[1] TINS BJ, BALAIN B.Incidence of numerical variants and transitional lumbosacral vertebrae on whole-spine MRI.Insights into Imaging.2016; 7(2):199-203.
[2] GOPALAN B, YERRAMSHETTY JS.Lumbosacral Transitional Vertebra-Related Low Back Pain: Resolving the Controversy.Asian Spine J. 2018;12(3):407-415.
[3] LIAN J, LEVINE N, CHO W.A review of lumbosacral transitional vertebrae and associated vertebral numeration. Eur Spine J. 2018; 27(5):995-1004.
[4] SHAIKH A, KHAN SA, HUSSAIN M, et al.Prevalence of Lumbosacral Transitional Vertebra in Individuals with Low Back Pain: Evaluation Using Plain Radiography and Magnetic Resonance Imaging.Asian Spine J. 2017;11(6):892-897.
[5] CARRINO JA, CAMPBELL PD JR, LIN DC, et al.Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology.2011;259(1):196-202.
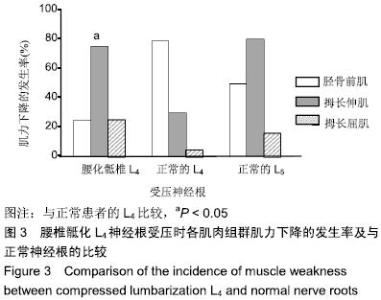
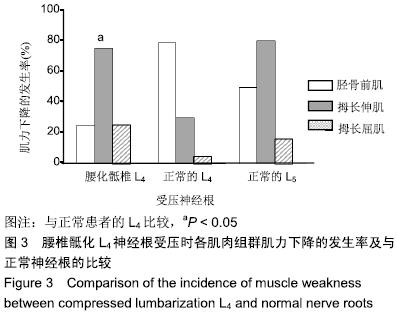
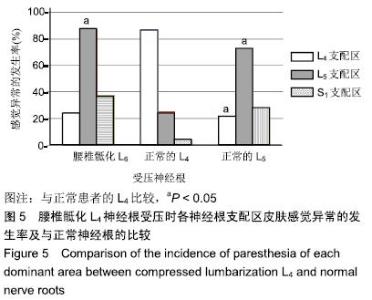
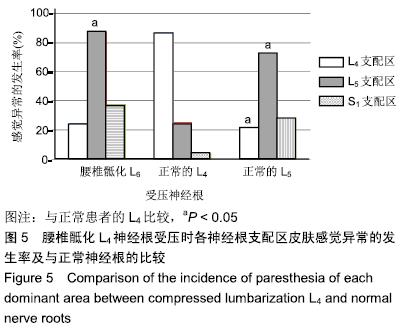
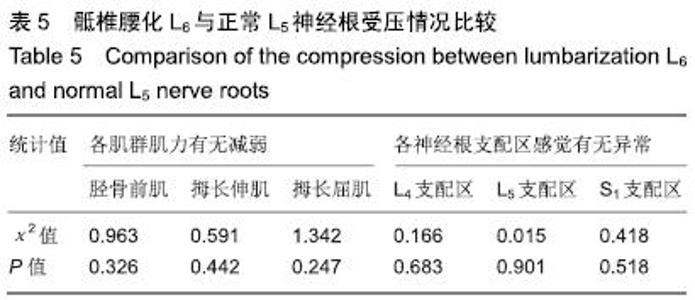
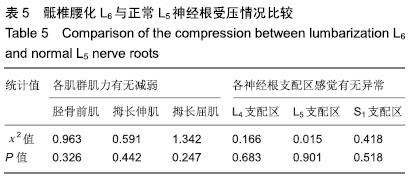
[6] CHANG HS, NAKAGAWA H.Altered function of lumbar nerve roots in patients with transitional lumbosacral vertebrae.Spine (Phila Pa 1976). 2004;29(15):1632-5; discussion 1635.
[7] NEVALAINEN MT, MCCARTHY E, MORRISON WB, et al. Lumbosacral transitional vertebrae: significance of local bone marrow edema at the transverse processes.Skeletal Radiol. 2018;47(8): 1145-1149.
[8] DE BRUIN F, TER HORST S, BLOEM JL, et al.Prevalence and clinical significance of lumbosacral transitional vertebra (LSTV) in a young back pain population with suspected axial spondyloarthritis: results of the SPondyloArthritis Caught Early (SPACE) cohort.Skeletal Radiol. 2017;46(5):633-639.
[9] OTANI K, KONNO S, KIKUCHI S. Lumbosacral transitional vertebrae and nerve-root symptoms.J Bone Joint Surg Br. 2001;83(8):1137-1140.
[10] SUZUKI N.An anatomical study of the root sleeve emergence and its relation to segmental anomalies of the lumbo-sacral spine. Nihon Seikeigeka Gakkai Zasshi. 1987;61(12):1379-1387.
[11] MCCULLOCH JA, WADDELL G.Variation of the lumbosacral myotomes with bony segmental anomalies. J Bone Joint Surg Br.1980; 62-B(4):475-480.
[12] 侯黎升,崔洪鹏,阮狄克,等. 腰骶移行椎患者腰骶神经根支配区域变化的临床研究[J].中国临床解剖学杂志, 2010,28(6):663-667.
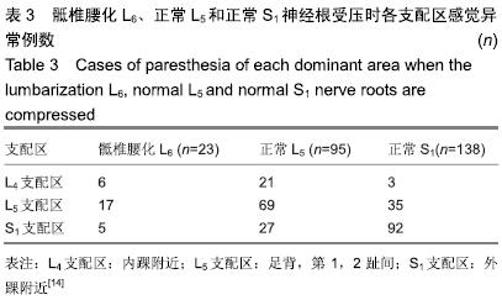
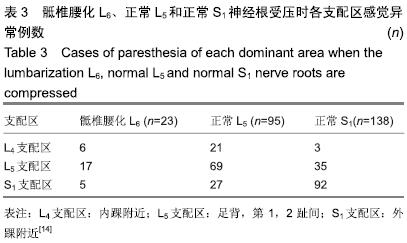
[13] Kim YH, Lee PB, Lee CJ, et al.Dermatome variation of lumbosacral nerve roots in patients with transitional lumbosacral vertebrae.Anesth Analg. 2008;106(4):1279-1283.
[14] 田伟.实用骨科学[M].北京:人民卫生出版社, 2016.
[15] TINS BJ, BALAIN B.Incidence of numerical variants and transitional lumbosacral vertebrae on whole-spine MRI.Insights into Imaging.2016; 7(2):199-203.
[16] CASTELLVI AE, GOLDSTEIN LA, CHAN DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects.Spine (Phila Pa 1976).1984;9(5):493-495.
[17] 刘淼,王振汉.腰骶部神经根解剖变异所致神经根症状的多变性[J].中华骨科杂志,1994,14(4):230-232.
[18] PATERSON AM. The Origin and Distribution of the Nerves to the Lower Limb.J Anat Physiol. 1894;28(Pt 2):169-193.
[19] KIKUCHI S, HASUE M, NISHIYAMA K, et al.Anatomic features of the furcal nerve and its clinical significance.Spine (Phila Pa 1976).1986; 11(10):1002-1007.
[20] HARSHAVARDHANA NS, DABKE HV.The furcal nerve revisited. Orthop Rev (Pavia). 2014;6(3):5428.
[21] Anetai H, Tokita K, Kojima R, et al.Variations in the course of the superior gluteal artery in relation to the lumbosacral plexus.Okajimas Folia Anat Jpn. 2017;94(2):45-54.
[22] 朱爱国,张烽,朱建炜,等.腰骶丛神经根的应用解剖及临床意义[J].中国组织工程研究, 2019,23(4):573-577.
[23] 吕亚萍,林薇,马雪梅.髂腰韧带在腰椎节段数中的定位[J]. 放射学实践, 2016,31(11):1080-1083.
[24] 鲍立杰,吴培斌,张志平.胸、腰椎手术术前定位方法的研究进展[J].实用临床医学, 2014,15(12):133-135.
[25] TOKGOZ N, UCAR M, ERDOGAN AB, et al.Are Spinal or Paraspinal Anatomic Markers Helpful for Vertebral Numbering and Diagnosing Lumbosacral Transitional Vertebrae?.Korean J Radiol. 2014;15(2): 258-266.
[26] LEE CH, SEO BK, CHOI YC, et al.Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments.AJR Am J Roentgenol.2004;182(5):1295-1300.
[27] CHAKRAVERTY R, PYNSENT P, ISAACS K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines?. J Anat. 2007;210(2):232-236.
|