Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (17): 3705-3712.doi: 10.12307/2025.648
Previous Articles Next Articles
Association between obesity and diffuse idiopathic skeletal hyperostosis
Kong Luming1, Zhao Diqian1, Bai Wenzhe1, Li Nianhu2
- 1The First Clinical Medical School, Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China; 2Shandong University of Traditional Chinese Medicine Affiliated Hospital, Jinan 250014, Shandong Province, China
-
Received:2024-06-07Accepted:2024-07-26Online:2025-06-18Published:2024-11-07 -
Contact:Li Nianhu, MD, Doctoral supervisor, Chief physician, Shandong University of Traditional Chinese Medicine Affiliated Hospital, Jinan 250014, Shandong Province, China -
About author:Kong Luming, Master candidate, The First Clinical Medical School, Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China -
Supported by:Natural Science Foundation of Shandong Province, No. ZR2023MH063 (to LNH); Construction Project of National Famous Elderly Traditional Chinese Medicine Experts Inheritance Workshop of Xu Xiangan, No. [2022]75 (to LNH)
CLC Number:
Cite this article
Kong Luming, Zhao Diqian, Bai Wenzhe, Li Nianhu. Association between obesity and diffuse idiopathic skeletal hyperostosis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3705-3712.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
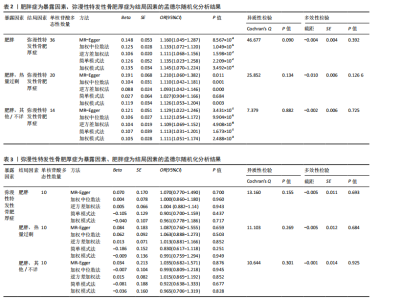
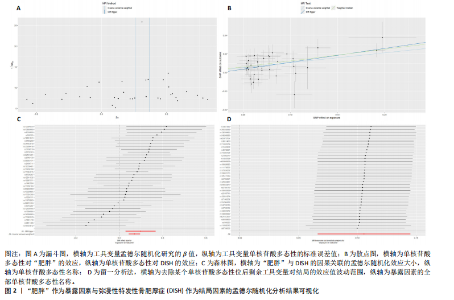
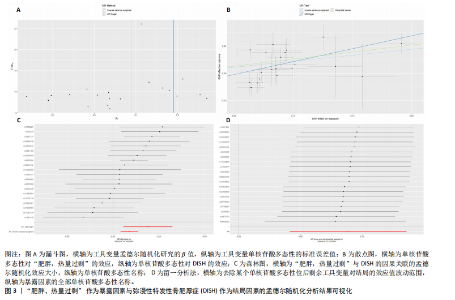
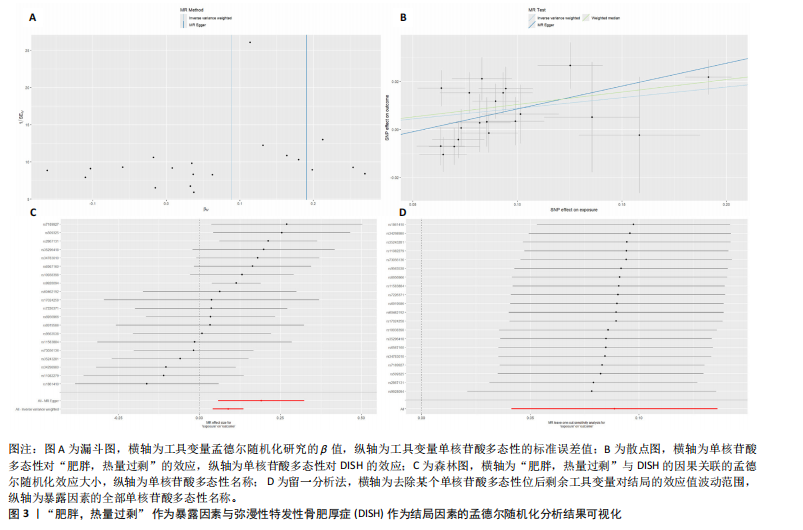
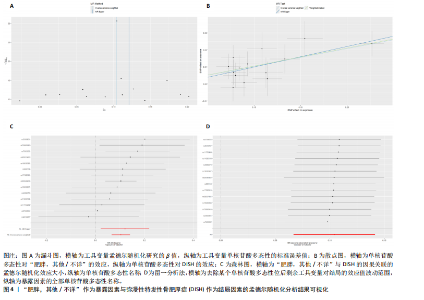
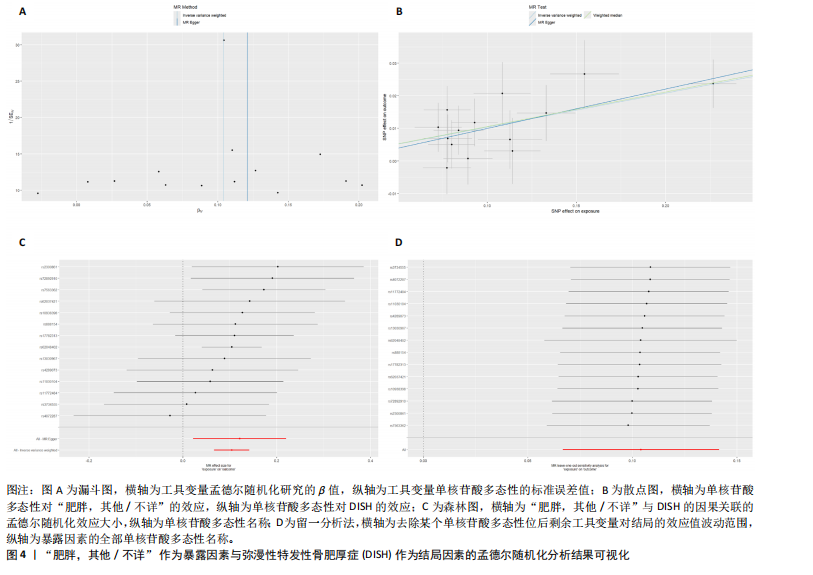
2.1 孟德尔随机化分析 2.1.1 工具变量筛选结果 在确保单核苷酸多态性与暴露因素显著相关,并去除连锁不平衡,排除弱工具变量后,“肥胖”数据集中筛选出了41个单核苷酸多态性,其中1个单核苷酸多态性在DISH数据集中没有相应结果,并排除了4个回文单核苷酸多态性;“肥胖,热量过剩”数据集中筛选出了23个单核苷酸多态性,所有单核苷酸多态性在DISH数据集中均可找到相应结果,并排除了3个回文单核苷酸多态性;“肥胖,其他/不详”数据集中筛选出了15个单核苷酸多态性,所有单核苷酸多态性在DISH数据集中均可找到相应结果,并排除了1个回文单核苷酸多态性。筛选过后的单核苷酸多态性被用于孟德尔随机化分析。 2.1.2 孟德尔随机化分析结果 “肥胖”与DISH之间的关系分析基于逆方差加权法(OR=1.111,95%CI:1.068- 1.156,P=1.598×10-7)显示两者之间存在显著的因果关系。其他4种分析方式也均支持这一结果。逆方差加权法的异质性检验(Q_Pval=0.090)显示不存在异质性,多效性检验(P=0.392)显示不存在水平多效性,MR-PRESSO检验(P=0.116)显示不存在离群值,留一分析法进行敏感性分析,该方法包括依次去除单核苷酸多态性,并重新计算与剩余单核苷酸多态性的因果效应,观察结果是否随着每次单核苷酸多态性去除而变化。该分析显示了稳定的结果,进一步证实了研究结果的可靠性。 “肥胖,热量过剩” 与DISH之间的关系分析基于逆方差加权法(OR=1.093,95%CI:1.042-1.146,P=0.000)显示两者之间存在显著的因果关系。MR-Egger、加权中位数法和加权模式法也均支持这一结果。除此之外,简单模式法(OR=1.027,95%CI:0.904-1.166,P=0.684)在统计上不表现出显著的因果关系,考虑到简单模式在分析时不考虑方差,因此在某些情况下可能准确性较低[23]。 逆方差加权法的异质性检验(Q_Pval= 0.134)显示不存在异质性,多效性检验(P=0.126)显示不存在水平多效性,MR-PRESSO检验(P=0.164)显示不存在离群值,留一分析法进行敏感性分析显示了结果的稳定。总而言之,尽管简单模式法表现出了因果关系的不显著性,但其效应值方向与其他分析方法均一致,为正相关,且该分析方法存在一定的不准确性,因此并不影响对因果关系的验证。 “肥胖,其他/不详”与DISH之间的关系分析基于逆方差加权法(OR=1.109,95%CI:1.069-1.152,P=4.908×10-8)显示两者之间存在显著的因果关系。其他4种分析方式也均支持这一结果。逆方差加权法的异质性检验(Q_Pval=0.882)显示不存在异质性,多效性检验(P=0.725)显示不存在水平多效性,MR-PRESSO检验(P=0.917)显示不存在离群值,留一分析法进行敏感性分析,显示了稳定的结果。 孟德尔随机化分析的详细结果见表2,结果可视化见图2-4。 2.2 反向孟德尔随机化分析结果 为了更深入地研究DISH与肥胖症之间的因果关系,继续进行了双样本孟德尔随机化分析,以DISH作为暴露因素,以肥胖症作为结局因素。数据的选择、工具变量的选择、孟德尔随机化分析的流程和检验方法均与之前相同。在确保单核苷酸多态性与暴露因素显著相关(P < 5×10-8),并去除连锁不平衡(r2 < 0.001,kb < 10 000),排除弱工具变量后,“DISH”数据集中筛选出了11个单核苷酸多态性,这11个单核苷酸多态性均能在“肥胖”和“肥胖,热量过剩”及“肥胖,其他/不详”3个数据集中找到相应结果,且在分析时排除掉1个回文单核苷酸多态性。筛选过后的单核苷酸多态性经过孟德尔随机化分析,5种分析方法的P值均 > 0.05,表明DISH与肥胖症之间没有因果关系。异质性检验和多效性检验也显示出不存在异质性和多效性,MR-PRESSO检验并未发现离群值的存在,证明了分析结果的可靠性。 反向孟德尔随机化分析的详细结果见表3。"

| [1] MADER R, VERLAAN JJ, BUSKILA D. Diffuse idiopathic skeletal hyperostosis: clinical features and pathogenic mechanisms. Nat Rev Rheumatol. 2013;9(12):741-750. [2] FORESTIER J, ROTES-QUEROL J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950;9(4):321-330. [3] RESNICK D, NIWAYAMA G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology. 1976;119(3):559-568. [4] TERZI R. Extraskeletal symptoms and comorbidities of diffuse idiopathic skeletal hyperostosis. World J Clin Cases. 2014; 2(9):422-425. [5] MADER R, NOVOFESTOVSKI I, ADAWI M, et al. Metabolic syndrome and cardiovascular risk in patients with diffuse idiopathic skeletal hyperostosis. Semin Arthritis Rheum. 2009;38(5):361-365. [6] OKADA E, ISHIHARA S, AZUMA K, et al. Metabolic Syndrome is a Predisposing Factor for Diffuse Idiopathic Skeletal Hyperostosis. Neurospine. 2021;18(1):109-116. [7] SETHI A, RUBY JG, VERAS MA, et al. Genetics implicates overactive osteogenesis in the development of diffuse idiopathic skeletal hyperostosis. Nat Commun. 2023; 14(1):2644. [8] WEIR CB, JAN A. BMI Classification Percentile And Cut Off Points. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [9] MOHAMMED MS, SENDRA S, LLORET J, et al. Systems and WBANs for Controlling Obesity. J Healthc Eng. 2018;2018:1564748. [10] SAKLAYEN MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20(2):12. [11] COACCIOLI S, FATATI G, DI CATO L, et al. Diffuse idiopathic skeletal hyperostosis in diabetes mellitus, impaired glucose tolerance and obesity. Panminerva Med. 2000;42(4):247-251. [12] 刘小康,郭海龙,鲍丰,等.弥漫性特发性骨肥厚症的危险因素分析[J].临床骨科杂志,2024,27(1):20-24. [13] EMDIN CA, KHERA AV, KATHIRESAN S. Mendelian Randomization. JAMA. 2017; 318(19):1925-1926. [14] KURKI MI, KARJALAINEN J, PALTA P, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613(7944):508-518. [15] DAVIES NM, HOLMES MV, DAVEY SMITH G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601. [16] PRITCHARD JK, PRZEWORSKI M. Linkage disequilibrium in humans: models and data. Am J Hum Genet. 2001;69(1):1-14. [17] PARK JH, WACHOLDER S, GAIL MH, et al. Estimation of effect size distribution from genome-wide association studies and implications for future discoveries. Nat Genet. 2010;42(7):570-575. [18] BRION MJ, SHAKHBAZOV K, VISSCHER PM. Calculating statistical power in Mendelian randomization studies. Int J Epidemiol. 2013;42(5):1497-1501. [19] BURGESS S, THOMPSON SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32(5):377-389. [20] BOWDEN J, DEL GRECO MF, MINELLI C, et al. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med. 2017;36(11):1783-1802. [21] BOWDEN J, DAVEY SMITH G, BURGESS S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512-525. [22] VERBANCK M, CHEN CY, NEALE B, et al. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693-698. [23] HARTWIG FP, DAVEY SMITH G, BOWDEN J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46(6):1985-1998. [24] BRIKMAN S, LUBANI Y, MADER R, et al. High prevalence of diffuse idiopathic skeletal hyperostosis (DISH) among obese young patients - A retrospective observational study. Semin Arthritis Rheum. 2024;65:152356. [25] HARLIANTO NI, WESTERINK J, FOPPEN W, et al. Visceral Adipose Tissue and Different Measures of Adiposity in Different Severities of Diffuse Idiopathic Skeletal Hyperostosis. J Pers Med. 2021;11(7):663. [26] CHAPUT CD, SIDDIQUI M, RAHM MD. Obesity and calcification of the ligaments of the spine: a comprehensive CT analysis of the entire spine in a random trauma population. Spine J. 2019;19(8):1346-1353. [27] FURUKAWA S, FUJITA T, SHIMABUKURO M, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114(12):1752-1761. [28] DAN LANTSMAN C, HERMAN A, VERLAAN JJ, et al. Abdominal fat distribution in diffuse idiopathic skeletal hyperostosis and ankylosing spondylitis patients compared to controls. Clin Radiol. 2018;73(10):910.e15-910.e20. [29] AHMED O, RAMACHANDRAN K, PATEL Y, et al. Diffuse Idiopathic Skeletal Hyperostosis Prevalence, Characteristics, and Associated Comorbidities: A Cross-Sectional Study of 1815 Whole Spine CT Scans. Global Spine J. 2024;14(4):1201-1209. [30] HIROTA R, TERAMOTO A, YOSHIMOTO M, et al. Osteophyte Bridge Formation Correlates with Vascular Calcification and Cardiovascular Disease in Diffuse Idiopathic Skeletal Hyperostosis. J Clin Med. 2023;12(16):5412. [31] ZINCARELLI C, IERVOLINO S, DI MINNO MN, et al. Diffuse idiopathic skeletal hyperostosis prevalence in subjects with severe atherosclerotic cardiovascular diseases. Arthritis Care Res (Hoboken). 2012;64(11):1765-1769. [32] OUDKERK SF, MOHAMED HOESEIN FAA, PTHM MALI W, et al. Subjects with diffuse idiopathic skeletal hyperostosis have an increased burden of coronary artery disease: An evaluation in the COPDGene cohort. Atherosclerosis. 2019;287:24-29. [33] ORDEN AO, DAVID JM, DÍAZ RP, et al. Association of diffuse idiopathic skeletal hyperostosis and aortic valve sclerosis. Medicina (B Aires). 2014;74(3):205-209. [34] JULKUNEN H, AROMAA A, KNEKT P. Diffuse idiopathic skeletal hyperostosis (DISH) and spondylosis deformans as predictors of cardiovascular diseases and cancer. Scand J Rheumatol. 1981;10(3):241-248. [35] MADER R, LAVI I. Diabetes mellitus and hypertension as risk factors for early diffuse idiopathic skeletal hyperostosis (DISH). Osteoarthritis Cartilage. 2009;17(6):825-828. [36] DENKO CW, MALEMUD CJ. Body mass index and blood glucose: correlations with serum insulin, growth hormone, and insulin-like growth factor-1 levels in patients with diffuse idiopathic skeletal hyperostosis (DISH). Rheumatol Int. 2006;26(4):292-297. [37] FASSIO A, ADAMI G, IDOLAZZI L, et al. Diffuse Idiopathic Skeletal Hyperostosis (DISH) in Type 2 Diabetes: A New Imaging Possibility and a New Biomarker. Calcif Tissue Int. 2021;108(2):231-239. [38] PARIENTE E, PINI SF, OLMOS JM, et al. Early stages of diffuse idiopathic skeletal hyperostosis (DISH) and chronic inflammation: the Camargo Cohort Study. Clin Rheumatol. 2023;42(7):1931-1942. [39] DĄBROWSKI M, KUBASZEWSKI Ł. Diffuse Idiopathic Skeletal Hyperostosis of Cervical Spine with Dysphagia-Molecular and Clinical Aspects. Int J Mol Sci. 2021;22(8):4255. [40] MADER R, PAPPONE N, BARALIAKOS X, et al. Diffuse Idiopathic Skeletal Hyperostosis (DISH) and a Possible Inflammatory Component. Curr Rheumatol Rep. 2021;23(1):6. [41] MADER R, NOVOFASTOVSKI I, SCHWARTZ N, et al. Serum adiponectin levels in patients with diffuse idiopathic skeletal hyperostosis (DISH). Clin Rheumatol. 2018;37(10):2839-2845. |
| [1] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei, Zhou Jiatan. Based on Mendelian randomization, the causal relationship between 1400 metabolites and sarcopenia and the correlation analysis of cardiovascular disease were investigated [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-11. |
| [3] | Dong Tingting, Chen Tianxin, Li Yan, Zhang Sheng, Zhang Lei. Causal relationship between modifiable factors and joint sports injuries [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1953-1962. |
| [4] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [5] |
Zhao Wensheng, Li Xiaolin, Peng Changhua, Deng Jia, Sheng Hao, Chen Hongwei, Zhang Chaoju, He Chuan.
Gut microbiota and osteoporotic fractures #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1296-1304.
|
| [6] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [7] | Li Jiatong, Jin Yue, Liu Runjia, Song Bowen, Zhu Xiaoqian, Li Nianhu . Association between thyroid function levels and phenotypes associated with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1312-1320. |
| [8] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| [9] | Wang Xuepeng, , He Yong, . Effect of insulin-like growth factor family member levels on inflammatory arthritis: a FinnGen biobank-based analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7656-7662. |
| [10] | Wang Tao, Wang Shunpu, Min Youjiang, Wang Min, Li Le, Zhang Chen, Xiao Weiping. Causal relationship between gut microbiota and rheumatoid arthritis: data analysis in European populations based on GWAS data [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7663-7668. |
| [11] | Han Jie, Pan Chengzhen, Shang Yuzhi, Zhang Chi. Identification of immunodiagnostic biomarkers and drug screening for steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7690-7700. |
| [12] | Liu Chenchen, Liu Ruize, Bao Mengmeng, Fang Li, Cao Liquan, Wu Jiangbo. Blood flow restriction training intervention in the elderly with sarcopenic obesity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6963-6970. |
| [13] | Wu Zhenhua, Zhang Xiwei, Wang Yipin, Li Qianqian. Relationship between seven serum lipid traits and osteoarthritis: a large sample analysis of European population in IEU OPEN GWAS database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 7004-7014. |
| [14] | Liu Xiaowu, Liu Jinping, Wu Ting, He Xian, Cai Jianxiong. Antioxidants from different sources and osteoarthritis: a genome-wide association analysis in European populations [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 7015-7027. |
| [15] | Zhang Bochun, Li Wei, Li Guangzheng, Ding Haoqin, Li Gang, Liang Xuezhen, . Association between neuroimaging changes and osteonecrosis: a large sample analysis from UK Biobank and FinnGen databases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6574-6582. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||