Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (26): 5572-5578.doi: 10.12307/2025.771
Previous Articles Next Articles
Emodin promotes autophagy to improve myocardial injury in septic model mice
Tian Yong, Zhou Qing, Luo Chuanquan, Hu Hongmei, Ma Changlin, Yang Lei, Wei Lin
- Department of Critical Care Medicine, Tongren People’s Hospital, Tongren 554300, Guizhou Province, China
-
Received:2024-09-04Accepted:2024-10-16Online:2025-09-18Published:2025-02-25 -
Contact:Wei Lin, Chief physician, Professor, Department of Critical Care Medicine, Tongren People’s Hospital, Tongren 554300, Guizhou Province, China -
About author:Tian Yong, MS, Attending physician, Department of Critical Care Medicine, Tongren People’s Hospital, Tongren 554300, Guizhou Province, China -
Supported by:Guizhou Provincial Administration of Traditional Chinese Medicine Chinese Medicine, Ethnic Medicine Science and Technology Research Funding, No. QZYY-2024-047 (to TY); Tongren City Science and Technology Plan Project, No. [2023]30 (to TY); Guizhou Provincial Science and Technology Plan Project, No. [2021]092 (to MCL)
CLC Number:
Cite this article
Tian Yong, Zhou Qing, Luo Chuanquan, Hu Hongmei, Ma Changlin, Yang Lei, Wei Lin. Emodin promotes autophagy to improve myocardial injury in septic model mice[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5572-5578.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
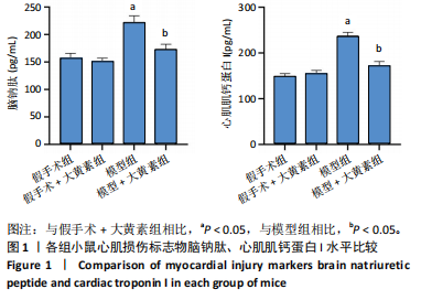
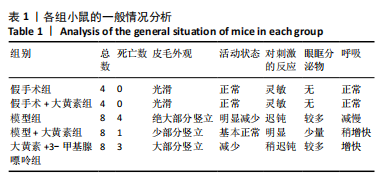
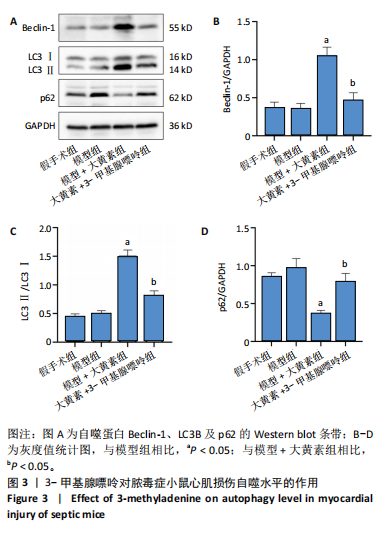
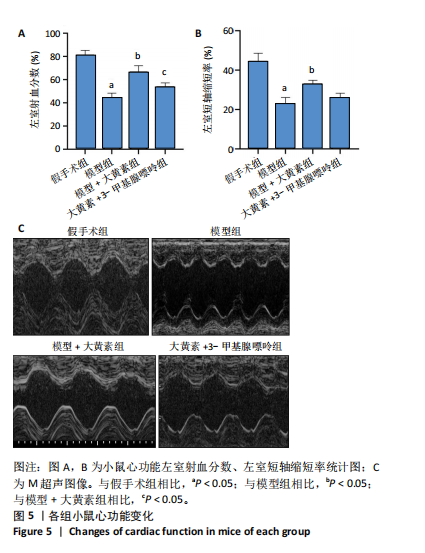
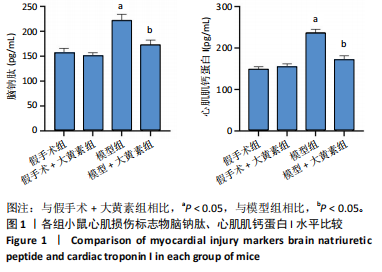
2.2 大黄素预处理对脓毒症小鼠心肌损伤的保护作用 采用ELISA方法评估各组小鼠血清中代表心脏损伤程度的生物标志物水平(图1)。与假手术组相比,假手术+大黄素组脑钠肽、心肌肌钙蛋白I水平均无统计学意义(P > 0.05);与假手术+大黄素组相比,模型组脑钠肽、心肌肌钙蛋白I水平均显著升高(P < 0.05);与模型组相比,模型+大黄素组脑钠肽、心肌肌钙蛋白I水平均显著降低(P < 0.05)。 2.3 大黄素预处理对脓毒症小鼠心肌损伤自噬水平的影响 采用Western blot方法检测各组小鼠心肌组织中自噬相关蛋白LC3B与p62的相对表达量(图2),与假手术组相比,假手术+大黄素组和模型组自噬标志物LC3Ⅱ/LC3Ⅰ、p62的蛋白相对表达量差异无显著性意义(P > 0.05);与模型组相比,模型+大黄素组LC3Ⅱ/LC3Ⅰ的蛋白相对表达量显著升高且p62的蛋白相对表达量显著降低(P < 0.05)。 2.4 3-甲基腺嘌呤对脓毒症小鼠心肌损伤自噬水平的作用 采用Western blot方法检测各组小鼠心肌中自噬蛋白LC3B、Beclin-1及p62的相对表达水平(图3),与假手术组相比,模型组LC3Ⅱ/LC3Ⅰ、Beclin-1及p62的蛋白相对表达量差异无显著性意义(P > 0.05);与模型组相比,模型+大黄素组LC3Ⅱ/LC3Ⅰ和Beclin-1的蛋白相对表达量均显著升高且p62的蛋白相对表达量显著降低(P < 0.05);与模型+大黄素组相比,大黄素+3-甲基腺嘌呤组LC3Ⅱ/LC3Ⅰ和Beclin-1的蛋白相对表达量均显著降低且p62的蛋白相对表达量显著升高(P < 0.05)。 2.5 大黄素促进自噬对脓毒症小鼠心肌损伤的作用 采用苏木精-伊红染色观察各组小鼠心肌组织的病理变化特征(图4)。假手术组小鼠心肌纤维结构有序,无明显水肿迹象,亦未观察到炎症细胞的浸润;模型组小鼠展现出心肌纤维排列杂乱、伴随显著组织水肿及大量炎症细胞的浸润现象;模型+大黄素组心肌纤维排列轻微紊乱、轻度水肿,部分组织出现少量空泡样结构变化;大黄素+3-甲基腺嘌呤组心肌组织表现出结构紊乱、水肿,并见较多的炎症细胞浸润。 2.6 大黄素促进自噬对脓毒症小鼠心肌功能障碍的作用 采用动物超声技术评估各组小鼠的左心室短轴缩短率及左心室射血分数(图5)。与假手术组相比,模型组左心室短轴缩短率、左心室射血分数均显著降低(P < 0.05);与模型组相比,模型+大黄素组左室短轴缩短率、左室射血分数均升高(P < 0.05);与模型+大黄素组相比,大黄素+3-甲基腺嘌呤组左室射血分数降低(P < 0.05),左室短轴缩短率降低但无统计学意义(P > 0.05)。"
| [1] PÓVOA P, COELHO L, DAL-PIZZOL F, et al. How to use biomarkers of infection or sepsis at the bedside: guide to clinicians. Intensive Care Med. 2023;49(2):142-153. [2] LI Y, ZHANG L, ZHANG P, et al. Dehydrocorydaline Protects Against Sepsis-Induced Myocardial Injury Through Modulating the TRAF6/NF-κB Pathway. Front Pharmacol. 2021;12:709604. [3] WANG Z, QIANG X, PENG Y, et al. Design and synthesis of salidroside analogs and their bioactivity against septic myocardial injury. Bioorg Chem. 2023;138:106609. [4] FRENCKEN JF, VAN SMEDEN M, VAN DE GROEP K, et al. Etiology of Myocardial Injury in Critically Ill Patients with Sepsis: A Cohort Study. Ann Am Thorac Soc. 2022;19(5):773-780. [5] BI CF, LIU J, YANG LS, et al. Research Progress on the Mechanism of Sepsis Induced Myocardial Injury. J Inflamm Res. 2022;15:4275-4290. [6] GAO Y, LIU J, LI K, et al. Metformin Alleviates Sepsis-Associated Myocardial Injury by Enhancing AMP-Activated Protein Kinase/Mammalian Target of Rapamycin Signaling Pathway-Mediated Autophagy. J Cardiovasc Pharmacol. 2023;82(4):308-317. [7] KLIONSKY DJ, PETRONI G, AMARAVADI RK, et al. Autophagy in major human diseases. EMBO J. 2021;40(19):e108863. [8] SUN Y, CAI Y, ZANG QS. Cardiac Autophagy in Sepsis. Cells. 2019;8(2): 141. [9] CAO W, LI J, YANG K, et al. An overview of autophagy: Mechanism, regulation and research progress. Bull Cancer. 2021;108(3):304-322. [10] IRIONDO MN, ETXANIZ A, VARELA YR, et al. LC3 subfamily in cardiolipin-mediated mitophagy: a comparison of the LC3A, LC3B and LC3C homologs. Autophagy. 2022;18(12):2985-3003. [11] SUN Y, YAO X, ZHANG QJ, et al. Beclin-1-Dependent Autophagy Protects the Heart During Sepsis. Circulation. 2018;138(20):2247-2262. [12] SHU X, SUN Y, SUN X, et al. The effect of fluoxetine on astrocyte autophagy flux and injured mitochondria clearance in a mouse model of depression. Cell Death Dis. 2019;10(8):577. [13] HO J, YU J, WONG SH, et al. Autophagy in sepsis: Degradation into exhaustion? Autophagy. 2016;12(7):1073-1082. [14] ZHANG P, LI Y, FU Y, et al. Inhibition of Autophagy Signaling via 3-methyladenine Rescued Nicotine-Mediated Cardiac Pathological Effects and Heart Dysfunctions. Int J Biol Sci. 2020;16(8):1349-1362. [15] BARICHELLO T, GENEROSO JS, SINGER M, et al. Biomarkers for sepsis: more than just fever and leukocytosis-a narrative review. Crit Care. 2022;26(1):14. [16] MCDONALD SJ, VANDERVEEN BN, VELAZQUEZ KT, et al. Therapeutic Potential of Emodin for Gastrointestinal Cancers. Integr Cancer Ther. 2022;21:15347354211067469. [17] QIN B, ZENG Z, XU J, et al. Emodin inhibits invasion and migration of hepatocellular carcinoma cells via regulating autophagy-mediated degradation of snail and β-catenin. BMC Cancer. 2022;22(1):671. [18] 徐瑞明,邵峥谊,王大为,等.大黄素对脓毒症大鼠心肌损伤的保护作用 [J].西部医学,2020,32(10):1443-1446. [19] 田勇,周颖,古雍翔,等.二甲双胍预处理诱导心脏自噬减轻脓毒症小鼠的心肌损伤[J].中国组织工程研究,2024,28(28):4469-4476. [20] GAO LL, WANG ZH, MU YH, et al. Emodin Promotes Autophagy and Prevents Apoptosis in Sepsis-Associated Encephalopathy through Activating BDNF/TrkB Signaling. Pathobiology. 2022;89(3):135-145. [21] 田勇,周颖,古雍翔,等.二甲双胍诱导心肌细胞自噬对脓毒症小鼠心肌损伤的保护机制[J].安徽医科大学学报,2024,59(1):92-98. [22] PEI XB, LIU B. Research Progress on the Mechanism and Management of Septic Cardiomyopathy: A Comprehensive Review. Emerg Med Int. 2023;2023:8107336. [23] ZOU HX, QIU BQ, ZHANG ZY, et al. Dysregulated autophagy-related genes in septic cardiomyopathy: Comprehensive bioinformatics analysis based on the human transcriptomes and experimental validation. Front Cardiovasc Med. 2022;9:923066. [24] TANG R, JIA L, LI Y, et al. Narciclasine attenuates sepsis-induced myocardial injury by modulating autophagy. Aging (Albany NY). 2021; 13(11):15151-15163. [25] WONG SQ, KUMAR AV, MILLS J, et al. Autophagy in aging and longevity. Hum Genet. 2020;139(3):277-290. [26] GROSS AS, GRAEf M. Mechanisms of Autophagy in Metabolic Stress Response. J Mol Biol. 2020;432(1):28-52. [27] LIU C, LIU Y, CHEN H, et al. Myocardial injury: where inflammation and autophagy meet. Burns Trauma. 2023;11:tkac062. [28] DU J, ZHOU Y. Propofol reduces lipopolysaccharide‑induced cardiomyocyte injury in sepsis by activating SIRT1‑mediated autophagy. Exp Ther Med. 2023;25(4):187. [29] WANG X, XIE D, DAI H, et al. Clemastine protects against sepsis-induced myocardial injury in vivo and in vitro. Bioengineered. 2022;13(3): 7134-7146. [30] QIN GW, LU P, PENG L, et al. Ginsenoside Rb1 Inhibits Cardiomyocyte Autophagy via PI3K/Akt/mTOR Signaling Pathway and Reduces Myocardial Ischemia/Reperfusion Injury. Am J Chin Med. 2021;49(8): 1913-1927. [31] WANG X, YANG S, LI Y, et al. Role of emodin in atherosclerosis and other cardiovascular diseases: Pharmacological effects, mechanisms, and potential therapeutic target as a phytochemical. Biomed Pharmacother. 2023;161:114539. [32] SU J, ZHOU F, WU S, et al. Research Progress on Natural Small-Molecule Compounds for the Prevention and Treatment of Sepsis. Int J Mol Sci. 2023;24(16):12732. [33] CUI Y, CHEN LJ, HUANG T, et al. The pharmacology, toxicology and therapeutic potential of anthraquinone derivative emodin. Chin J Nat Med. 2020;18(6):425-435. [34] DAI S, YE B, CHEN L, et al. Emodin alleviates LPS-induced myocardial injury through inhibition of NLRP3 inflammasome activation. Phytother Res. 2021;35(9):5203-5213. [35] TU YJ, TAN B, JIANG L, et al. Emodin Inhibits Lipopolysaccharide-Induced Inflammation by Activating Autophagy in RAW 264.7 Cells. Chin J Integr Med. 2021;27(5):345-352. [36] LIU H, WANG Q, SHI G, et al. Emodin Ameliorates Renal Damage and Podocyte Injury in a Rat Model of Diabetic Nephropathy via Regulating AMPK/mTOR-Mediated Autophagy Signaling Pathway. Diabetes Metab Syndr Obes. 2021;14:1253-1266. [37] WU P, XIAO Y, QING L, et al. Emodin activates autophagy to suppress oxidative stress and pyroptosis via mTOR-ULK1 signaling pathway and promotes multi-territory perforator flap survival. Biochem Biophys Res Commun. 2024;704:149688. [38] SHE H, TAN L, DU Y, et al. VDAC2 malonylation participates in sepsis-induced myocardial dysfunction via mitochondrial-related ferroptosis. Int J Biol Sci. 2023;19(10):3143-3158. [39] SHEN XD, ZHANG HS, ZHANG R, et al. Progress in the Clinical Assessment and Treatment of Myocardial Depression in Critically Ill Patient with Sepsis. J Inflamm Res. 2022;15:5483-5490. [40] LIU FJ, GU TJ, WEI DY. Emodin alleviates sepsis-mediated lung injury via inhibition and reduction of NF-kB and HMGB1 pathways mediated by SIRT1. Kaohsiung J Med Sci. 2022;38(3):253-260. [41] GUO R, LI Y, HAN M, et al. Emodin attenuates acute lung injury in Cecal-ligation and puncture rats. Int Immunopharmacol. 2020;85:106626. [42] DONG Y, ZHANG L, JIANG Y, et al. Emodin reactivated autophagy and alleviated inflammatory lung injury in mice with lethal endotoxemia. Exp Anim. 2019;68(4):559-568. [43] CHANG X, HE Y, WANG L, et al. Puerarin Alleviates LPS-Induced H9C2 Cell Injury by Inducing Mitochondrial Autophagy. J Cardiovasc Pharmacol. 2022;80(4):600-608. [44] ZHANG W, ZHANG J. Semaglutide Pretreatment Induces Cardiac Autophagy to Reduce Myocardial Injury in Septic Mice. Discov Med. 2023;35(178):853-860. [45] WU B, SONG H, FAN M, et al. Luteolin attenuates sepsis‑induced myocardial injury by enhancing autophagy in mice. Int J Mol Med. 2020;45(5):1477-1487. |
| [1] | Li Huayuan, Li Chun, Liu Junwei, Wang Ting, Li Long, Wu Yongli. Effect of warm acupuncture on PINK1/Parkin pathway in the skeletal muscle of rats with chronic fatigue syndrome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1618-1625. |
| [2] | Zhou Panpan, Cui Yinglin, Zhang Wentao, Wang Shurui, Chen Jiahui, Yang Tong . Role of cellular autophagy in cerebral ischemic injury and the regulatory mechanism of traditional Chinese medicine [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1650-1658. |
| [3] | Zhu Hanmin, Wang Song, Xiao Wenlin, Zhang Wenjing, Zhou Xi, He Ye, Li Wei, . Mitophagy regulates bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1676-1683. |
| [4] | Zheng Rongfa, Mo Weibin, Huang Peng, Chen Junji, Liang Ting, Zi Fangyu, Li Guofeng. Effects of electroacupuncture on the expression of metabolic enzymes and autophagy genes in gastrocnemius muscle tissues of exercising rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1127-1136. |
| [5] | Chen Yuning, Jiang Ying, Liao Xiangyu, Chen Qiongjun, Xiong Liang, Liu Yue, Liu Tong. Buqi Huoxue Compounds intervene with the expression of related factors and autophagy related proteins in a rat model of cerebral ischemia/reperfusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1152-1158. |
| [6] | Liu Lingyun, He Guixin, Qin Weibin, Song Hui, Zhang Liwen, Tang Weizhi, Yang Feifei, Zhu Ziyi, Ou Yangbin . Improvement of myocardial injury by traditional Chinese medicine: mitochondrial calcium homeostasis mediates macrophage autophagy and pyroptosis pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1276-1284. |
| [7] | Xu Tianjie, Fan Jiaxin, Guo Xiaoling, Jia Xiang, Zhao Xingwang, Liu kainan, Wang Qian. Metformin exerts a protective effect on articular cartilage in osteoarthritis rats by inhibiting the PI3K/AKT/mTOR pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1003-1012. |
| [8] | Zhang Fei, Zuo Jun. Inhibition of hypertrophic scar in rats by beta-sitosterol-laden mesoporous silica nanoparticles [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7301-7309. |
| [9] | Yan Laijun, Ge Haiya, Wang Zhengming, Yang Zongrui, Niu Lifeng, Zhan Hongsheng. Mechanism by which Tongdu Huoxue Decoction inhibits macrophage inflammation to delay intervertebral disc degeneration in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6851-6857. |
| [10] | Nigeayi · Aihemaiti, Yilidanna · Dilixiati, An Wei, Maimaitituxun · Tuerdi. Expression of mitochondrial creatine kinase 2 in a rat model of temporomandibular joint osteoarthritis and its role in inflammation progression [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6877-6884. |
| [11] | Wang Ziheng, Wu Shuang. Oxidative stress-related genes and molecular mechanisms after spinal cord injury: data analysis and verification based on GEO database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6893-6904. |
| [12] | Lu Xiuli, Xu Huazhen, Chen Yuxing, Yao Nan, Hu Zixuan, Huang Dane. Mechanism of Jiangu Formula in treating osteoporosis based on osteoclast-osteoblast coupling [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6828-6835. |
| [13] | He Changliang, Wang Yan, Luo Ling, Liu Jian. Human umbilical cord-derived mesenchymal stem cells thwart pyroptosis of lung tissue cells in septic mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6642-6648. |
| [14] | Yu Qinghe, Cai Ziming, Wu Jintao, Ma Pengfei, Zhang Xin, Zhou Longqian, Wang Yakun, Lin Xiaoqin, Lin Wenping. Vanillic acid inhibits inflammatory response and extracellular matrix degradation of endplate chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6391-9397. |
| [15] | Fan Jiaxin, Jia Xiang, Xu Tianjie, Liu Kainan, Guo Xiaoling, Zhang Hui, Wang Qian . Metformin inhibits ferroptosis and improves cartilage damage in osteoarthritis model rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6398-6408. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||