Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (11): 2319-2326.doi: 10.12307/2025.355
Previous Articles Next Articles
Differences in dynamic stability across different height barriers between obese and average men
Zhang Wenli1, Zhao Ziqi1, Liang Leichao2, Tang Yunqi3, Wang Yong1
- 1School of Physical Education and Sport, Liaocheng University, Liaocheng 252000, Shandong Province, China; 2Shanghai University of Medicine & Health Sciences, Shanghai 201318, China; 3Shaanxi University of Science & Technology, Xi’an 710021, Shaanxi Province, China
-
Received:2024-03-19Accepted:2024-05-14Online:2025-04-18Published:2024-08-12 -
Contact:Wang Yong, PhD, Associate professor, School of Physical Education and Sport, Liaocheng University, Liaocheng 252000, Shandong Province, China -
About author:Zhang Wenli, Master, School of Physical Education and Sport, Liaocheng University, Liaocheng 252000, Shandong Province, China Zhao Ziqi, Master candidate, School of Physical Education and Sport, Liaocheng University, Liaocheng 252000, Shandong Province, China Zhang Wenli and Zhao Ziqi contributed equally to this work. -
Supported by:Humanities and Social Sciences Research Planning Fund Project of the Ministry of Education, No. 21YJCZH115 (to WY); Shandong Province Postgraduate Education Teaching Reform Research Project, No. SDYJG21196 (to WY)
CLC Number:
Cite this article
Zhang Wenli, Zhao Ziqi, Liang Leichao, Tang Yunqi, Wang Yong. Differences in dynamic stability across different height barriers between obese and average men[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2319-2326.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

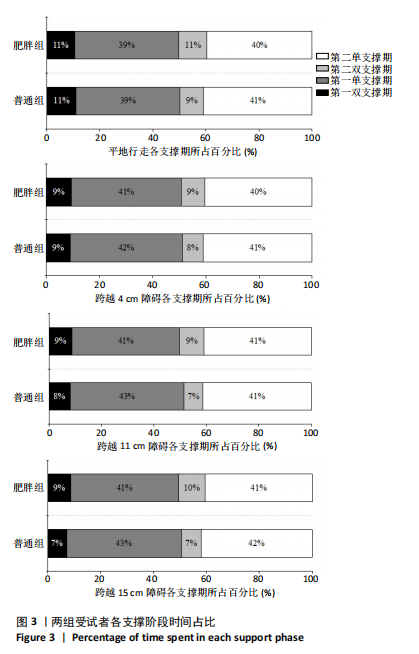
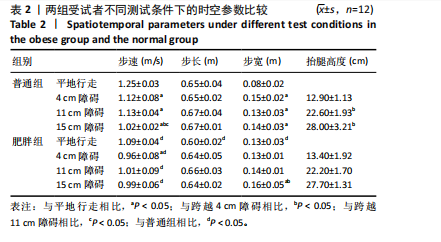
2.4 时空参数 双重复测量方差分析结果显示,障碍高度与组别交互作用对步速[F(3,33)=4.642,P=0.021]与步宽[F(3,33)=5.021,P=0.005]的影响显著,障碍高度与组别交互作用对步长[F(3,33)=1.071,P=0.372]与抬腿高度[F(3,33)=3.919,P=0.32]的影响不显著。遂对步速与步宽进行简单效应分析,对步长与抬腿高度进行主效应分析。 如表2所示,平地行走时,相较于普通组,肥胖组的步速降低(P < 0.001)、步长减小(P=0.015)、步宽增加(P=0.001);跨越4 cm障碍时,肥胖组的步速更低(P=0.001),步长(P=0.701)、步宽(P=0.051)与抬腿高度(P=0.057)均无显著性差异;跨越11 cm障碍时,肥胖组步速降低(P=0.004),步长(P=0.49)、抬腿高度(P=0.051)与步宽(P=0.202)均无显著性差异;跨越15 cm障碍时,肥胖组的步长减小(P=0.018),而步速(P=0.246)、抬腿高度(P=0.059)与步宽(P=0.384)无显著性差异。 普通组4项测试间的步速和步宽均有显著性差异(P < 0.001)。跨越障碍时的步速显著小于平地行走时(P < 0.001),而步宽则大于平地行走时(P < 0.001),同时跨越4 cm与11 cm障碍的步速要大于跨越15 cm障碍(P < 0.001)。 肥胖组4项测试间的步速(P=0.047)和步宽(P < 0.001)亦有显著性差异。相较于平地行走,跨越4 cm障碍时的步速降低(P=0.005),跨越15 cm障碍时的步宽增加(P=0.025)。"
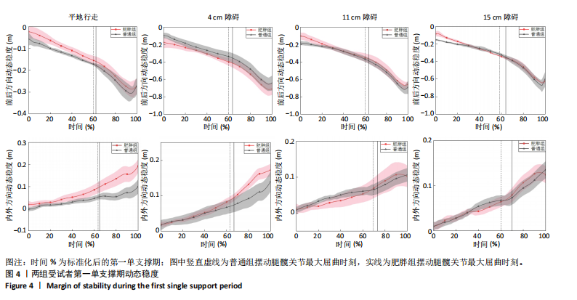
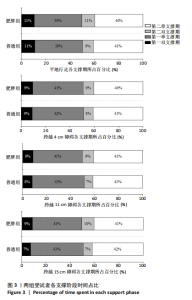
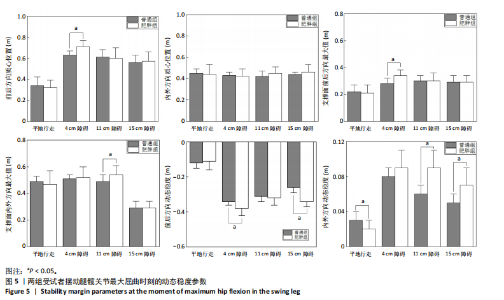
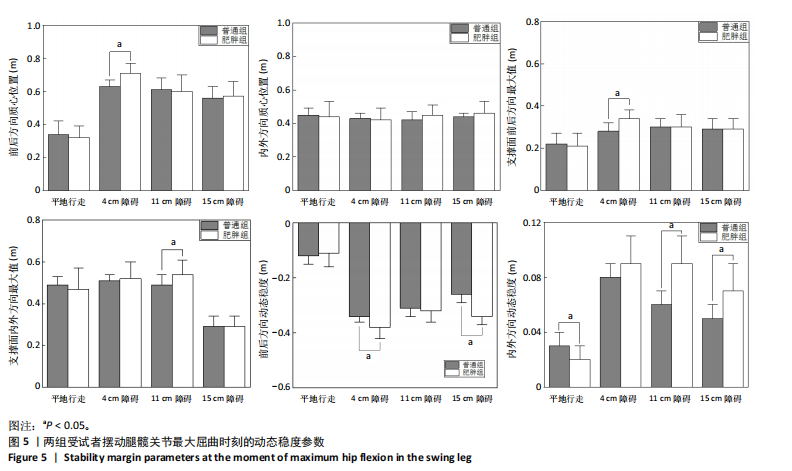
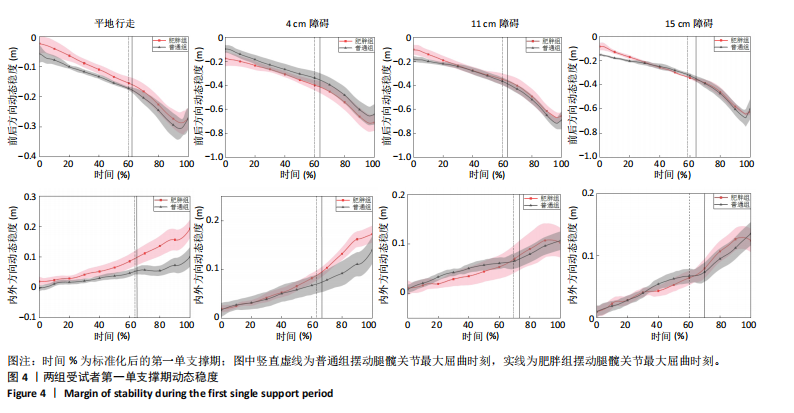
2.5 前后与内外方向动态稳度 如图4所示,普通组与肥胖组的前后与内外方向动态稳度变化趋势一致,但摆动腿髋关节屈曲时刻不同。平地行走与跨越4 cm障碍时,前后方向动态稳度为负值,且肥胖组大于普通组,在跨越11 cm与15 cm障碍时无明显变化;内外方向动态稳度为正值,肥胖组整体大于普通组,这一差异在摆动腿髋关节最大屈曲时刻之后更为显著。 2.6 摆动腿髋关节最大屈曲时刻的前后方向动态稳度 双因素重复测量方差分析结果显示,障碍高度与组别的交互作用对动态稳度的影响显著[F(3,33)=4.172,P=0.028],遂进行简单效应分析。 如图5所示,在平地行走时,肥胖组与普通组在前后方向的动态稳度无显著性差异(P=0.518);在跨越4 cm障碍时,肥胖组在前后方向的动态稳度低于普通"

组(P=0.027);在跨越11 cm障碍时,两组在前-后方向的动态稳度无显著性差异(P=0.705);在跨越15 cm障碍时,两组在前-后方向的动态稳度差异有显著性意义(P < 0.001)。 肥胖组4项测试的前后方向动态稳度表现出显著性差异(P < 0.001)。肥胖组在跨越4 cm障碍时,与跨越15 cm障碍比较,前后侧动态稳度无显著性差异(P=0.21),与平地行走(P < 0.001)和跨越11 cm障碍(P=0.002)之间差异有显著性意义;肥胖组在跨越11 cm障碍时,与跨越15 cm障碍比较,前后侧动态稳度无显著性差异(P=0.862),与其他两项测试比较,则表现出显著性差异(P平地行走< 0.001,P4 cm障碍=0.003);肥胖组在跨越15 cm障碍时,与平地行走比较,前后侧动态稳度表现出显著性差异(P < 0.001),与其他两项测试之间差异无显著性(P4 cm障碍= 0.21,P11 cm障碍=0.862)。 普通组4项测试之间动态稳度存在显著性差异(P < 0.001);普通组在跨越4 cm障碍时,与跨越11 cm障碍比较,前后方向动态稳度无显著性差异(P=0.234),与其他两项测试之间则表现出显著性差异(P平地行走< 0.001,P15 cm障碍= 0.003);普通组在跨越11 cm障碍时,与平地行走比较,前后侧动态稳度无显著性差异(P=0.234),与其他两项测试间均有显著性差异(P4 cm障碍< 0.001,P15 cm障碍< 0.001);普通组在跨越15 cm障碍时,前后方向动态稳度大于平地行走时(P < 0.001),小于跨越4 cm障碍时(P=0.003),但与跨越11 cm障碍间无显著性差异(P=0.27)。 2.7 摆动腿髋关节最大屈曲时刻的内外方向动态稳度 双因素重复测量方差分析结果显示,障碍高度与组别的交互作用对动态稳度的影响不显著[F(3,33)=3.025,P=0.053],遂进行主体内效应分析。 如图5所示,在不同步行模式下,两组内外方向动态稳度均为正值。但肥胖组平地行走(P=0.039)、跨越11 cm障碍(P=0.004)、跨越15 cm障碍(P=0.032)时与普通组对比表现出显著性差异。 平地行走与跨越3个高度障碍对比,内外方向动态稳度表现出显著性差异(P4 cm障碍< 0.001,P11 cm障碍< 0.001,P15 cm障碍< 0.001);跨越4 cm障碍与跨越11 cm障碍、15 cm障碍间均无显著性差异(P11 cm障碍=0.935,P15 cm障碍= 0.069),跨越11 cm障碍与15 cm障碍间亦无显著性差异(P=0.564)。 2.8 不良事件 试验过程中24名受试者均未发生不良事件。"

| [1] 黄守清, 许艺惠, 尹莲花. 414例不同年龄男女间平衡能力及身体质量指数的差异分析[J]. 山东体育科技,2016,38(2):52-55. [2] MACIE A, MATSON T, SCHINKEL-IVY A. Age affects the relationships between kinematics and postural stability during gait. Gait Posture. 2023;102:86-92. [3] HARRISON K, KWON YU, SIMA A, et al. Inter-joint coordination patterns differ between younger and older runners. Hum Mov Sci. 2019;64: 164-170. [4] HATZITAKI V, AMIRIDIS IG, ARABATZI F. Aging effects on postural responses to self-imposed balance perturbations. Gait Posture. 2005;22(3):250-257. [5] 张阳, 严凤清, 郭小莉, 等. BMI和性别对大学生静动态平衡能力影响的研究[J]. 吉林体育学院学报,2021,37(5):83-87. [6] 曾玉冰. 男性肥胖大学生步行与慢跑步态特征分析[D]. 大连: 大连理工大学,2021. [7] CHARDON M, BARBIERI F A, PENEDO T, et al. The effects of experimentally-induced fatigue on gait parameters during obstacle crossing: A systematic review. Neurosci Biobehav Rev. 2022;142: 104854. [8] CHO H, HEIJNEN MJ, CRAIG BA, et al. Falls in young adults: The effects of sex, physical activity, and prescription medications. PLOS One. 2021;16(4):e0250360. [9] STRUBHAR AJ, PETERSON ML, ASCHWEGE J. The effect of text messaging on reactive balance and the temporal and spatial characteristics of gait. Gait Posture. 2015;42(4):580-583. [10] SONG Q, ZHOU J, SUN W, et al. Long-term tai chi exercise increases body stability of the elderly during stair ascent under high and low illumination. Sports Biomech. 2018;17(3):402-413. [11] MIAN OS, NARICI MV, MINETTI AE, et al. Centre of mass motion during stair negotiation in young and older men. Gait Posture. 2007;26(3): 463-469. [12] NOVAK A, BROUWER B. Sagittal and frontal lower limb joint moments during stair ascent and descent in young and older adults. Gait Posture. 2011;33(1):54-60. [13] GONCALVES G, SELISTRE L, PETRELLA M, et al. Kinematic alterations of the lower limbs and pelvis during an ascending stairs task are associated with the degree of knee osteoarthritis severity. Knee. 2017; 24(2):295-304. [14] QU X, HU X. Lower-extremity kinematics and postural stability during stair negotiation: Effects of two cognitive tasks. Clin Biomech. 2014; 29(1):40-46. [15] HOF AL, GAZENDAM MG, SINKE WE. The condition for dynamic stability. J Biomech. 2005;38(1):1-8. [16] GILL SV, HUNG YC. Effects of overweight and obese body mass on motor planning and motor skills during obstacle crossing in children. Res Dev Disabil. 2014;35(1):46-53. [17] 郑慧芬, 孙威, 宋祺鹏, 等. 手机任务介入对下楼梯行走动态稳定性的影响[J]. 中国运动医学杂志,2021,40(7):528-535 [18] 黄尚军, 伍勰, 黄睿, 等. 脑卒中伴随膝伸肌痉挛者跨越障碍的运动控制策略研究[J]. 医用生物力学,2021,36(S1):201. [19] 陈岩, 孙威, 马腾, 等. 有跌倒史老年人跨越障碍步态特征的研究[J]. 山东体育学院学报,2014,30(5):62-64. [20] 孟站领, 张庆来, 苑玲伟, 等. 不同跌倒风险老年人跨越障碍前后足底压力特征[J]. 医用生物力学,2022,37(4):741-747. [21] KIM D, LEWIS CL, GILL SV. The effect of obesity on whole-body angular momentum during steady-state walking. Gait Posture. 2022;94: 93-101. [22] LEWINSON RT, MADDEN R, KILLICK A, et al. Foot structure and knee joint kinetics during walking with and without wedged footwear insoles. J Biomech. 2018;73:192-200. [23] BLOEM BR, GRIMBERGEN YA, VAN DIJK JG, et al. The” posture second” strategy: A review of wrong priorities in parkinson’s disease. J Neurol Sci. 2006;248(1):196-204. [24] 王莉, 于卫华, 徐忠梅. 社区老年人双重任务行走步态特征与跌倒的关系研究[J]. 护理学杂志,2016,15(1):76-79. [25] 杨凤娇, 王芗斌, 侯美金, 等. 三维步态分析比较青年人与老年人双任务下步态特征的差异[J]. 中国组织工程研究,2021,25(3):344-349. [26] LEE HJ, CHOU LS. Balance control during stair negotiation in older adults. J Biomech. 2007;40(11):2530-2536. [27] 梁雷超, 黄灵燕, 伍勰, 等. 膝骨关节炎对女性老年人步行动态稳定性的影响[J]. 体育科学,2016,36(3):61-66. [28] PEEBLES AT, REINHOLDT A, BRUETSCH AP, et al. Dynamic margin of stability during gait is altered in persons with multiple sclerosis. J Biomech.2016;49(16):3949-3955. [29] HINMAN RS, BENNELL KL, METCALF BR, et al. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology. 2002;41(12):1388-1394. [30] MCANDREW YP, DINGWELL J. Voluntary changes in step width and step length during human walking affect dynamic margins of stability. Gait Posture. 2012;36(2):219-224. [31] ARAMPATZIS A, KARAMANIDIS K, MADEMLI L. Deficits in the way to achieve balance related to mechanisms of dynamic stability control in the elderly. J Biomech. 2008;41(8):1754-1761. [32] 曾照宏, 薛奥传, 王会会, 等. 肥胖大学生膝关节肌力特征及动态平衡的关系[J]. 体育科技文献通报,2022,30(9):120-123. [33] BOEKA AG, LOKKEN KL. Neuropsychological performance of a clinical sample of extremely obese individuals. Arch Clin Neuropsych. 2008; 23(4):467-474. [34] DIAMOND A, LEE K. Interventions shown to aid executive function development in children 4–12 years old. Science. 2011;333(6045): 959-964. [35] GREVE J, ALONSO A, BORDINI AC, et al. Correlation between body mass index and postural balance. Clinics (Sao Paulo). 2007;62(6):717-720. [36] GILL SV, HUNG YC. Influence of weight classification on children stepping over obstacles. Am J Phys Med Rehabil. 2012;91(7):625-630. [37] LIU ZQ, YANG F. Obesity may not induce dynamic stability disadvantage during overground walking among young adults. PLOS ONE. 2017; 12(1): e0169766. [38] ESPY DD, YANG F, BHATT T, et al. Independent influence of gait speed and step length on stability and fall risk. Gait Posture. 2010;32(3): 378-382. [39] CURTZE C, BUURKE TJW, MCCRUM C. Notes on the margin of stability. J Biomech. 2024;166:112045. [40] DONELAN J, KRAM R, KUO A. Mechanical and metabolic determinants of the preferred step width in human walking. Proc Biol Sci. 2001; 268(1480):1985-1992. [41] HERSSENS N, CRIEKINGE TV, SAEYS W, et al. An investigation of the spatio-temporal parameters of gait and margins of stability throughout adulthood. J R Soc Interface. 2020;17(166):20200194. [42] FORNER CORDERO A, KOOPMAN HF, VAN DER HELM FC. Multiple-step strategies to recover from stumbling perturbations. Gait Posture. 2003; 18(1):47-59. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [3] | Zhu Xiaoxue, Zhao Qiongqiu, Zhang Teng, Wang Dan, Qiu Jihong, Song Qipeng, Shen Peixin. Increasing toe-out angle during drop-landing can diminish risk of inversion injuries among individuals with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1827-1833. |
| [4] | Zhang Xinxin, Gao Ke, Xie Shidong, Tuo Haowen, Jing Feiyue, Liu Weiguo. Network meta-analysis of non-surgical treatments for foot and ankle ability and dynamic balance in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1931-1944. |
| [5] | Zhang Yuxin, Yu Cong, Zhang Cui, Ding Jianjun, Chen Yan. Differences in postural control ability between older adults with mild cognitive impairment and those with normal cognition under different single-task and dual-task conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1643-1649. |
| [6] |
Liang Xiaoxiao, Zheng Jiejiao, Duan Linru, Chen Xi, Zhang Tingyu.
Characterization of postural stability in elderly patients with idiopathic normal pressure hydrocephalus #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1208-1213.
|
| [7] | Wu Yihan, Liu Zhongqiang, Wei Qiaoye, Liu Mingdong, Chen Keyi, Li Zhigang. Effect of balance training with different visual conditions on proprioception in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1050-1057. |
| [8] | Li Jing, Lu Guangqi, Zhuang Minghui, Cui Ying, Yu Zhangjingze, Sun Xinyue, Ma Mingming, Zhu Liguo, Yu Jie. Development of a clinical prediction model for cervical instability in young and middle-aged adults based on machine learning [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7203-7210. |
| [9] | Guo Ping, Wang Juan. Bilateral lower limb biomechanical abnormalities in patients with unilateral chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6920-6926. |
| [10] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [11] | Wang Zilong, Meng Xin, Zhang Zhiqi, Xie Yu, Meng Lingyue, Zhang Qiuxia, Kong Lingyu. Biomechanical characteristics of lower extremities during counter movement jump in male patients with functional ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 478-485. |
| [12] | Zheng Xiang, Zhang Mingxing, Huang Ya, Shan Sharui. Improvement of lower limb walking function in patients with chronic non-specific low back pain by biofeedback assisted electrical stimulation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 547-553. |
| [13] | Muzaipaer · Maitusong, Xiao Yang, Gulimire · Adili, Zhigeer · Lehalebieke, Aizihaier · Aisikaer, Wang Yixi, Chen Ruilin, Paerhati · Rexiti, , . Biomechanical performance of novel fully cortical bone threaded screws in modified cortical bone trajectory screw technique for lumbar vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5765-5772. |
| [14] | Zhu Tianrui, Shi Jipeng, Sun Jiahe, Wang Luyi, Zhang Chen, Xu Hongqi, Quan Helong. Effectiveness of different exercise regimens to reduce fall risks in older adults: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5662-5672. |
| [15] | Wang Xia, Xue Boshi, Yang Chen, Zhou Zhipeng, Zheng Liangliang. Influence of neuromuscular function on the risk of biomechanical injury in landing manoeuvres in patients undergoing anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5556-5562. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||