA ALB, FILGUEIRAS AT, SANTOS KA, et al. Effect of intraradicular fiber post on the fracture resistance of endodontically treated and restored anterior teeth: A systematic review and meta-analysis. J Prosthet Dent. 2022;128(1):13-24. [28] ALHAJJ MN, QI CH, SAYED ME, et al. Fracture resistance of titanium and fiber dental posts: a systematic review and meta-analysis. J Prosthodont. 2022;31(5):374-384. [29] DE MORAIS DC, BUTLER S, SANTOS MJMC. Current Insights on Fiber Posts: A Narrative Review of Laboratory and Clinical Studies. Dent J. 2023;11(10):236. [30] 胡梦甜,潘树矿,丁凤,等.玻璃纤维桩全冠修复在后牙严重牙体缺损中应用效果[J].临床军医杂志,2024,52(8):847-849,853. [31] LIN J, MATINLINNA JP, SHINYA A, et al. Effect of fiber post length and abutment height on fracture resistance of endodontically treated premolars prepared for zirconia crowns. Odontology. 2018;106(2):215-222. [32] SPICCIARELLI V, MARRUGANTI C, DI MATTEO C, et al. Influence of single post, oval, and multi-post restorative techniques and amount of residual tooth substance on fracture strength of endodontically treated maxillary premolars. J Oral Sci. 2020;63(1):70-74. [33] GRÉ C, LISE D, RAMOS R, et al. Better glass-fiber post preservation in teeth with ferrule when subjected to chewing. Oper Dent. 2021; 46(4):419-427. [34] MA PS, NICHOLLS JI, JUNGE T, et al. Load fatigue of teeth with different ferrule lengths, restored with fiber posts, composite resin cores, and all-ceramic crowns. The Journal of Prosthet Dent. 2009;102(4):229-234. [35] KUMAR S, VISWANATHAN M, RAJKUMAR K, et al. Comparative study on fracture resistance of endodontically treated tooth in relation to variable ferrule heights using custom-made and prefabricated post and core: an in vitro study. J. Pharm. Bioallied Sci. 2020;12(5):554. [36] ASSIRI A YK, SAAFI J, AL-MOALEEM MM, et al. Ferrule effect and its importance in restorative dentistry: a literature review. J Popul Ther Clin Pharmacol. 2022;29(4):e69-e82. [37] MENG Q, CHEN Y, NI K, et al. The effect of different ferrule heights and crown-to-root ratios on fracture resistance of endodontically-treated mandibular premolars restored with fiber post or cast metal post system: an in vitro study. BMC Oral Health. 2023;23(1):360. [38] SAMRAN A, MOURSHED B, AHMED MA, et al. Influence of post length, post material, and substance loss on the fracture resistance of endodontically treated teeth: a laboratory study. Int J Prosthodont. 2023;36(6):712-721. [39] ZHANG YY, PENG MD, WANG YN, et al. The effects of ferrule configuration on the anti-fracture ability of fiber post-restored teeth. J Dent. 2015;43(1):117-125. [40] 李洋,王时越,祁麟.牙本质肩领位置对下颌切牙抗折强度影响的研究[J].口腔医学研究,2021,37(10):945-950. [41] ZAHRAN M, ABDERBWIH D, MANDOURAH H, et al. Effect of ferrule height and distribution on the fracture resistance of endodontically treated premolars. Niger J Clin Pract. 2021; 24(4):505-510. [42] KOOSHA S, JEBELIZADEH MS, MOSTAFAVI AS. Effect of Ferrule Location on Fracture Resistance of Maxillary Premolars: An In Vitro Study. Int J Dent. 2023;2023:9513804. [43] HARALUR S, ALALYANI A, ALMUTIQ M, et al. Effect of inadequate ferrule segment location on fracture resistance of endodontically treated teeth. Indian J Dent Res. 2018;29(2):206. [44] CAGIDIACO MC, GARCÍA-GODOY F, VICHI A, et al. Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am J Dent. 2008; 21(3):179-184. [45] 闫慧,张燕,赵彬.两种桩核系统修复对不同程度缺损磨牙抗折性能影响研究[J].中国实用口腔科杂志,2011,4(3):147-150. [46] WANG X, SHU X, ZHANG Y, et al. Evaluation of fiber posts vs metal posts for restoring severely damaged endodontically treated teeth: a systematic review and meta-analysis. Quintessence Int. 2019;50(1):8-20. [47] SELVARAJ H, KRITHIKADATTA J, SHRIVASTAVA D, et al. Systematic review fracture resistance of endodontically treated posterior teeth restored with fiber reinforced composites- a systematic review. BMC Oral Health. 2023;23(1):566. [48] YU H, ZHU H. The management of a complicated crown-root fracture incorporating modified crown-lengthening surgery. Br Dent J. 2021;230(4):217-222. [49] SANTOS PANTALEÓN D, TRIBST J PM, GARCÍA-GODOY F. Influence of size-anatomy of the maxillary central incisor on the biomechanical performance of post-and-core restoration with different ferrule heights. J Adv Prosthodont. 2024;16(2):77. [50] IEMSAENGCHAIRAT R, AKSORNMUANG J. Fracture resistance of thin wall endodontically treated teeth without ferrules restored with various techniques. J Esthet Restor Dent. 2022; 34(4):670-679. [51] LIN J, LIN Z, ZHENG Z. Effect of different restorative crown design and materials on stress distribution in endodontically treated molars: a finite element analysis study. BMC Oral Health. 2020;20(1):226. [52] 段海英,高少怀.3种材料纤维桩细胞毒性评价[J].口腔医学研究,2012,28(6):516-518. [53] 肖严.玻璃纤维桩与金属桩核修复外力导致牙体损伤的比较[J].中国组织工程研究, 2019,23(26):4165-4169. [54] 秦明群,莫弼凡,黄甲清.玻璃纤维桩在严重缺损牙齿修复中的应用[J].中国组织工程研究与临床康复,2007,11(44):8957-8959. [55] PEÑA BENGOA F, MAGASICH ARZE MC, MACCHIAVELLO NOGUERA C, et al. Effect of ultrasonic cleaning on the bond strength of fiber posts in oval canals filled with a premixed bioceramic root canal sealer. Restor Dent Endod. 2020;45(2):e19. [56] MING X, ZHANG Z, XIE W, et al. Internal adaptation and mechanical properties of CAD/CAM glass fiber post-cores in molars: An in vitro study. J Dent. 2023;138:104685. [57] OLIVEIRA G, MACHRY R, CADORE-RODRIGUES A, et al. Fatigue Properties of Weakened and Non-weakened Roots Restored with CAD-CAM Milled Fiber Post, Prefabricated Fiber Post, or Cast Metal Post. Oper Dent. 2022;47(6):658-669. [58] LIN P, XU Z, LUO Y, et al. A digital technique for a prefabricated custom post-and-core restoration. J oProsthet Dent. 2023;130(3): 278-283. [59] GAMA M, BALBINOT GS, FERREIRA GC, et al. CAD/CAM Milled Glass Fiber Posts: Adaptation and Mechanical Behavior in Flared Root Canals. Oper Dent. 2021;46(4): 438-447. [60] SUZAKI N, YAMAGUCHI S, NAMBU E, et al. Fabricated CAD/CAM post-core using glass fiber-reinforced resin shows innovative potential in restoring pulpless teeth. Mater (Basel Switz.). 2021;14(20):6199. [61] IMAI D, MINE A, EZAKI R, et al. Does the bonding effectiveness of a fiber post/resin composite benefit from mechanical or chemical treatment? Seven methods for saliva-contaminated surfaces. J Prosthodont Res. 2022;66(2):288-295. [62] BOGGIAN LC, SILVA AV, SANTOS GR, et al. Effect of intra-radicular cleaning protocols after post-space preparation on marginal adaptation of a luting agent to root dentin. J Oral Sci. 2023;65(2):81-86. [63] YANIK D, TURKER N. Glycolic acid on push-out bond strength of fiber post and smear removal: an in vitro study: Odontology. 2024; 112(3):739-750. [64] SOUZA JCM, FERNANDES V, CORREIA A, et al. Surface modification of glass fiber-reinforced composite posts to enhance their bond strength to resin-matrix cements: an integrative review. Clin Oral Investig. 2022; 26(1):95-107. [65] DENG Z, HUANG Z, PING L, et al. The combined treatment of fiber post and root canal by the Er:YAG laser enhances the bond strength of composite reconstruction. Lasers Med Sci. 2023;38(1):146. [66] ABDUL HADI AHMED R, MOHAMMED ALI HUSSEIN B. Effect of Laser Treatment of Root Dentine on Retention of Dental Fiber Post in Endodontically Treated Teeth: An In Vitro Study. J Lasers Med Sci. 2024;15:e28. [67] COMBA A, BALDI A, JUZIKIS E, et al. Does Curing Delay Affect the Bond Strength of Fiber Post with Self-Adhesive Cements? Int J Prosthodont. 2023;36(5):595-602. [68] LEANDRIN TP, FERNÁNDEZ E, LIMA RO, et al. Customized Fiber Post Improves the Bond Strength and Dentinal Penetrability of Resin Cementation System to Root Dentin. Oper Dent. 2022;47(1):E22-E34. [69] ABDELKADER E, CORTES CORTES J, BOTELLA C, et al. Flexural Strength of Dental Fiber Composite Post Manufactured with a Novel Approach. Materials. 2022;15(9):3370. [70] WANG B, HUANG M, DANG P, et al. PEEK in Fixed Dental Prostheses: Application and Adhesion Improvement. Polymers (Basel). 2022;14(12):2323. [71] ZHAO T, JIANG Z, GE Y, et al. Mechanical properties, biosafety, and shearing bonding strength of glass fiber-reinforced PEEK composites used as post-core materials. J Mech Behav Biomed Mater. 2023;145:106047. [72] BENLI M, EKER GÜMÜŞ B, KAHRAMAN Y, et al. Surface characterization and bonding properties of milled polyetheretherketone dental posts. Odontology. 2020;108(4): 596-606. [73] 陈文彬,孟洋,王芳萍,等.纤维桩拆除方法的研究进展[J].中国实用口腔科杂志, 2023,16(4):498-502. [74] BARDALES-ALCOCER J, RAMÍREZ-SALOMÓN M, VEGA-LIZAMA E, et al. Endodontic retreatment using dynamic navigation: A case report. J Endodont. 2021;47(6): 1007-1013. [75] HAUPT F, RIGGERS I, KONIETSCHKE F, et al. Effectiveness of different fiber post removal techniques and their influence on dentinal microcrack formation. Clin Oral Invest. 2022; 26(4):3679-3685. [76] ABELLA SANS F, ALATIYA ZT, VAL GG, et al. A laboratory study comparing the static navigation technique using a bur with a conventional freehand technique using ultrasonic tips for the removal of fibre posts. Int Endod J. 2024;57(3):355-368. [77] PEREZ C, SAYEH A, ETIENNE O, et al. Microguided endodontics: accuracy evaluation for access through intraroot fibre‐post. Aust Endod J. 2021;47(3):592-598. [78] LIU R, XIE C, SUN M, et al. Guided removal of a fractured fiber post and immediate restoration with a digitally prefabricated titanium post-and-core and zirconia crown: A clinical report. J Prosthet Dent. 2023; 129(5):684-689. [79] JANABI A, TORDIK PA, GRIFFIN IL, et al. Accuracy and efficiency of 3-dimensional dynamic navigation system for removal of fiber post from root canal–treated teeth. J Endodont. 2021;47(9):1453-1460. [80] PAPOULIDOU I, DIONYSOPOULOS D, MOUROUZIS P, et al. Evaluation of Er,Cr:YSGG laser technique for fiber post removal of endodontically treated teeth using micro-computed tomography. Microsc Res Tech. 2023;86(7):803-812. [81] ÖZCAN N, UTAR M, ÇULHAOĞLU AK, et al. Effect of er:YAG laser on removal of fibre posts from root canal. Aust Endodontic J. 2023; 49(S1):294-300. [82] DEEB JG, GRZECH-LEŚNIAK K, WEAVER C, et al. Retrieval of glass fiber post using er:YAG laser and conventional endodontic ultrasonic method: an in vitro study. J Prosthodont. 2019; 28(9):1024-1028. |
| [1] | Kang Zirui, Wu Yang, Song Hailong, Yang Qiaoyun, Zang Lixiang, Xu Dongliang. Finite element analysis of implants with different crown-to-implant ratios under different bone conditions [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 319-328. |
| [2] | Zhang Qiya, Tong Yixiang, Yang Shijiao, Zhang Yumeng, Deng Ling, Wu Wei, Xie Yao, Liao Jian, Mao Ling. In vitro biocompatibility of graded glass infiltrated ultra-translucent zirconia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 443-450. |
| [3] | Tan Fengyi, Xie Jiamin, Pan Zhenfeng, Zhang Xinxu, Zheng Zetai, Zeng Zhiying, Zhou Yanfang. Effect and mechanism of collagen combined with microneedles in treatment of skin photoaging [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 451-458. |
| [4] | Wang Zhuo, Sun Panpan, Cheng Huanzhi, Cao Tingting. Application of chitosan in repair and regeneration of oral hard and soft tissues [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 459-468. |
| [5] | Tang Yiyang, Xiao Yuxin, Sun Hening, Li Chunxiao, Zhang Yutong, Fu Jiale. Key points of zirconia all-ceramic restoration materials in clinical application [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(14): 3717-3725. |
| [6] | Du Huijing, Chen Shichun, Liu Yinuo, Yang Yutong, Wang Ruohan, Yang Xueying, Ma Zhe, Yan Rui. Application of quantitative light-induced fluorescence technology in diagnosis of oral diseases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(14): 3736-3744. |
| [7] | Jin Hui, Chen Hui. Preparation and mechanical properties of zirconia ceramic composites for stomatology [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(14): 3548-3556. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||