Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (6): 1296-1304.doi: 10.12307/2025.311
Previous Articles Next Articles
Gut microbiota and osteoporotic fractures #br#
#br#
Zhao Wensheng1, Li Xiaolin2, Peng Changhua3, Deng Jia1, Sheng Hao1, Chen Hongwei3, Zhang Chaoju3, He Chuan1, 3
- 1Hubei University of Chinese Medicine, Wuhan 430061, Hubei Province, China; 2Yangtze University, Jingzhou 434023, Hubei Province, China; 3Jingzhou Hospital of Traditional Chinese Medicine Affiliated to Hubei University of Chinese Medicine, Jingzhou 434000, Hubei Province, China
-
Received:2024-02-08Accepted:2024-03-28Online:2025-02-28Published:2024-06-24 -
Contact:He Chuan, Master, Associate professor, Master’s supervisor, Chief physician, Hubei University of Chinese Medicine, Wuhan 430061, Hubei Province, China; Jingzhou Hospital of Traditional Chinese Medicine Affiliated to Hubei University of Chinese Medicine, Jingzhou 434000, Hubei Province, China Co-corresponding author: Li Xiaolin, MD, Associate professor, Yangtze University, Jingzhou 434023, Hubei Province, China -
About author:Zhao Wensheng, Master candidate, Physician, Hubei University of Chinese Medicine, Wuhan 430061, Hubei Province, China -
Supported by:the Construction Project of National Famous Traditional Chinese Medicine Expert Inheritance Workshop, No. [2022]75 (to ZCJ); Hubei Province Natural Science Foundation, No. 2022CFB054 (to LXL); Chinese Medicine Research Project of Hubei Administration of Chinese Medicine, No. ZY2023M051 (to HC); Jingzhou Institute of Traditional Chinese Medicine Independent Topic Project, No. ZZXT2023Y07 (to PCH)
CLC Number:
Cite this article
Zhao Wensheng, Li Xiaolin, Peng Changhua, Deng Jia, Sheng Hao, Chen Hongwei, Zhang Chaoju, He Chuan. Gut microbiota and osteoporotic fractures #br#
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
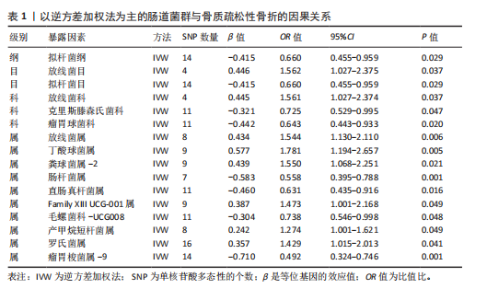
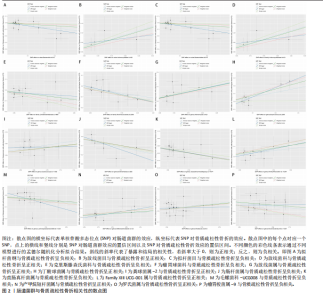
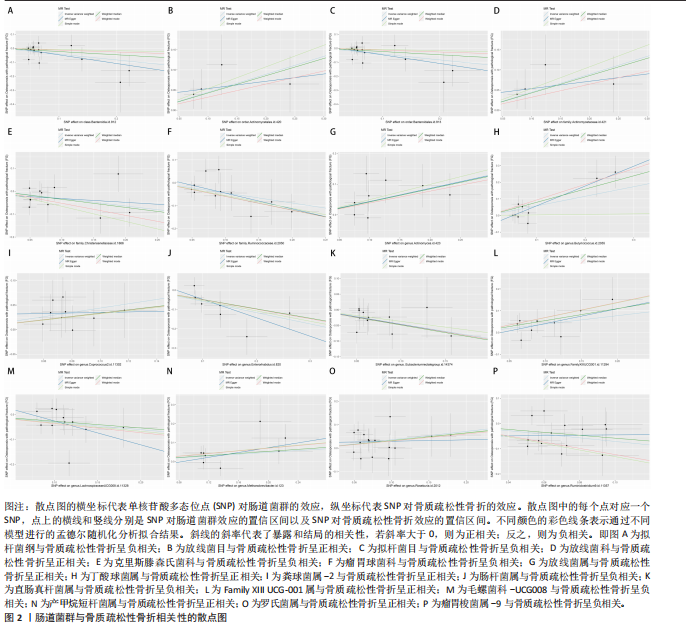
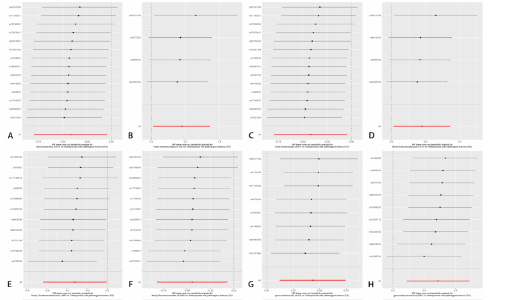
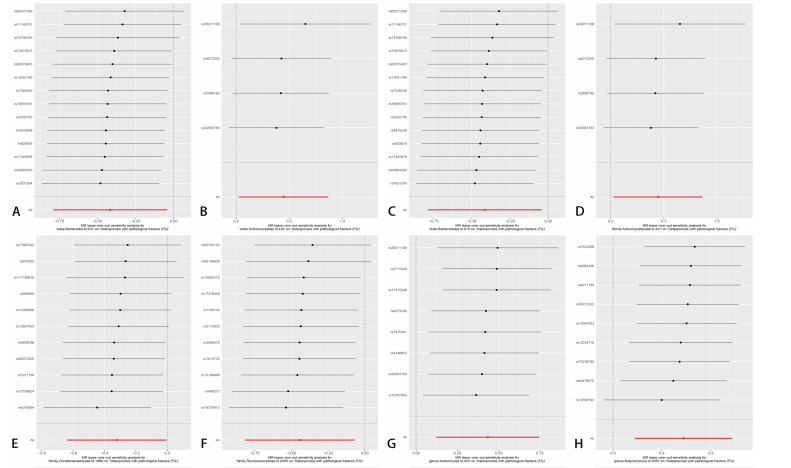
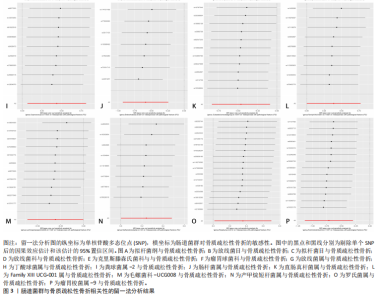
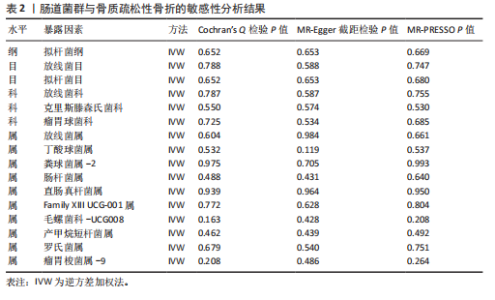
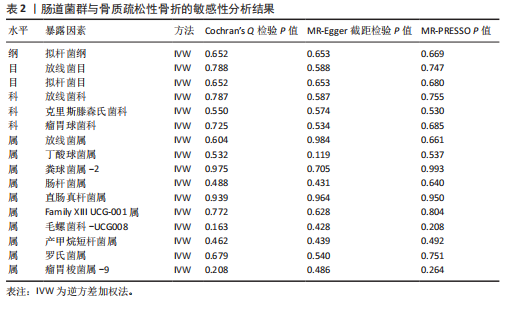
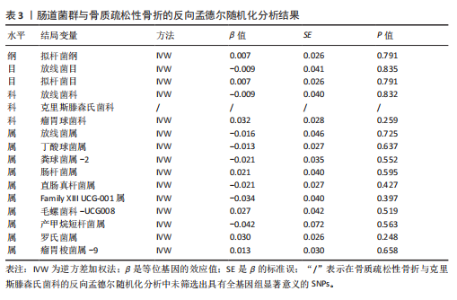
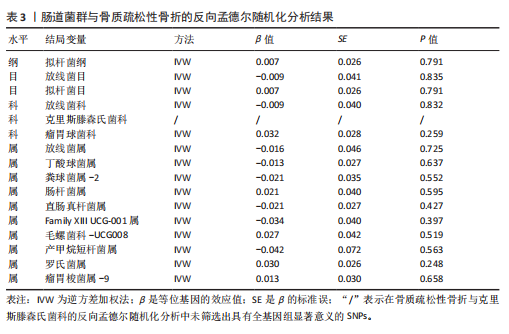
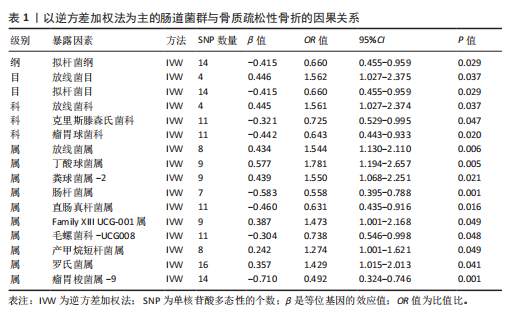
2.1 SNP的筛选结果 此正向MR分析中,文章根据工具变量的筛选标准,在全基因组统计学显著阈值(P < 1×10-5)下筛选出了160个SNPs,包括1个纲、2个目、3个科、10个属,所有纳入的SNP的F 统计量均大于10,表明所有SNP均为强工具变量。其中14个SNPs与拟杆菌纲相关,4个SNPs与放线菌目相关,14个SNPs与拟杆菌目相关,4个SNPs与放线菌科相关,11个SNPs与克里斯滕森氏菌科相关,11个SNPs与瘤胃球菌科相关,8个SNPs与放线菌属相关,9个SNPs与丁酸球菌属相关,9个SNPs与粪球菌属-2相关,7个SNPs与肠杆菌属相关,11个SNPs与直肠真杆菌属相关,9个SNPs与Family XIII UCG-001属相关,11个SNPs与毛螺菌科-UCG008相关,8个SNPs与产甲烷短杆菌属相关,16个SNPs与罗氏菌属相关,14个SNPs与瘤胃梭菌属-9相关,见表1。 2.2 孟德尔随机化分析结果 文章以IVW方法为主要分析方法,发现了16种与骨质疏松性骨折相关的肠道菌群,其中8种肠道菌群与骨质疏松性骨折呈正相关,另外8种肠道菌群与骨质疏松性骨折呈负相关。IVW方法分析结果显示,放线菌目(OR=1.562,95%CI:1.027-2.375,P=0.037)、放线菌科(OR=1.561,95%CI:1.027-2.374,P=0.037)、放线菌属(OR=1.544,95%CI:1.130-2.110,P=0.006)、丁酸球菌属(OR=1.781,95%CI:1.194-2.657,P=0.005)、粪球菌属-2(OR=1.550,95%CI:1.068-2.251,P=0.021)、Family XIII UCG-001属(OR=1.473,95%CI:1.001-2.168,P=0.049)、产甲烷短杆菌属(OR=1.274,95%CI:1.001-1.621,P=0.049)、罗氏菌属(OR=1.429,95%CI:1.015-2.013,P=0.041)的丰度升高,会增加患者骨质疏松性骨折的风险;拟杆菌纲(OR=0.660,95%CI:0.455-0.959,P=0.029)、拟杆菌目(OR=0.660,95%CI:0.455-0.959,P=0.029)、克里斯滕森氏菌科(OR=0.725,95%CI:0.529-0.995,P=0.047)、瘤胃球菌科(OR=0.643,95%CI:0.443-0.933,P=0.020)、肠杆菌属(OR=0.558,95%CI:0.395-0.788,P=0.001)、直肠真杆菌属(OR=0.631,95%CI:0.435-0.916,P=0.016)、毛螺菌科-UCG008 (OR=0.738,95%CI:0.546-0.998,P=0.048)、瘤胃梭菌属-9(OR=0.492,95%CI:0.324-0.746,P=0.001)的丰度升高,会降低患者骨质疏松性骨折的风险。此外,文章还使用了MR-Egger回归、WME方法、SM方法、WM方法对IVW方法的结果进行补充验证,结果显示,其他4种方法结果的方向与IVW方法一致,见图2。 2.3 敏感性分析结果 2.3.1 异质性检验和水平多效性检验结果 经Cochran’s Q检验和MR-Egger截距检验发现,P值均大于0.05,因此此MR分析结果不存在异质性和水平多效性。MR-PRESSO方法结果显示,未检测到离群值,见表2。 2.3.2 留一法检验结果 通过留一法检验评估此MR结果的稳定性,依次剔除每个SNP,再计算剩余SNPs的meta效应,结果显示,不存在单个SNP对因果关系估计值产生较大影响,表明此MR分析结果较为稳定,见图3。 2.4 反向MR分析结果 文章对骨质疏松性骨折与正向MR分析中确定的16个肠道菌群进行反向MR分析,除了以克里斯滕森氏菌科为结局变量的反向MR分析未筛选出具有全基因组显著意义的SNPs,其他分析结果的P值均大于0.05,表明骨质疏松性骨折与各个水平的肠道菌群不具有反向因果关系,进一步验证了正向MR分析得出的结果,见表3。"
| [1] GOLOB AL, LAYA MB. Osteoporosis: screening, prevention, and management. Med Clin North Am. 2015;99(3):587-606. [2] LEMS WF, DREINHÖFER KE, BISCHOFF-FERRARI H, et al. EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis. 2017; 76(5):802-810. [3] SI L, WINZENBERG TM, JIANG Q, et al. Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos Int. 2015;26(7):1929-1937. [4] RUBIN CD. Emerging concepts in osteoporosis and bone strength. Curr Med Res Opin. 2005; 21(7):1049-1056. [5] FAN Y, PEDERSEN O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19(1):55-71. [6] YAN J, HERZOG JW, TSANG K, et al. Gut microbiota induce IGF-1 and promote bone formation and growth. Proc Natl Acad Sci U S A. 2016;113(47):E7554-E7563. [7] DING K, HUA F, DING W. Gut microbiome and osteoporosis. Aging Dis. 2020;11(2):438-447. [8] ORWOLL ES, PARIMI N, WIEDRICK J, et al. Analysis of the associations between the human fecal microbiome and bone density, structure, and strength: the osteoporotic fractures in men (MrOS) Cohort. J Bone Miner Res. 2022;37(4):597-607. [9] GUSS JD, HORSFIELD MW, FONTENELE FF, et al. Alterations to the gut microbiome impair bone strength and tissue material properties. J Bone Miner Res. 2017;32(6):1343-1353. [10] ROSELLÓ-AÑÓN A, CHIAPPE C, VALVERDE-VÁZQUEZ MR, et al. Pilot study to determine the association between gut microbiota and fragility hip fracture. Rev Esp Cir Ortop Traumatol. 2023;67(4):279-289. [11] OZAKI D, KUBOTA R, MAENO T, et al. Association between gut microbiota, bone metabolism, and fracture risk in postmenopausal Japanese women. Osteoporos Int. 2021;32(1):145-156. [12] BIRNEY E. Mendelian randomization. Cold Spring Harb Perspect Med. 2022;12(4):a041302. [13] YUAN S, MASON AM, BURGESS S, et al. Genetic liability to insomnia in relation to cardiovascular diseases: a Mendelian Randomisation study. Eur J Epidemiol. 2021;36(4):393-400. [14] DAVIES NM, HOLMES MV, DAVEY SG. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601. [15] DAVEY SG, HEMANI G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89-R98. [16] KURILSHIKOV A, MEDINA-GOMEZ C, BACIGALUPE R, et al. Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat Genet. 2021;53(2):156-165. [17] SANNA S, VAN ZUYDAM NR, MAHAJAN A, et al. Causal relationships among the gut microbiome, short-chain fatty acids and metabolic diseases. Nat Genet. 2019;51(4):600-605. [18] LI P, WANG H, GUO L, et al. Association between gut microbiota and preeclampsia-eclampsia: a two-sample Mendelian randomization study. BMC Med. 2022;20(1):443. [19] XIAO Z, WANG Z, ZHANG T, et al. Bidirectional Mendelian randomization analysis of the genetic association between primary lung cancer and colorectal cancer. J Transl Med. 2023;21(1):722. [20] KAMAT MA, BLACKSHAW JA, YOUNG R, et al. PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics. 2019;35(22): 4851-4853. [21] PALMER TM, LAWLOR DA, HARBORD RM, et al. Using multiple genetic variants as instrumental variables for modifiable risk factors. Stat Methods Med Res. 2012;21(3):223-242. [22] SLOB E, BURGESS S. A comparison of robust Mendelian randomization methods using summary data. Genet Epidemiol. 2020;44(4): 313-329. [23] BOWDEN J, DAVEY SG, HAYCOCK PC, et al. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304-314. [24] LI J, BAI H, QIAO H, et al. Causal effects of COVID-19 on cancer risk: a Mendelian randomization study. J Med Virol. 2023,95(4): e28722. [25] GRECO MF, MINELLI C, SHEEHAN NA, et al. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med. 2015; 34(21):2926-2940. [26] BOWDEN J, DAVEY SG, BURGESS S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512-525. [27] VERBANCK M, CHEN CY, NEALE B, et al. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693-698. [28] BURGESS S, BOWDEN J, FALL T, et al. Sensitivity analyses for robust causal inference from mendelian randomization analyses with multiple genetic variants. Epidemiology. 2017; 28(1):30-42. [29] LAWLOR DA. Commentary: two-sample Mendelian randomization: opportunities and challenges. Int J Epidemiol. 2016;45(3): 908-915. [30] SHEVROJA E, CAFARELLI FP, GUGLIELMI G, et al. DXA parameters, trabecular bone score (TBS) and bone mineral density (BMD), in fracture risk prediction in endocrine-mediated secondary osteoporosis. Endocrine. 2021;74(1):20-28. [31] PAN B, CAI J, ZHAO P, et al. Relationship between prevalence and risk of osteoporosis or osteoporotic fracture with non-alcoholic fatty liver disease: a systematic review and meta-analysis. Osteoporos Int. 2022;33(11):2275-2286. [32] ZHONG X, ZHANG F, YIN X, et al. Bone homeostasis and gut microbial-dependent signaling pathways. J Microbiol Biotechnol. 2021;31(6):765-774. [33] LU L, CHEN X, LIU Y, et al. Gut microbiota and bone metabolism. FASEB J. 2021;35(7):e21740. [34] TU Y, YANG R, XU X, et al. The microbiota-gut-bone axis and bone health. J Leukoc Biol. 2021; 110(3):525-537. [35] WOOTTON RE, JONES HJ, SALLIS HM. Mendelian randomisation for psychiatry: how does it work, and what can it tell us? Mol Psychiatry. 2022;27(1):53-57. [36] PAGONI P, DIMOU NL, MURPHY N, et al. Using Mendelian randomisation to assess causality in observational studies. Evid Based Ment Health. 2019;22(2):67-71. [37] HAYCOCK PC, BURGESS S, WADE KH, et al. Best (but oft-forgotten) practices: the design, analysis, and interpretation of Mendelian randomization studies. Am J Clin Nutr. 2016; 103(4):965-978. [38] WANG Y, ZHANG X, TANG G, et al. The causal relationship between gut microbiota and bone mineral density: a Mendelian randomization study. Front Microbiol. 2023;14:1268935. [39] ZENG HQ, LI G, ZHOU KX, et al. Causal link between gut microbiota and osteoporosis analyzed via Mendelian randomization. Eur Rev Med Pharmacol Sci. 2024;28(2):542-555. [40] 李俊杰,贾鹏,徐又佳.骨质疏松性骨折后再骨折现状及管理策略的研究进展[J].中华骨科杂志,2022,42(22):1514-1522. [41] WANG W, WANG Q, YU L, et al. Bio-orthogonal engineered peptide: a multi-functional strategy for the gene therapy of osteoporotic bone loss. Biomaterials. 2023;302:122352. [42] LUCAS S, OMATA Y, HOFMANN J, et al. Short-chain fatty acids regulate systemic bone mass and protect from pathological bone loss. Nat Commun. 2018;9(1):55. [43] ZHAN Z, TANG H, ZHANG Y, et al. Potential of gut-derived short-chain fatty acids to control enteric pathogens. Front Microbiol. 2022;13: 976406. [44] LIU Y, GUO YL, MENG S, et al. Gut microbiota-dependent Trimethylamine N-Oxide are related with hip fracture in postmenopausal women: a matched case-control study. Aging (Albany NY). 2020;12(11):10633-10641. [45] 王志凌,郭源源,张浩,等.骨免疫微环境中炎症因子诱导骨丢失的机制及免疫治疗研究进展[J].中国骨与关节杂志,2023, 12(12):943-948. [46] LYU Z, HU Y, GUO Y, et al. Modulation of bone remodeling by the gut microbiota: a new therapy for osteoporosis. Bone Res. 2023; 11(1):31. [47] YAN F, CAO H, COVER TL, et al. Colon-specific delivery of a probiotic-derived soluble protein ameliorates intestinal inflammation in mice through an EGFR-dependent mechanism. J Clin Invest. 2011;121(6):2242-2253. [48] LUTGENDORFF F, AKKERMANS LM, SÖDERHOLM JD. The role of microbiota and probiotics in stress-induced gastro-intestinal damage. Curr Mol Med. 2008;8(4):282-298. [49] PUJO J, DE PALMA G, LU J, et al. Gut microbiota modulates visceral sensitivity through calcitonin gene-related peptide (CGRP) production. Gut Microbes. 2023;15(1): 2188874. [50] LIN X, XIAO HM, LIU HM, et al. Gut microbiota impacts bone via Bacteroides vulgatus-valeric acid-related pathways. Nat Commun. 2023; 14(1):6853. [51] LI S, HAN X, LIU N, et al. Lactobacillus plantarum attenuates glucocorticoid-induced osteoporosis by altering the composition of rat gut microbiota and serum metabolic profile. Front Immunol. 2023;14:1285442. [52] WANG Z, LIANG Y, YU J, et al. Guchang Zhixie Wan protects mice against dextran sulfate sodium-induced colitis through modulating the gut microbiota in colon. J Ethnopharmacol. 2020;260:112991. [53] LOW A, LEE J, GOUNOT JS, et al. Mutual exclusion of methanobrevibacter species in the human gut microbiota facilitates directed cultivation of a candidatus methanobrevibacter intestini representative. Microbiol Spectr. 2022;10(4):e84922. [54] COLLINS KH, PAUL HA, REIMER RA, et al. Relationship between inflammation, the gut microbiota, and metabolic osteoarthritis development: studies in a rat model. Osteoarthritis Cartilage. 2015;23(11):1989-1998. [55] LI Y, LIU C, LUO J, et al. Ershiwuwei Lvxue Pill alleviates rheumatoid arthritis by different pathways and produces changes in the gut microbiota. Phytomedicine. 2022;107:154462. [56] XIE W, HAN Y, LI F, et al. Neuropeptide Y1 receptor antagonist alters gut microbiota and alleviates the ovariectomy-induced osteoporosis in rats. Calcif Tissue Int. 2020; 106(4):444-454. [57] WANG S, WANG S, WANG X, et al. Effects of icariin on modulating gut microbiota and regulating metabolite alterations to prevent bone loss in ovariectomized rat model. Front Endocrinol (Lausanne). 2022;13:874849. [58] MA S, QIN J, HAO Y, et al. Structural and functional changes of gut microbiota in ovariectomized rats and their correlations with altered bone mass. Aging (Albany NY). 2020;12(11):10736-10753. [59] LU H, XU X, FU D, et al. Butyrate-producing Eubacterium rectale suppresses lymphomagenesis by alleviating the TNF-induced TLR4/MyD88/NF-κB axis. Cell Host Microbe. 2022;30(8):1139-1150. [60] WANG Y, SAKKA M, YAGI H, et al. Ruminiclostridium josui Abf62A-Axe6A: a tri-functional xylanolytic enzyme exhibiting α-l-arabinofuranosidase, endoxylanase, and acetylxylan esterase activities. Enzyme Microb Technol. 2018;117:1-8. |
| [1] | Liu Hongtao, Wu Xin, Jiang Xinyu, Sha Fei, An Qi, Li Gaobiao. Causal relationship between age-related macular degeneration and deep vein thrombosis: analysis based on genome-wide association study data [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1602-1608. |
| [2] | Zhang Cuicui, Chen Huanyu, Yu Qiao, Huang Yuxuan, Yao Gengzhen, Zou Xu. Relationship between plasma proteins and pulmonary arterial hypertension and potential therapeutic targets [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1331-1340. |
| [3] | Zeng Hao, Sun Pengcheng, Chai Yuan, Huang Yourong, Zhang Chi, Zhang Xiaoyun. Association between thyroid function and osteoporosis: genome-wide data analysis of European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1019-1027. |
| [4] | Gu Fucheng, Yang Meixin, Wu Weixin, Cai Weijun, Qin Yangyi, Sun Mingyi, Sun Jian, Geng Qiudong, Li Nan. Effects of Guilu Erxian Glue on gut microbiota in rats with knee osteoarthritis: machine learning and 16S rDNA analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1058-1072. |
| [5] | Liu Chu, Qiu Boyuan, Tong Siwen, He Linyuwei, Chen Haobo, Ou Zhixue. A genetic perspective reveals the relationship between blood metabolites and osteonecrosis: an analysis of information from the FinnGen database in Finland [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 785-794. |
| [6] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei, Zhou Jiatan. Based on Mendelian randomization, the causal relationship between 1400 metabolites and sarcopenia and the correlation analysis of cardiovascular disease were investigated [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-11. |
| [7] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [8] | Li Jiatong, Jin Yue, Liu Runjia, Song Bowen, Zhu Xiaoqian, Li Nianhu . Association between thyroid function levels and phenotypes associated with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1312-1320. |
| [9] |
Sun Guanghan, Xie Zhencong, Sun Mi, Xu Yang, Guo Dong.
Therapeutic effect and mechanism by which Trichosanthis Fructus-Allii Macrostemonis Bulbus regulates gut microbiota in a rat model of coronary heart disease #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 917-927.
|
| [10] | Huang Haina, Yu Yanrong, Bi Jian, Huang Miao, Peng Weijie. Epigenetic characteristics of hepatogenic differentiation of mesenchymal stem cells in three-dimensional culture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7848-7855. |
| [11] | Wang Tao, Wang Shunpu, Min Youjiang, Wang Min, Li Le, Zhang Chen, Xiao Weiping. Causal relationship between gut microbiota and rheumatoid arthritis: data analysis in European populations based on GWAS data [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7663-7668. |
| [12] | Liu Xiaowu, Liu Jinping, Wu Ting, He Xian, Cai Jianxiong. Antioxidants from different sources and osteoarthritis: a genome-wide association analysis in European populations [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 7015-7027. |
| [13] | Cui Yuena, Chen Xiaoyu, Liang Meiting, Chen Wujin, He Yi, Dilinur·Ekpa, Du Manxi, Zhu Yuqiu, Abuduwupuer·Haibier, Sun Yuping. Differences of calorie restriction and time-restricted feeding on metabolic indices and gut microbiota of mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6449-6456. |
| [14] | Zhang Bochun, Li Wei, Li Guangzheng, Ding Haoqin, Li Gang, Liang Xuezhen, . Association between neuroimaging changes and osteonecrosis: a large sample analysis from UK Biobank and FinnGen databases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6574-6582. |
| [15] | Luo Weidong, Pu Bin, Gu Peng, Huang Feng, Zheng Xiaohui, Chen Fuhong. Mendelian randomization study on the association between telomere length and 10 common musculoskeletal diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 654-660. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||