[1] AYERS C, KANSAGARA D, LAZUR B, et al. Effectiveness and Safety of Treatments to Prevent Fractures in People With Low Bone Mass or Primary Osteoporosis: A Living Systematic Review and Network Meta-analysis for the American College of Physicians. Ann Intern Med. 2023; 176(2):182-195.
[2] QASEEM A, HICKS LA, ETXEANDIA-IKOBALTZETA I, et al. Pharmacologic Treatment of Primary Osteoporosis or Low Bone Mass to Prevent Fractures in Adults: A Living Clinical Guideline From the American College of Physicians. Ann Intern Med. 2023;176(2):224-238.
[3] SING CW, LIN TC, BARTHOLOMEW S, et al. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post-Fracture Treatment, and All-Cause Mortality. J Bone Miner Res. 2023;38(8):1064-1075.
[4] IMANOJ P, DERWIN R, GEORGE S. What is the impact of daily oral supplementation of vitamin D3 (cholecalciferol) plus calcium on the incidence of hip fracture in older people? A systematic review and meta-analysis. Int J Older People Nurs. 2023;18(1):e12492.
[5] BUZKOVA P, CAULEY JA, FINK HA, et al. Age-Related Factors Associated With The Risk of Hip Fracture. Endocr Pract. 2023;29(6):478-483.
[6] FRYDENDAL T, CHRISTENSEN R, MECHLENBURG I, et al. Total hip arthroplasty versus progressive resistance training in patients with severe hip osteoarthritis: protocol for a multicentre, parallel-group, randomised controlled superiority trial. BMJ Open. 2021;11(10): e051392.
[7] VENDITTOLI PA, GIRARD J, BONNOMET F. Hip Arthroplasty, a mature surgical technique with room for improvement. Orthop Traumatol Surg Res. 2022;108(6):103379.
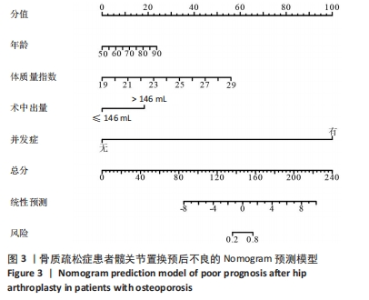
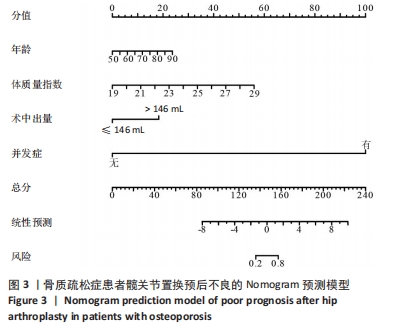
[8] MAZZUCCHI E. Both the nomogram and the score system can represent an useful tool especially in those cases where the complication is foreseen by the surgeon. Int Braz J Urol. 2022;48(5):828-829.
[9] 胥少汀,葛宝丰,徐印坎.实用骨科学[M].3版.北京:人民军医出版社,2005.
[10] 程晓光,王亮,曾强,等.中国定量CT(QCT) 骨质疏松症诊断指南(2018)[J].中国骨质疏松杂志,2019,25(6):733-737.
[11] 朱江龙,陈跃平,董盼锋,等.老年骨质疏松症患者髋关节置换术后预后及相关因素分析[J].中国骨质疏松杂志,2019,25(8):1073-1077.
[12] 蔡成成,汪信德,席永斌.多学科联合治疗在老年骨质疏松性髋部骨折中的疗效分析[J].甘肃医药,2023,42(5):410-412.
[13] AIBAR-ALMAZÁN A, VOLTES-MARTÍNEZ A, CASTELLOTE-CABALLERO Y, et al. Current Status of the Diagnosis and Management of Osteoporosis. Int J Mol Sci. 2022;23(16):9465.
[14] 滕晓洁,王振刚,唐冠兰,等.内分泌疾病与继发性骨质疏松症相关性的研究进展[J].实用中医内科杂志,2023,37(6):59-62.
[15] LEBOFF MS, GREENSPAN SL, INSOGNA KL, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022;33(10):2049-2102.
[16] MCDONOUGH CM, HARRIS-HAYES M, KRISTENSEN MT, et al. Physical Therapy Management of Older Adults With Hip Fracture. J Orthop Sports Phys Ther. 2021;51(2):CPG1-CPG81.
[17] LEX JR, DI MICHELE J, KOUCHEKI R, et al. Artificial Intelligence for Hip Fracture Detection and Outcome Prediction: A Systematic Review and Meta-analysis. JAMA Netw Open. 2023;6(3):e233391.
[18] KHAN AA, ABUALROB H, TARIQ F, et al. Osteoporosis treatment rate following hip fracture in a community hospital. Arch Osteoporos. 2021;16(1):8.
[19] HOLVIK K, ELLINGSEN CL, SOLBAKKEN SM, et al. Cause-specific excess mortality after hip fracture: the Norwegian Epidemiologic Osteoporosis Studies (NOREPOS). BMC Geriatr. 2023;23(1):201.
[20] ALBERGARIA BH, ZERBINI CAF, SZEJNFELD VL, et al. An updated hip fracture incidence rate for Brazil: the Brazilian Validation Osteoporosis Study (BRAVOS). Arch Osteoporos. 2022;17(1):90.
[21] 钱颖玲.连续性护理干预在预防全髋关节置换术患者下肢深静脉血栓形成中的效果[J].透析与人工器官,2023,34(1):104-108.
[22] DESCAMPS J, TEISSIER V, GRAFF W, et al. Managing early complications in total hip arthroplasty: the safety of immediate revision. J Orthop Traumatol. 2023;24(1):38.
[23] KARASAVVIDIS T, BOURIS V, XIANG W, et al. Prophylaxis for Venous Thromboembolic Events in Elective Total Hip and Total Knee Arthroplasty. Curr Pharm Des. 2022;28(10):771-777.
[24] PARIKH S, PANNU TS, DAVIS T, et al. Local Soft-Tissue Thickness vs. Body Mass Index as Predictors of Complications After Total Knee or Hip Arthroplasty: A Literature Review. JBJS Rev. 2023;11(11). doi: 10.2106/JBJS.RVW.22.00128.
[25] 杨昌凤,何永琴,易德坤,等.老年髋部骨折患者术后1年内死亡的影响因素分析及列线图预测模型构建[J].陆军军医大学学报, 2023,45(1):60-66.
[26] 邵菲,李燕,陈晶,等.髋部骨折术后非计划入住重症监护病房的列线图预测模型构建与分析[J].实用骨科杂志,2022,28(2):114-119.
[27] RIBEIRO U JR. Nomogram for Predicting Pathologic Response Following Neoadjuvant Chemotherapy or Chemoradiotherapy in Patients with Esophageal Cancer. Ann Surg Oncol. 2023;30(4):1945-1947.
[28] 郑红波,梅伟,李勇,等.不同麻醉方式对老年全膝关节置换术早期预后的影响:一项单中心回顾性研究[J].骨科,2024,15(2):109-114.
[29] 千建荣,朱仕文.采用空心钉内固定与半髋关节置换治疗老年Garden Ⅰ、Ⅱ型股骨颈骨折的疗效对比[J].骨科临床与研究杂志, 2023,8(6):350-355.
[30] 俞荣耀,庞清江,陈先军,等.非移位型股骨颈骨折股骨头后倾角测量及对预后影响的研究进展[J].中国骨伤,2023,36(10):969-974.
[31] 张斌飞,庄岩,刘林,等.全髋关节置换术治疗髋臼骨折研究进展[J].中国骨与关节损伤杂志,2023,38(8):888-892.
[32] 吴栋姣,王馨,陈黛楠,等.术前修正衰弱指数联合血清PGE_2、IL-17A预测老年髋关节置换术患者术后谵妄的临床研究[J].现代生物医学进展,2023,23(15):2847-2851.
[33] 张苏立,葛红艳,叶萍.肥胖对患者初次全髋关节置换术后护理疗效及预后的影响[J].当代护士(上旬刊),2020,27(12):97-98.
[34] 王晨光.肥胖股骨头坏死患者行人工全髋关节置换术的疗效及并发症分析[D].郑州:河南大学,2021.
[35] 沈伟明,高兵,陈杰.老年全髋关节置换术后慢性疼痛的影响因素分析[J].中国当代医药,2022,29(11):56-59+63.
[36] 孙晶.腹腔镜手术治疗良性卵巢肿瘤临床效果观察[J].中西医结合心血管病电子杂志,2020,8(34):61+74.
[37] 陈曦.SuperPATH入路髋关节置换术治疗老年股骨颈骨折患者的效果及其对髋关节功能、骨代谢相关因子表达水平的影响[J].中国现代医药杂志,2023,25(9):70-73.
[38] 邓星军,胡祖湘.半髋与全髋关节置换术对老年股骨颈骨折患者围术期指标及髋关节功能的影响对比[J].现代诊断与治疗,2023, 34(15):2325-2327.
[39] 靳贺,危朝辉,张琦,等.肋骨骨折评分和肋骨评分对创伤性肋骨骨折患者伤情的评估价值及对不良预后事件的预测效能研究[J].创伤外科杂志,2023,25(6):437-442.
[40] 钟晶.围术期预见性护理对全髋关节置换术患者术后患肢功能恢复及关节脱位的预防效果[J].医学信息,2023,36(22):167-170.
|